minerals
advertisement

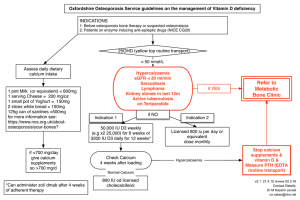
minerals GANESH DHAKAL PG MED. BIOCHEMISTRY J.N.MEDICAL COLLEGE Definitions & Types • Minerals are essential for the normal growth and maintenance of the body. • Macro minerals (more than 100 mg/day). • Micro minerals also known as trace elements (less than 100 mg/day) Important minerals • Major elements; calcium, magnesium, phosphorus, sodium, potassium, chloride, sulphur. • Trace elements; Iron, iodine copper, manganese, zinc, molybdenum, selenium, fluoride. Biological role of minerals • Structural components of bone and teeth; calcium, p, mg,f. • Structural components of soft tissues such as liver, muscle, nerve cells: p,k,fe,s etc. • Fluid balance: Na, k,cl etc. • Acid base balance: Na, p. • Nerve cell transmission and muscle contraction: Exchange of Na & k. helps NT and Ca helps MC. • Blood coagulation: Ca Thyroid Hormone activity: Iodine. Vit.B12 : cobalt Hb &Heme containing compounds: Iron. CALCIUM • Total calcium in the body is about 1-1.5 kg. • 99% seen in bone and 1% in ECF. Daily req.:500 mg/day child:1200mg/day Source: milk good source egg, fish and veg. medium source cereals contain small amount. Absorption • Absorption: first and second part of duodenum against a conc. Gradient. And req. energy. • Factors causing increased absorption: Vit D, PTH, Acidity, lysine and arginine. • Factors causing decreased absorption: Phytic acid(cereals),oxalates(lefty vegetables) malabsorption syndromes, high phosphate. Role of calcium • • • • • • • • Muscles contraction Nerve conduction Coagulation Secretion of hormones(calcitonin, ADH, PTH) Secondary messenger(glucagon) Activation of enzymes (Pyruvatekinase, lipase) Prolongs systole Bone & teeth formation. Calpains • Family of calcium-dependent,cysteine proteases(proteolytic enzymes). • Seen ubiquitously in mammals. • Calpain I & calpain II isoforms share small(30k) subunit, large (80k) subunit. Role: cell mobility, cell cycle progression, potentiation in neurons and cell fusion in myoblasts. • Hyperactivity of calpain :Alzheimer’s dzs cataract formation myocardial ischemia cerebral ischemia. NOTE: Increase in conc. Calcium in all cell results in calpain activation, which lead to unregulated proteolysis and result irreversible tissue damage . Blood calcium level • Normal blood level: 9-11 mg% • 10mg% of ca++=5mEq/L) • Ionized calcium: about 5 mg% • Protein bound calcium: about 4 mg% Factors regulating blood calcium level Calcium homeostasis • There are effective controls to maintain this narrow range of blood calcium (9-11 mg/dl). • Vitamin D(calcitriol). • Parathyroid Hormone(PTH) • Calcitonin. • Vitamin D: It has hypercalcemic effect. It increases the blood calcium level. It has three major independent sites of action: Intestine, kidney bones. A. Vitamin D and Absorption of Calcium • Calcitriol promotes the absorption of calcium and • phosphorus from the intestine. • In the brush-border surface, calcium is absorbed passively. From the intestinal cell to blood, absorption of calcium needs energy. It is either by the sodium-calcium exchange mechanism or by pumping out the calcium-calbind incomplex. Calcitriol acts like a steroid hormone. • It enters the target cell and binds to a cytoplasmic • receptor. • The hormone-receptor complex interacts • with DNA and causes derepression and consequent • transcription of specific genes that code for • Calbindin . Due to the increased • availability of calcium binding protein, the absorption of calcium is increased. B. Effect of Vitamin D in Bone • Mineralization of the bone is increased by • increasing the activity of osteoblasts. • Calcitriol coordinates the remodelling action of • osteoclasts and osteoblasts. • It produces the differentiation of osteoclast precursors from multinucleated cells of osteoblast lineage. • Calcitriol stimulates osteoblasts which secrete alkaline • phosphatase. Due to this enzyme, the local • concentration of phosphate is increased. • The ionic product of calcium and phosphorus increases, leading to mineralization C. Effect of Vitamin D in Renal Tubules • Calcitriol increases the reabsorption of calcium and phosphorus by renal tubules, therefore both minerals are conserved. D. Regulation of Calcitriol • The hormonal level of calcitriol is maintained by the feed back control. • The rate of production is modulated by serum • levels of calcium, phosphorus, PTH and calcitriol itself. • The major site of control is on the 1-alphahydroxylase of kidney. • Hypercalcemia decreases calcitriol. • Low dietary calcium and hypocalcemia increase the rate of production of 1,25-DHCC. • The stimulatory effect of hypocalcemia on 1alpha hydroxylaseis through PTH. • Hypercalcemia decreases calcitriol. • The half-life of 1, 25-DHCC is 6-8 hours. • Parathyroid hormone (PTH): • It has a hypercalcemic hormone. • It has three major sites of action: Intestine Kidney Bones Mechanism of Action of PTH • • • • PTH binds with a receptor protein (Mol. wt. 70,000 Daltons) on the surface of target cells. This activates adenyl cyclase with consequent increase in intracellular calcium concentration. A kinase is activated and enzyme systems are activated. • The PTH has three major independent sites of action; bone kidney and intestine PTH and bones: causes • In the bone, PTH cause demineralization or decalcification • It induces pyrophosphatase in the osteoclasts. • The numbers of osteoclasts are also increased. • Osteoclasts release lactate into surrounding medium which solubilizes calcium. PTH also causes secretion of collagenase from osteoclasts. • This causes loss of matrix and bone resorption. • As a consequence, mucopolysaccharidesand hydroxyproline are excreted in urine. PTH and kidney • : In kidney, PTH causes • decreased renal excretion of calcium and • increased excretion of phosphates. The action is mainly through increase in reabsorption of calcium from kidney tubules • PTH and intestines: PTH stimulates 1hydroxylation • of 25-hydroxycalciferol in kidney to • produce calcitriol. This indirectly increases • calcium absorption from intestine. • Calcitonin: • Secreated by parafollicular cells of thyroid gland. • Tumor marker . • It is hypocalcemic hormone,which decreases the blood calcium level. • Site of Action; Kidney and bone • Calcitonin level is increased in medullary carcinoma of thyroid and therefore, is a tumor marker. • The level is also increased in multiple endocrine neoplasia (MEN). Hypercalcitoninemia • may also result from ectopic calcitonin production from malignant tumors of the lung and bronchus. • • • • • Calcitonin decreases serum calcium level. It inhibits resorption of bone. It decreases the activity of osteoclasts and increases that of osteoblasts. Calcitonin and PTH are directly antagonistic. Calcitonin,Calcitriol &PTH Act Together • When blood level calcium tends to lower, PTH secretion is stimulated and Calcitonin is inhibited: bone demineralization leads to entry of more calcium into blood. • When blood calcium is increased, PTH is inhibited and calcitonin is secreted, causing more entry of calcium into bone. Calcitonin and Calcitriol are Different • Calcitonin is the peptide hormone released from thyroid gland. It decreases blood calcium level. • Calcitriol is the active form of vitamin D. It • increases the blood calcium Functions of Phosphate Ions • 1. Formation of bone and teeth. • 2. Production of high energy phosphate compounds such as ATP, CTP, GTP, creatine phosphate, etc. • 3. Synthesis of nucleoside co-enzymes such as NAD and NADP. • 4. DNA and RNA synthesis, where phosphodiester linkages form the backbone of the structure. • 5. Formation of phosphate esters such as glucose-6-phosphate, phospholipids. • 6. Formation of phosphoproteins, e.g. casein. • 7. Activation of enzymes by phosphorylation. • 8. Phosphate buffer system in blood. The ratio of Na2HPO4 : NaH2PO4 in blood is 4:1at pH of 7.4. Phosphate level also has an effect on calcium homeostasis: • Hypophosphatemia increases the serum calcium level. • Hypophosphatemia enhances the hydroxylation of vitamin D in kidneys to form calcitriol, which has hypercalcemic effect. When to check calcium level? • • • • • • • Neurological symptoms,irritability, seizures Renal calculi Ectopic calcification Suspected malignancies Polyuria &polydypsia Chronic renal failure Prolonged drug treatment, which cause hypercalcemia (thiazide diuretics) Phosphate level is to checked • • • • • Renal tubular dzs Hyperparathyroidism Hypoparathyroidism Bone dzs such as ricket Muscle weakness Causes of Hyperphosphatemia • • • • • • • • • • • • • • • 1. Increased absorption of phosphate Excess vitamin D Phosphate infusion 2. Increased cell lysis Chemotherapy for cancer Bone secondaries Rhabdomyolysis 3. Decreased excretion of phosphorus Renal impairment Hypoparathyroidism 4. Hypocalcemia 5. Massive blood transfusions 6. Thyrotoxicosis 7. Drugs Chlorothiazide, Nifedipine, Furosemide Causes of Hypophosphatemia • • • • • 1. Decreased absorption of phosphate Malnutrition Malabsorption Chronic diarrhea Vitamin D deficiency • 2. Intracellular shift • • • Insulin therapy, glucose phosphorylation Respiratory alkalosis 3. Increased urinary excretion of phosphate • • • Hyperparathyroidism Fanconi's syndrome Hypophosphatemic rickets • • • • • 4. Hereditary hypophosphatemia 5. Hypercalcemia 6. Chronic alcoholism 7. Drugs Antacids, Diuretics, Salicylate intoxication Important Combinations of Serum Calcium and Phosphate Levels in Blood • • • • • • • • • • • • • 1. Increased P with decreased Ca Hypoparathyroidism Renal disease 2. Increased P with normal or increased Ca Milk alkali syndrome Hypervitaminosis D 3. Decreased P with increased Ca Hyperparathyroidism Sarcoidosis 4. Decreased P and Ca Malabsorption Vitamin D deficiency Renal tubular acidosis Magnesium • MAGNESIUM (Mg++) Magnesium is the fourth most abundant cation in the body and second most prevalent intracellular cation. • Magnesium is mainly seen in intracellular fluid. Total body magnesium is about 25 g, 60% of which is complexed with calcium in bone. Functions of Magnesium • 1. Mg++ is the activator of many enzymes requiring ATP. Alkaline phosphatase, hexokinase, fructokinase, phosphofructokinase, adenyl cyclase, cAMP dependent kinases, etc. need magnesium. • 2. Neuromuscular irritability is lowered by magnesium. • 3. Insulin-dependent uptake of glucose is reduced in magnesium deficiency. Magnesium supplementation improves glucose tolerance. • SULFUR Source of sulfates is mainly amino acids cysteine and methionine. Proteins contain about 1% sulfur by weight. Inorganic sulfates of Na+, K+ and Mg++, though available in food, are not utilized. Functions of Sulfur • 1. Sulfur containing amino acids are important constituents of body proteins. The disulfide bridges keep polypeptide units together, e.g. insulin, immunoglobulins. • 2. Chondroitin sulfates are seen in cartilage and bone. • 3. Keratin is rich in sulfur, and is present in hair and nail. • 4. Many enzymes and peptides contain -SH group at the active site, e.g. glutathione. • 5. Co-enzymes derived from thiamine, biotin, pantothenic acid and lipoic acid also contain sulfur. • 6. If sulfate is to be introduced in glycosaminoglycans or in phenols for detoxification, it can be done only by phosphoadenosine phosphosulfate (PAPS). • 7. Sulfates are also important in detoxification mechanisms, e.g. production of indoxyl sulphate IRON (Fe) • Distribution of iron Total body iron content is 3 to 5 gm; 75% of which is in blood, the rest is in liver, bone marrow and muscles. Iron is present in almost all cells. • Heme containing proteins are shown in Table 35.2. Blood contains 14.5 g of Hb per 100 ml. About 75% of total iron is in hemoglobin, and 5% is in myoglobin and 15% in ferritin. Heme-containing proteins • • • • • • • Hemoglobin Myoglobin Cytochrome oxidase Cytochrome Cytochrome c1 Cytochrome c Cytochrome b5 Cytochrome p-450 Catalase Nonheme Iron-containing Proteins • • • • • Aconitase Phe-hydroxylase Transferrin Plasma Ferritin Tissues Hemosiderin COPPER (Cu) • Total body copper is about 100 mg. • It is seen in muscles, liver, bone marrow, brain, kidney, heart and in hair. • Copper containing enzymes are ceruloplasmin, cytochrome oxidase, cytochrome c, tyrosinase, lysyl oxidase, ALA synthase, monoamine oxidase, superoxide dismutase and phenol oxidase Functions of Copper • 1. It is necessary for iron absorption and incorporation of iron into hemoglobin. • 2. It is necessary for tyrosinase activity. • 3. It is a co-factor for vitamin C requiring hydroxylations. • 4. It increases HDL and so protects the heart. Fluoride • Fluoride is known to prevent caries. • Caries is a Latin term, meaning "decay". • In the pits and fissures of premolar and molar teeth, bacterial fermentation of residual food leads to acid production FLuorosis is More Dangerous Than Caries • Fluoride level more than 2 ppm will cause chronic intestinal upset, gastroenteritis, loss of appetite and loss of weight. • Level more than 5 ppm causes mottling of enamel, stratification and discoloration of teeth. • A level more than 20 ppm is toxic, leading to alternate areas of osteoporosis and osteosclerosis, with brittle bones. • This is called fluorosis. ZINC (Zn) • Total zinc content of body is about 2 gm, out of which 60% is in skeletal muscles and 30% in bones. • Highest concentration of zinc is seen in hippocampus area of brain and prostatic secretion. • In liver, zinc is stored in combination with a specific protein, metallothionein. Zinc is excreted through pancreatic juice and to a lesser extent through sweat. • More than 300 enzymes are zinc-dependent. • Some important ones are carboxypeptidase, carbonic anhydrase, alkaline phosphatase, lactate dehydrogenase, alcohol dehydrogenase and glutamate dehydrogenase. RNA polymerase contains zinc and so it is required for protein biosynthesis. Extracellular superoxide dismutase is zinc dependent and so, zinc has antioxidant activity. • Insulin when stored in the beta cells of pancreas contains zinc, which stabilizes the hormone molecule. But the insulin released into the blood does not contain zinc. The commercially available preparation, protaminzinc-insulinate (PZI) also contains zinc. Zinc containing protein, Gusten, in saliva is important for taste sensation. Zinc deficiency manifestations • Poor wound healing, lesions of skin, impaired spermatogenesis, hyperkeratosis, dermatitis and alopecia are deficiency manifestations of zinc. • There is reduction in number of T and B lymphocytes. • Macrophage function is retarded. Zinc deficiency leads to depression, dementia and other psychiatric disorders. Zinc binds with amyloid to form a plaque in Alzheimer's disease • SELENIUM (Se) Selenium intake depends on the nature of the soil in which food crops are grown. Requirement is 50-100 microgram/day. Normal serum level is 50-100 microgram/dl. • In mammals, glutathione peroxidase (GP) is the important selenium containing enzyme. RBC contains good quantity of glutathione peroxidase. Thyroxin is converted to T3 by 5'de-iodinase, which is a selenium containing enzyme. • In Se deficiency, this enzyme becomes less active, leading to hypothyroidism. • Selenium concentration in testis is the highest in adult tissue. • It is necessary for normal development of spermatozoa. It is concentrated in the midpiece of spermatozoa as a specific selenoprotein in mitochondria MANGANESE (Mn) • Total body manganese is 15 mg. Maximum concentration is in liver (1.5 ppm). In the cells, it is mainly seen inside the nuclei, as complexed with nucleic acids. Functions: • The following enzymes either contain or are activated by manganese: Hexokinase, phosphoglucomutase, pyruvate carboxylase, isocitrate dehydrogenase, succinate dehydrogenase, arginase, glutamine synthetase • Mndependent superoxide dismutase. Manganese is an integral part of glycosyl transferases, responsible for synthesis of glycoproteins and chondroitin sulfate. Mn is also required for RNA polymerase activity.