Excretory System (pg 378)
advertisement

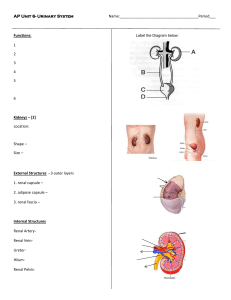
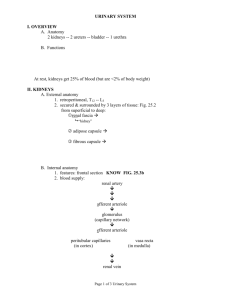
Excretory System (pg 378) Maintain equilibrium by eliminating waste Lungs-CO2, H2O, heat (breath) Skin-H2O, salt, heat (sweat) Large intestines- indigestible materials (feces) Liver-toxins, heavy metals (urine) Kidneys- urea, uric acid (urine) Urinary System Maintains water balance, ion balance and eliminates metabolic wastes Metabolic wastes are byproducts of cellular respiration that have been converted to toxins by the liver Ammonia (NH3) VERY TOXIC must convert to urea Urea (blood to kidneys) Uric acid (blood to kidneys) Regulates the composition of blood Principle Structures Renal Artery/Renal Vein Ureter Urinary Bladder Urethra Kidneys Nephron Renal Artery/Renal Vein Renal Artery-Branches from the aorta to carry blood to kidneys to be cleaned Renal Vein-Joins with inferior vena cava to carry cleaned blood back to heart Ureter Tubes which carry urine from kidneys to urinary bladder Lined with cells that secrete mucus to protect walls Outside walls are smooth muscle for peristalsis Urinary Bladder Temporary storage of urine by muscular organ behind pubic bone Empty looks like a deflated balloon Full about the size of a pear 2 rings of muscle at junction Internal sphincter-involuntary External sphincter- voluntary 200-400ml max vol over 600ml control is lost 1.5 L empties in 24 hours Urethra Tube from bladder to exterior of body Longer in males Shorter in females Kidneys (pg 379) 2 half kilogram fist sized on either side of the spine on the back wall of the ab. cavity May hold up to ¼ of body’s blood Filters waste from blood and produces urine 3 layers Outer connective tissue-renal cortex Inner connective tissue-renal medulla Inner hollow chamber –renal pelvis Nephron Functional part of the kidney Approx 1 million slender tubules partly in cortex and partly in medulla Parts of the Nephron that carry blood Renal Artery Afferent arterioles Glomerulus Efferent arterioles Peritubular capillaries-wrap around the kidney tubule Renal vein Parts that carry “urine” Bowman’s capsule Proximal tubule Loop of henle Distal tubule Collecting ducts Nephron Functional Regions A Filter A Tubule A Duct A Filter Filtration structure at top of each nephron is Bowman’s capsule Renal artery enters and splits into glomerulus Walls of glomerulus act as a filter impermeable to proteins, large molecules and red blood cells Permeable to water, small molecules, ions and urea Filtered fluid that leaves glomerulus and enters Bowmans capsule is called filtrate A Tubule Bowman’s capsule connects to small long narrow tube that is twisted back on itself to form a loop This loop is a reabsorption device and has three sections: proximal (nearby) tubule, loop of Henle, distal (distant) tubule Tubule absorbs substances that are useful to body (glucose, ions) from filtrate and secretes substances into surrounding tissue A Duct Tubule empties into larger channel called the collecting duct Collecting duct reclaims water from filtrate Filtrate that remains in collecting duct is now called urine Solids and water reclaimed during reabsorption returned to body via renal veins Formation of Urine Glomerular filtration 1. Movement of water and solutes from blood into nephron Tubular reabsorption 2. Transfer essential solutes from nephron back into blood Tubular secretion 3. Transport of additional waste materials from blood into nephron filtrate Water reabsorption 4. Removes water from filtrate and returns it to blood Glomerular Filtration Process that forces waste from blood plasma into Bowman’s capsule Filtrate is identical to blood plasma minus proteins and blood cells Plasma protein, blood cells, platelets are too large to move through Water, sodium chloride, glucose, amino acids, H ions, urea are small enough to move through Tubular Reabsorption Proximal Tubule Mitochondria in walls use ATP for active transport of nutrients (Na+, glucose, amino acids, K+) back into blood Negatively charged ions (Cl-) tag along passively, attracted by electrical charge on transported ions Water follows by osmosis Tubular Reabsorption Loop of Henle Reabsorb water and ions from filtrate Permeability of loop changes and water is reabsorbed on the descending side and sodium ions reabsorbed on the ascending side Tubular Reabsorption & Secretion Distal Tubule (under control of hormones) Active reabsorption of sodium depends on needs of body Passive reabsorption of negative ions like chloride because of attraction Decreases concentration of filtrate so water reabsorbed by osmosis Potassium and hydrogen (pH regulation) is actively secreted back into nephron Other substances not normally part of body also secreted Water Reabsorption Collecting Duct Filtrate still contains lots of water Passive reabsorption of water from filtrate by osmosis Permeability to water will depend on body conditions Filtrate is 4x more concentrated by the time it leaves duct and is approx 1% of original filtrate volume now its called urine Maintaining the Excretory system Water regulation (osmoregulation) Blood pressure regulation Water regulation Decrease of H2O in blood More H2O moves from cells to blood increasing the osmotic pressure Cells shrink Osmoreceptors located detect pressure change in blood Triggers thirst and the release of ADH ADH (antidiuretic hormone)moves to distal tubule and collecting duct to make them more permeable to water which will increase reabsorption into blood More water in blood means more water to the cells returning the osmotic pressure to normal Negative feedback loop Drinking Change in osmotic pressure Cells shrink Release of ADH to encourage reabsorption Blood Pressure Regulation Blood volume influences blood pressure Kidneys also play a role by adjusting blood volume Blood pressure receptors near glomerulus called detect low pressure Release enzyme rennin which activates angiotensin Angiotensin constricts blood vessels and initiates release of aldosterone produced in adrenal gland above kidney travels to kidney to act on distal tube and collecting duct to increase sodium transport which causes fluid level to increase Increase fluid level means higher blood voluem therefore pressure change Negative Feedback loop Constrict blood vessels Change in blood pressure Renin initiates activation of Angiotensin Release of Aldosterone Increase in NaCl reabsorption and Fluid level in body increases Disorders of Urinary System Diabetes mellitus Diabetes insipidus Bright’s Disease Kidney Stones Gout Nephrosis Toxemia