MLAB 2401: Clinical Chemistry Keri Brophy
advertisement

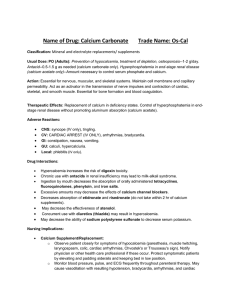
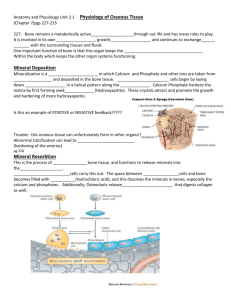
MLAB 2401: Clinical Chemistry Keri Brophy-Martinez Overview: Mineral and Bone Metabolism Calcium Homeostasis Organs involved ◦ Small intestine ◦ Skeleton Hydroxyapatite ( calcium+ phosphorus+ hydroxide) ◦ Kidneys Origin ◦ Diet Reservoir ◦ Bone Forms of Calcium Bound to albumin–45% ◦ Reversible process ◦ Binding is pH dependent Free “ionized”–50% Complexes with anions -5% Ionized Calcium Free calcium in blood Tightly regulated Biologically active form Advantage ◦ Not associated with proteins or anions Functions of Calcium Nerve impulse transmission Cofactor in certain enzymes Coagulation of blood Skeletal mineralization Preservation of cell membrane integrity and permeability Regulation of Calcium Homeostasis Parathyroid hormone- PTH Vitamin D3 Calcitonin Parathyroid Hormone- PTH Originates from the parathyroid gland Secretion based on levels of free calcium Activities/Roles ◦ Stimulation of osteoclastic bone reabsorption and release of calcium and phosphate from bone ◦ Stimulation of calcium reabsorption and inhibition of phosphate reabsorption from the renal tubules ◦ Stimulation of renal production of 1,25(OH)2 vitamin D3, which increase intestinal absorption of calcium and phosphate Regulation of Calcium Homeostasis Vitamin D3/ Cholecalciferol Synthesis occurs in skin, liver, kidneys Affects gut, bone, and parathyroid Actions/ Roles ◦ Increases plasma calcium and phosphate concentration by increasing the absorption of calcium and phosphate from the gastrointestinal tract ◦ Increases bone resorption and enhances the effects of PTH in the nephron to promote renal tubular calcium reabsorption ◦ Stimulates osteoclasts to metabolize bone calcium Vitamin D: Where Does it Come From? Sources of: ◦ Diet Animal tissues and products ( liver) Irradiated milk ◦ Sunlight Calcitonin Secreted by the thyroid gland Secreted when blood calcium rises Inhibits PTH and Vitamin D Inhibits bone resorption, promotes bone formation Phosphorous Origin ◦ Diet ◦ Bone ◦ Phosphate ion is distributed equally. Intracellular Component of macromolecules Extracellular Inverse relationship with Calcium Functions of Phosphorous Component of bones & teeth Essential part of cell membranes Contributes to enzyme function Storage and transfer of energy Component of many compounds Phosphorous Regulation Kidneys ◦ Excrete or reabsorb Other factors ◦ PTH Increases renal excretion ◦ Vitamin D increases levels Phosphate absorption in intestine Phosphate reabsorption in kidneys ◦ Growth Hormone, calcitonin, acid-base status Magnesium 2nd most abundant intracellular cation Location ◦ 50-60% found in bone ◦ 40-50% muscle & soft tissue ◦ 1% in the RBC Origin ◦ Diet Nuts, hard water, meat, green vegetables, fish, dry cereal Forms of Magnesium Free or ionized (~55%) Bound to proteins (~30%) Complexed with phosphate, citrate and other ions (~15%) Functions of Magnesium Important co-factor in reactions using ATP ◦ Carbohydrate metabolism ◦ Muscle contraction ◦ Blood coagulation Membrane stabilization Nerve conduction Maintenance of potassium Magnesium Regulation Primary regulatory factor ◦ Amount of magnesium in the plasma Regulatory control ◦ Kidney Excrete or reabsorb magnesium depending on condition ◦ Parathyroid hormone Increases renal reabsorption Enhances absorption in intestines References Bishop, M., Fody, E., & Schoeff, l. (2010). Clinical Chemistry: Techniques, principles, Correlations. Baltimore: Wolters Kluwer Lippincott Williams & Wilkins. http://rickets.stanford.edu/ http://scrink.com/blog/wellness/2009/02/vitamin-d-coldflu-correlation.html Sunheimer, R., & Graves, L. (2010). Clinical Laboratory Chemistry. Upper Saddle River: Pearson .



![2012 [1] Rajika L Dewasurendra, Prapat Suriyaphol, Sumadhya D](http://s3.studylib.net/store/data/006619083_1-f93216c6817d37213cca750ca3003423-300x300.png)