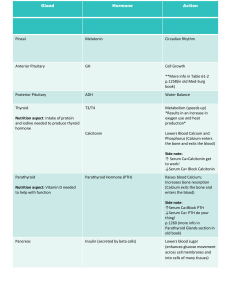
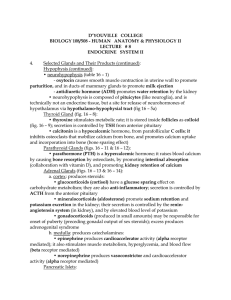
THE PARATHYROID GLAND Parathyroid Hormone, Calcitonin, Calcium and Phosphate Metabolism, Vitamin D, Bone The physiology of calcium and phosphate Metabolism, formation of bone and teeth, and regulation of vitamin D, parathyroid hormone (PTH) and calcitonin are all closely intertwined Overview of Calcium and Phosphate Regulation in the ECF and Plasma CALCIUM – 1100 GM – 1.5% of body weight 1. Skeleton (99%) a. Rapidly Exchangeable reservoir b. Stable calcium 2. Blood (1%) 9 – 10 mg%, Average 9.4 mg%, 2.4 mmol per liter a. 41% ( 1 mmol/L) - combination with plasma protein and is non-diffusible through capillary membrane b. 9% ( 0.2 mmol/L ) - diffusible , not ionized c. 50% - diffusible and ionized Absorption and Excretion of Calcium and Phosphate Intestinal Absorption and Fecal Excretion of Calcium and Phosphate Renal Excretion of Calcium and Phosphate Bone and Its Relation to Extracellular Calcium and Phosphate Composition of Compact Bone 1. Organic Matrix (30%) - 90 to 95% collagen fibers - Remainder is ground substance ( composed of ECF plus proteoglycans esp. chondroitin sulfate and hyaluronic acid 2. Bone Salts (70) - crystalline salt is composed principally of calcium and phosphate, known as Hydroxyapatite Tensile and Compressional Strength of Bone Collagen fibers of bone have great tensile strength Calcium salts have great compressional strength Deposition and Absorption of Bone Deposition of Bone by the Osteoblast Absorption of Bone by the Osteoclast The Osteoclast send out villus-like projections toward the bone. The villi secrete: 1. proteolytic enzyme released from lysosome of the osteoclast 2. several acids including lactic acid and citric acid, released from the mitochondria and secretory vesicles VITAMIN D Steps that Lead to the Formation of Substances from Vitamin D - Cholecalciferol (Vitamin D3) is Formed in the Skin - Cholecalciferol is Converted to 25Hydroxycholecalciferol in the liver - Formation of 1,25Dihydroxycholecalciferol in the Kidneys and Its Control by Parathyroid Hormone - Calcium Ion Concentration Controls the Formation of 1,25 Dihydrocholecalciferol Actions of Vitamin D 1. “Hormonal “ Effect of Vitamin D to Promote Intestinal Calcium Absorption 2. Vitamin D Promotes Phosphate Absorption by the Intestine 3. Vitamin D Decreases Renal Calcium Absorption and Phosphate Excretion 4. Effect of Vitamin D on Bone and its Relation to Parathyroid Hormone Activity PARATHYROID HORMONE Physiologic Anatomy of the Parathyroid Gland Effect of Parathyroid Hormone on Calcium and Phosphate Concentrations in the ECF The rise in calcium concentration is caused by two Effects 1. an effect of PTH to increase calcium and phosphate absorption from the bone 2. a rapid effect of PTH to decrease the excretion of calcium by the kidneys - Parathyroid Hormone Increased Calcium and Phosphate Absorption from the Bone - Rapid Phase of Calcium and Phosphate Absorption – Osteolysis - Slow Phase of Bone Absorption and Calcium Phosphate Release – Activation of the Osteoclasts - Parathyroid Hormone Decreases Calcium Excretion and Increase Phosphate Excretion in the Kidneys - Parathyroid Hormone Increases Intestinal absorption of Calcium and Phosphate - Cyclic Adenosine Monophosphate Mediates the Effects of Parathyroid Hormone ACTIONS OF PTH ON TARGET ORGANS 1. BONES OR SKELETON Calcium and Phosphate absorption from bones a. Rapid Phase – osteolysis b. Slow Phase – activation of osteoclasts 1. immediate activation of osteoclasts that are already formed 2. formation of new osteoclasts from osteoprogenator cells 2. INTESTINES Enhances both Ca and PO4 absorption from the intestines by increasing formation of 1, 25 dihydroxycholecalciferol from vitamin 3. KIDNEYS a. Increased renal tubular reabsorption of calcium in the distal tubules and collecting ducts b. diminished proximal tubular reabsorption of PO4 EFFECTS OF PTH ON TARGET ORGANS 1. Blood Calcium and Phosphate a. Hypercalcemia b. Hypophosphatemia 2. Urine a. Hypocalciuria b. Hyperphosphatemia - phosphaturic Control of Parathyroid Hormone Secretion CALCITONIN Peptide hormone secreted by the thyroid gland that tends to decrease plasma calcium concentration. Two ways: 1. decrease absorptive activities of the osteoclasts and the osteocytic effect of the osteocytic membrane – immediate effect 2. decrease formation of new osteoclasts – more prolonged effect Increased Plasma Calcium Concentration Stimulates Calcitonin Secretion Calcitonin Has a Weak Effect on Plasma Calcium Concentration in Adult Human SUMMARY OF CONTROL OF CALCIUM ION CONCENTRATION 1. Buffer Function of the Exchangeable Calcium in Bones - the First Line of Defense 2. Hormonal Control of Calcium ion concentration – the Second Line of Defense a. PTH b. Calcitonin PARATHYROID HORMONE and BONE DISEASE 1. Hypoparathryroidism a.Tetany – Calcium concentration is 6-7 mg% - Larygospasm Signs of Latent Tetany 1. Chvostek’s sign 2. Trousseau’s sign b. Impairment of blood clotting 2. Hyperparathyroidism a. Bone Disease - broken bones - Cystic bone disease – Osteitis Fibrosa Cystica or Von Recklinghausen’s Disease b. Effects of Hypercalcemia 1. Rise of calcium to 12-15 mg% - depression of central and peripheral nervous system - muscular weakness, constipation, abdominal pain, peptic ulcer, lack of appetite, depressed relaxation of the heart during diastole 2. Formation of kidney stones 3. Parathyroid hormone poisoning and metastatic calcification- 17 mg% Calcium •alveoli of the lungs – tubules of kidneys •thyroid gland – walls of the arteries •stomach mucosa BONE DISEASES Rickets – Vitamin D Deficiency - occurs mainly in children - results from calcium or phosphate deficiency in the ECF caused by lack of VitaminD - develops tetany Osteomalacia – “Adult Rickets” - deficiency of both vitamin D and calcium occurs as aresult of steatorrhea (failure to absorb fat) because vitamin D is fat soluble - “Renal rickets” is a type of osteomalacia that results from kidney damage Osteoporosis – Decreased Bone Matrix - the most common of all bone disease in adults especially in old age - results from diminished bone matrix rather than poor bone calcification Causes: a. lack of physical stress on the bones due to inactivity b. malnutrition – sufficient protein matrix cannot be formed c. lack of vitamin C – necessary for secretion of intercellular substances d. postmenopausal lack of estrogen secretion – estrogen have osteoblast-stimulating activity e. old age – diminished growth hormone f. Cushing’s syndrome – massive glucocorticoids cause decreased deposition of protein thus depressing osteoblastic activity PHYSIOLOGY OF THE TEETH