Disorders of Calcium Metabolism: Hypercalcemia Steven Chessler, MD, Ph.D. March, 2015
advertisement

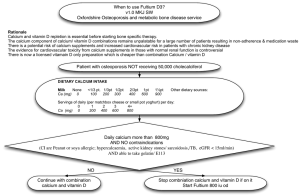
Disorders of Calcium Metabolism: Hypercalcemia Steven Chessler, MD, Ph.D. March, 2015 Internal Medicine noon conference (F5) History and Physical A 45 year-old female consults you because of a low bone mineral density (BMD). She relates that she availed herself of a free screening test of her BMD. The results indicated that she had osteopenia, so she called your office for an appointment. The checklist that she filled out indicates that she is in good health and on no medications. She looks well and the physical is unrevealing. Laboratory Her routine laboratory evaluation is essentially normal, including normal renal function, except for a serum calcium of 10.6, where 10.5 is the upper limit of normal. A DEXA reveals normal bone mineral density. What labs would you order to follow-up on the Ca++? History and Physical A 45 year-old female consults you because of a low bone mineral density (BMD). She relates that she availed herself of a free screening test of her bone mineral density (BMD). The results indicated that she had osteopenia, so she called your office for an appointment. The checklist that she filled out indicates that she is in good health and on no medications. She looks well and the physical is unrevealing. Laboratory Her routine laboratory evaluation is essentially normal, including normal renal function, but includes a serum calcium of 10.6, where 10.5 is the upper limit of normal. A DEXA reveals normal bone mineral density What labs would you order to follow-up on the Ca++? Results Repeat Ca++: 10.8 Albumin: 4 mg/dl Phos: 3 mg/dl (2.5-4.0) PTH (at same time): 42 pg/ml (nl: 11-54) After verifying the lab results thus far, which would be the best test to help confirm the most likely diagnosis and avoid possible unnecessary treatment? A. 1,25-dihyroxyvitamin D B. 25-hydroxyvitamin D C. Spot urine Ca++ D. 24 hour urine Ca++ E. PTHrP Answer is D: • Twenty-four-hour urine for calcium will help in the differential diagnosis of FHH. If marked hypercalciuriais present (ie, > 400 mg/d), a more complete urinary biochemical stone profile should be considered. In the presence of abnormal findings indicating increased calcium-containing stone risk and marked hypercalciuria, a guideline for surgery is met. 24 hour urine is 114 mg/24 hours. (normal 100-300) Best single next step to help establish diagnosis? A. Family history B. Sestamibi imaging of parathyroid glands C. Surgical exploration of parathyroid glands D. TSH and free T4 Same case, but now result is: 24 hour urine is 450 mg/24 hours (normal 100-300). Also, there is no history of renal stones, fracture, mental status changes or other symptoms. Most appropriate therapy (per current guidelines)? A. Cinacalcet B. Parathyroid surgery C. Alendronate D. Either parathyroid surgery or monitoring over time E. Monitoring over time Primary Hyperparathyroidism: Management Guidelines (2013) surgery recommended if: Measurement Result Serum calcium (>upper limit of nl.) 1.0 mg/dL (0.25 mmol/L) Skeletal A. BMD by DXA: T-score <-2.5 at lumbar spine, total hip, femoral neck, or distal 1/3 radius B. Vertebral fracture Renal A. Creatinine clearance <60 cc/min B. 24-h urine for calcium >400 mg/d and increased stone risk by biochemical stone risk analysis C. Presence of nephrolithiasis or nephrocalcinosis by x-ray, ultrasound, or CT Age, y <50 Hypercalcemia/hyperparathyroidism: clinical signs • GI: – Nausea, vomiting, abdominal pain – Constipation • Renal: – Polyuria, dehydration – Renal failure – Nephrolithiasis Hypercalcemia/hyperparathyroidism: clinical signs • Neurological – – – – Fatigue Confusion Depression Stupor, coma • Skeletal – Bone pain and tenderness – Spontaneous fracture (compression fx’s) Hyperparathyroidism/Hypercalcemia – signs/symptoms • Neuromuscular – Muscle weakness, hypotonia • Cardiovascular – Hypertension – Short QT interval Hypercalcemia: major causes • Primary hyperparathyroidism (PHPT) • Malignancy • Others Hyperparathyroidism: causes • Primary – Adenoma (90%) – Multiple gland enlargement (10%) • MEN 1 • MEN 2A • Familial hyperparathyroidism – Carcinoma (<1%) – Familial benign hypercalcemia (FBH) • Secondary (normo- or hypocalcemic) – Renal failure – Vitamin D deficiency Primary hyperparathyroidism • Affects approximately 100,000 patients a year. • Prevalence: 0.1 to 0.3% of the general population. • More common in women (1:500) than in men (1:2000). • Patients with single adenoma (~90%): minimally invasive surgery Sestamibi imaging ~90% sensitive, ~98% specific Minimally invasive = incision length < 2.5 cm Intraoperative PTH testing confirms biochemical cure Malignant hypercalcemia: major causes • PTHrP - mediated – Breast carcinoma – Squamous carcinoma (lung, head & neck, esophagus) – Renal carcinoma • Cytokine/osteoclast activating factor - mediated – Myeloma (lymphoma, leukemia) • Tumor production of calcitriol – Lymphoma Hypercalcemia: other causes • Drugs: – – – – – Vitamin D Calcium carbonate (milk alkali syndrome) Lithium Thiazide diuretics Vitamin A • Sarcoidosis, other granulomatous disorders • Hyperthyroidism REVIEW, Ca++ metabolism: PTH, Vitamin D and Calcium homeostasis 1. Calcium and phosphorus 2. 3. 4. 5. Bone Vitamin D Parathyroid Hormone Calcitonin Extracellular Calcium • Three definable fractions of calcium in serum: – Ionized calcium 50% – Protein-bound calcium 41% • 90% bound to albumin – Calcium complexed to serum constituents 9% • Citrate and phosphate Calcium turnover Renal Excretion • The kidneys account for the bulk of regulated calcium excretion • Three distinct locations along the renal tubule are involved • The regulation of calcium excretion at each of the three renal sites is different Renal Excretion • Proximal convoluted tubule – Accounts for 70% of calcium reabsorption – Mainly paracellular pathway Renal Excretion • Proximal convoluted tubule • Thick ascending limb of loop of Henle 20 % of calcium reabsorption Calcium sensing receptor (CaSR) FHH, FBH (familial benign/hypocalciuric hypercalcemia) Caskey F J , Pickett T M Nephrol. Dial. Transplant. 2005;20:1752-1755 Renal Excretion • Proximal convoluted tubule • Thick ascending limb • Distal convoluted tubule – PTH regulation – 8% of calcium reabsorption 20-24 PTH, Vitamin D and Calcium homeostasis 1. Calcium and phosphorus 2. Bone 3. Vitamin D 4. Parathyroid Hormone 5. Calcitonin 20-25 Calcium Regulation: Bone Exchange • Bone is dynamic and is constantly remodeled • Calcium is exchanged between blood and bone daily (roughly 400 mg/day); 10% of skeleton per year • Ongoing remodeling allows bone to store and release calcium as needed to help maintain homeostasis Normal bone remodeling cycle Case: Man With Lethargy, Fatigue and Weakness • 60 yr old male presents with complaints of fatigue and weakness over 1 month. • PMHx: Negative; no history CHF or kidney disease • PE: significant for memory and cognitive defects • Lab: Ca 15.0 mg/dL PO4 2.3 mg/dL 60 yr old male presents with complaints of fatigue and weakness over 1 month. Renal function is normal. PMHx: Negative; no history CHF or kidney disease PE: significant for memory and cognitive defects Lab: Ca 15.0 mg/dL, PO4 2.3 mg/dL Most likely cause of hypercalcemia? A) Vitamin D intoxication B) Granulomatous disease C) Malignancy D) Acute hyperparathyroidism E) Chronic hyperparathyroidism After admission, the patient becomes increasingly obtunded. How do you treat? Severe hypercalcemia: • Principles of therapy – Expand ECF volume – Increase urinary calcium excretion – Decrease bone resorption • Indications for therapy – Symptoms of hypercalcemia – Plasma [Ca] >15 mg/dl Hypercalcemia - Treatment – NS bolus to restore volume; then 100 – 200 ml/hr – Bisphosphonates (onset 24-48 hrs) – Calcitonin 4 – 8 IU q6-8 hrs (onset immediate, resistance develops in 24-48 hrs) – [Mg and K prn] Despite having administered zoledronic acid (4 mg IV), hypercalcemia is not brought under adequate control. The best option for prolonged control is now to add: A) A drug targeting the calcium-sensing receptor (CaSR). B) Pamidronate C) A loop diuretic D) A drug targeting the calcitonin receptor E) A drug targeting RANK ligand (RANKL) Rank Ligand (RANKL) and osteoprotegerin (OPG) balance bone loss and formation • RANKL is a key inducer of osteoclast formation • By binding with RANKL, OPG (or denosumab) prevents RANKL Ligand from binding with RANK on the surface of osteoclasts and their precursors. PTH, Vitamin D and Calcium homeostasis Lecture outline 1. Calcium and phosphorus 2. Bone Hormonal control of Ca2+ 3. Vitamin D 4. Parathyroid Hormone 5. Calcitonin Synthesis of Vitamin D • Parathyroid hormone (PTH) stimulates 1,25(OH)2-Vitamin D synthesis. • The first hydroxylation reaction takes place in the liver yielding 25-hydroxyl D • Second hydroxylation reaction takes place in the kidney yielding 1,25(OH)2-D3 (calcitriol; 1,25-dihydroxyvitamin D). • Sarcoidosis, other granulomatous disorders, certain malignancies (lymphoma) can also produce 1,25(OH)2-D3 20-35 REGULATION OF RENAL 1α-HYDROXYLASE PRODUCTION Stimulates Inhibits PTH Low calcium Low phosphate Calcitonin 1,25(OH)2D3 High calcium High phosphate Case: A 36 yo African-American male with a 5 month history of cough and dyspnea is found to have a calcium level of 10.9 mg/dl (normal < 10.6). His only medication is an albuterol MDI. He smokes 1-2 packs per day. He is thin and illappearing. Physical exam is only notable for lungs having scattered crackles bilaterally and cervical lymphadenopathy. Laboratory results: Albumin— 4 mg/dL (normal) Creatinine: 1.0 mg/dL Repeat Ca++: 10.8 mg/dL Phosphate: 4.5 mg/dL PTH: 9 pg/ml 25-hydroxyvitamin-D: 25 ng/ml (8.5-10.5 mg/dL) (2.5-4.4 mg/dL) (11-54 pg/ml) (30-74 ng/ml) The cause of the hypercalcemia will most likely be revealed by: A. Measurement of 24 hour urine calcium B. Measurement of serum PTHrP C. Measurement of serum 1,25-dihydroxyvitamin-D D. Sequencing of the gene encoding the CaSR Answer: C (has sarcoid or TB so measure 1,25-dihydroxyvit.-D) From: UpToDate, Diagnostic approach to hypercalcemia: “Measurement of the serum phosphate concentration and urinary calcium excretion also may be helpful in selected cases. Hyperparathyroidism and humoral hypercalcemia of malignancy (due to PTH-related protein) may be associated with frank hypophosphatemia or low-normal serum phosphate levels resulting from inhibition of renal proximal tubular phosphate reabsorption. In comparison, the serum phosphate concentration is normal or elevated in granulomatous diseases, vitamin D intoxication, immobilization, thyrotoxicosis, milk-alkali syndrome, and metastatic bone disease.“ Summary: vitamin D action • Main action of 1,25-(OH)2-D is to stimulate absorption of Ca2+ (and phosphate) from the intestine. also: • acts on osteoblasts to increase RANKL and thus activate osteoclasts to increase Ca++ resorbtion. • is necessary for proper bone formation. PTH, Vitamin D and Calcium homeostasis 1. Calcium and phosphorus 2. Bone 3. Vitamin D 4. Parathyroid Hormone 5. Calcitonin 20-41 Parathyroid Hormone Calcium regulates PTH secretion via a CaSR PTH and calcium+phosphate homeostasis PTH, Vitamin D and Calcium homeostasis Lecture outline 1. 2. 3. 4. Calcium and phosphorus Bone Vitamin D Parathyroid Hormone 5. Calcitonin Calcitonin • Decreases plasma Ca2+ and phosphate concentrations, mainly by decreasing bone resorption. • Synthesized and secreted by the parafollicular cells (aka C cells) of the thyroid gland. • Release stimulated by hypercalcemia and inhibited by hypocalcemia Slide credit: Dale Buchanan Hales Ph.D. Calcitonin effects • Calcitonin rapidly inhibits osteoclast activity o causes inhibition of osteoclast motility, alterations in cell morphology and osteoclast inactivation. • Kidneys o inhibits calcium reabsorption (increases excretion) o also increases phosphorus excretion • Role in calcium homeostasis unclear Hormone Effect on bones Effect on gut Effect on kidneys Parathyroid hormone increase Ca++, decrease PO4 levels in blood Promotes resorption Indirect effects via increase in calcitriol from 1hydroxylation Promotes Ca++ reabsorption and PO4 excretion, activates 1hydroxylation Calcitriol (RANKL→bone (vitamin D) Ca++, PO4 levels resportion) increase in blood Increases Ca++ and PO4 absorption No direct effects Calcitonin No direct effects Promotes Ca++ and PO4 excretion Inhibits resorption Hypocalcemia: clinical signs • • • • • Paresthesias Tetany (carpopedal spasm) Trousseau’s, Chvostek’s signs Seizures Chronic: cataracts, basal ganglia Ca Trousseau’s sign Hypocalcemia: causes • Hypoparathyroidism – Surgical (thyroid, parathyroid surgery) – Autoimmune – Magnesium deficiency • PTH resistance (pseudohypoparathyroism) • Vitamin D deficiency • Vitamin D resistance • Other: renal failure, pancreatitis, tumor lysis END