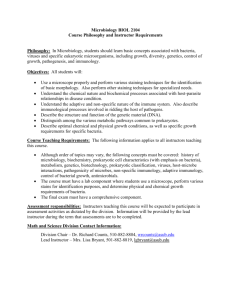
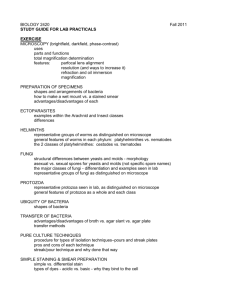
Objectives
advertisement

UNIVERSITY OF TABUK Faculty of Applied Medical Sciences Department of Medical Laboratory Technology LABORATORY MANUAL IN DIAGNOSTIC MICROBIOLOGY 1 (MLT 303) 1st semester 1433/1434 H Prepared by Thamer Hamdan. M.Sc. Clinical Microbiology and Immunology Ayman Sir Alkhatim M.Sc. Medical Microbiology and Immunology Laboratory Manual in Diagnostic Microbiology I Experiment. No. 1 Orientation to Microbiology laboratory and Safety rules Objectives 1- To use, utilize and practice all Safety guidelines in the Microbiology lab. 2- To realize and understand the importance of safety guidelines. 3- To see the safety equipment in microbiology laboratory. Materials Gloves Masks Lab coats Safety shower station Fume hoods Safety cabinets Autoclave Eye washer station Fire extinguisher Background Usually in each lab there are a general lab practices for safety and safety lab guide that help all personnel to deal and contact with lab tools, equipment and practices safely in order to protect the followings from the contamination: a. b. c. d. e. Workers (health care providers) Co-workers (Trainees, visitors & maid/services) Patients Environment Materials and cultures MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. Rev.0. Laboratory Manual in Diagnostic Microbiology I General laboratory safety rules at microbiology laboratory 1. Follow precautionary statements given in each exercise by your instructor 2. Never eat, drink, smoke, or chew gum while working in the laboratory. 3. Students should wear gloves, coats, safety shield or glasses. Shorts and sandals should not be worn in the lab at any time. 4. Do not use any equipment unless you are trained and approved as a user by your supervisor. 5. Long hairs should be tied and placed inside the coat. 6. Removal of media, equipment, and bacterial cultures is prohibited. 7. All cultures should be handled as being potentially pathogenic 8. Keep the work area clear of all materials except those needed for your work. Coats should be hung in the hall or placed in a locker. Extra books, purses, etc. should be kept away from equipment that requires air flow or ventilation to prevent overheating and never place it on bench books 9. Disposal - Students are responsible for the proper disposal of used material if any in appropriate containers. 10. Equipment Failure - If a piece of equipment fails while being used, report it immediately to your lab assistant or tutor. Never try to fix the problem yourself because you could harm yourself and others. 11. Never pipette anything by mouth. 12. Clean up your work area before leaving. 13. At the beginning and termination of each laboratory session are to be wiped with a disinfectant solution. 14. Use a glassware marker. 15. On completion of the laboratory session all cultures and materials to be discard should be placed in the disposal area designated by the instructor. 16. Hands must be washed with detergent before leaving the laboratory. MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. Rev.0. Laboratory Manual in Diagnostic Microbiology I Experiment. No.: 2 Common materials, apparatuses and equipment used in Microbiology laboratory Objectives 1. The student should identify the equipment and tools used in Microbiology laboratory. 2. The student should know the function of that equipment. 3. The student should understand the principle of that equipment. Materials Autoclave Incubator Microscope Oven Centrifuge Safety cabinets Petri dishes Refrigerators Glass slides Flasks Rotator Loops Swabs Forceps Dispenser Thermometer Colony counter Background The students are dealing with many types of equipment. The uses and functions of them will be discussed by the instructor. The following items are used in diagnostic microbiology lab: 1. Autoclave: used to sterilize the items used in microbiology lab. 2. Incubator: to provide the optimum temperature for bacterial growth. 3. Microscope: to visualize tiny objects 4. Oven: to sterilize objects and dry them 5. Centrifuge: for separation purposes 6. Safety cabinets: safety place to perform the procedures 7. Petri dishes ( glass or plastic) with different sizes: for culture 8. Refrigerators: for preservation 9. Glass slides: for smear preparation 10. Glassware: for media preparation 11. Rotator: for mixing 12. Loops (plastic or wire): for inoculation and sub culturing MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. Rev.0. Laboratory Manual in Diagnostic Microbiology I 13. Swabs: for culturing 14. Forceps: to pick up the discs 15. Dispenser: to transfer the media and discs 16. Thermometer: to measure the Temperature 17. Colony counter: to count the No. of colonies. Principle There are different principles for each items and instrument mentioned in the instrument manual. Procedure According to the instructor steps and then students’ application. MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. Rev.0. Laboratory Manual in Diagnostic Microbiology I Experiment. No. 3 Use and care of Microscopes Objectives 1. The student should know the components of compound microscope. 2. The students should be able to use and store the microscope properly. 3. The student should understand the principle of microscopy. Materials Microscope. Xylene. Lens paper. Prepared slides. Background Microscopes: are instruments used to magnify objects that cannot be seen by naked eye (which is unable to distinguish objects with a diameter less than 0.1 mm) . Types of microscopes: 1. Bright-field microscopes 2. Dark- field microscopes 3. Phase-contrast microscopes 4. Fluorescent microscopes 5. Electron microscopes Essentials features of Bright-field microscopes This type of microscope is routinely used to study the size, shape, and arrangement it provides little information about internal cell structure. It contains two main lens systems: The ocular lens in the eyepiece and the objective lens located in the nosepiece The specimen is illuminated by a beam of tungsten light focused on it by a sub stage lens designated as a condenser. The absence of contrast between the specimen and the surrounding medium is the limitation. Essentially, a compound microscope consists of structural and optical components. However, within these two basic systems, there are some essential components that every microscopist should know and understand. These key microscope parts are illustrated and explained below. MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. Rev.0. Laboratory Manual in Diagnostic Microbiology I STRUCTURAL COMPONENTS The three basic structural components of a compound microscope are the head, base and arm. Head/Body houses the optical parts in the upper part of the microscope Base of the microscope supports the microscope and houses the illuminator Arm connects to the base and supports the microscope head. It is also used to carry the microscope. When carrying a compound microscope always take care to lift it by both the arm and base, simultaneously. OPTICAL COMPONENTS There are two optical systems in a compound microscope: Eyepiece Lenses and Objective Lenses: Eyepiece or Ocular is what you look through at the top of the microscope. Typically, standard eyepieces have a magnifying power of 10x. Optional eyepieces of varying powers are available, typically from 5x-30x. Eyepiece tube holds the eyepieces in place above the objective lens. Objective Lenses are the primary optical lenses on a microscope. They range from 4x-100x and typically, include, three, four or five on lens on most microscopes. Objectives can be forward or rearfacing. Resolving nosepiece houses the objectives. Stage is where the specimen to be viewed is placed. A mechanical stage is used when working at higher magnifications where delicate movements of the specimen slide are required. Stage Clips are used when there is no mechanical stage. The viewer is required to move the slide manually to view different sections of the specimen. Aperture is the hole in the stage through which the base (transmitted) light reaches the stage. Illuminator is the light source for a microscope, typically located in the base of the microscope. Most light microscopes use low voltage, halogen bulbs with continuous variable lighting control located within the base. Condenser is used to collect and focus the light from the illuminator on to the specimen. It is located under the stage often in conjunction with an iris diaphragm. Iris Diaphragm controls the amount of light reaching the specimen. It is located above the condenser and below the stage. MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. Rev.0. Laboratory Manual in Diagnostic Microbiology I Coarse adjustment knob- used to initially focus specimen Fine adjustment knob- used for final focus of specimen. Principle Theoretical principles of Microscopy Magnification Objective lens Ocular lens Total magnification Scanning lens 4X 10X 40X Low power lens 10X 10X 100X High power dry lens 40 X 10X 400X Oil immersion lens 100X 10X 1000X Refractive index: bending power of light passing from the glass slide into objective lens. RI of air is less than the glass, so the light rays passing from the glass slide into the air will be lost How to compensate? By using immersion oil (cedar). ( have the same RI as glass) Limit of resolution of the lens: the minimum distance between two closely spaced points in an object that can be seen as distinct points in the image Most microscopes are par focal: par focal is the ability to move from high power to low power with minor adjustments. MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. Rev.0. Laboratory Manual in Diagnostic Microbiology I Procedure MICROSCOPE USE AND CARE Always carry the microscope with two hands, one hand on the arm and one hand placed under the base for support. Remove cover, plug into outlet, and turn on light. Place slide in stage, when it is in down position Using scanning objective (RED), locate object; using the coarse adjustment knob focus to obtain the clearest image possible. Using the fine adjustment knob, bring the object into the clearest image possible; center object in the field of view. Bring the low power objective (yellow) into place Focus the object using minor adjustments with the fine adjustment knob. Centre object in field of view; adjust light source if needed. Bring the high power objective (blue-sky is high) into place. When finished with your microscope: Remove slide, when the objective lens is on scanning position. Centre the mechanical stage holder Place the red scanning objective in place Return stage to the down position Turn off light Clean the oil immersion lens with xylene. Fold up and tie cord Replace cover Return microscope to the cabinet MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. Rev.0. Laboratory Manual in Diagnostic Microbiology I Experiment. No. 4 Cultural Media ( Preparation and Types) Objectives 1. The student should know the composition of cultural media. 2. The student should be able to differentiate between different types of media. 3. The student should prepare different types of media under aseptic techniques. Materials • • • • • • • • • • • Glass wares Distilled water Dehydrated media Magnetic beads Hot plate Balance Spatula Filter paper Autoclave Petri dishes Sterile glass or plastic tubes Background • Culture: growth in media containing living microorganisms. • Pure culture: growth in media containing one type of bacteria. • Mixed culture: growth in media containing more than one type of bacteria. • Culture media: solution that contains nutrients for bacterial growth and identification. Nutrients materials in media • Water • Source of carbon • Source of nitrogen • Buffer system • Source of minerals Types of media ( composition) • Chemically defined media: the chemical composition is known e.g. minimal salt medium • Complex (undefined medium): the chemical constitution is unknown e.g. blood agar Types of media(content)(percentage of agar) • Agar: solidifying agent for solid or semi-solid (hydrocolloid derived from red algae) (it melts at 100 degrees and remains liquid until cooled to 40 degrees). 1) Liquid media (broth): no agar, nutrient broth used for growth of pure culture. 2) semi-solid media: > 1% agar, motility media MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. Rev.0. Laboratory Manual in Diagnostic Microbiology I 3) solidified media: 1.5-1.8% agar , nutrient agar • Slanted agar position: used for maintenance, preservation of pure culture and sub culturing • Deep agar position: used for storage and for studying the gaseous requirements of microorganisms. • Agar plate media (Petri dishes): used of isolation and sub culturing purposes. Principle Types of media ( purpose) • • • • • All-purpose medium ( simple): supports the growth of most organisms( trypticase soy broth and nutrient broth) Enriched medium: base growth medium with special supplements added such as: blood, vitamins and amino acids (most bacteria grow on it). ( blood agar) Differential medium: more than one type of bacteria can grow and separation is based on color and other ( blood agar) Selective medium: it allows one or more species to grow and suppresses others by incorporating dyes, antibiotics, adjusting pH, bile salts…ets.( Salmonella- Shigella agar (SS agar) Selective and differential medium: contain pH indicator and an inhibitor. E.g. MacConkey agar ( contain bile salts and crystal violet as inhibitor and neutral red as pH indicator) Another example is Mannitol salt agar (high salt concentration and phenol red). Procedure Identification of different types of media the student should know and examine with the aid of instructor the different types of media Media preparation 1. The dehydrated media is weighed and dissolved in a specific amount of water in flask. 2. Bring to gentle boil on a hotplate until all ingredients are dissolved. 3. Cover the flask with cotton and aluminum foil to prevent vaporization. 4. Autoclave at 121 degrees under 15 Ibs pressure for 15 minutes. 5. After autoclaving period, cool the flask to 50 degrees. 6. Working quickly, remove the cap of flask, flame the mouth, and pour the liquid agar into sterile Petri dishes while the cover is partially raised. 7. Allow all plates to cool for about 15 minutes without moving 8. The media are ready for inoculation. MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. Rev.0. Laboratory Manual in Diagnostic Microbiology I Experiment. No. 5 Isolation techniques with aseptic techniques to cultivate bacteria Objectives Each student should be able to 1. Understand the purpose of the isolation techniques. 2. Use aseptic technique to remove and transfer bacteria for subculturing. 3. Correctly use an inoculating loop and needle. 4. Perform the isolation techniques. Materials Slant cultures of either Serratia marcescens pigmented (ATCC13880) or Micrococcusroseus (ATCC 186) or Streak-plate cultures. Sterile Nutrient broth tubes. Sterile Nutrient agar slants. Sterile Nutrient agar deeps. Wax pencil. Inoculating loop, inoculating needle. Bunsen burner &vortex mixer (if available). Background In natural habitats, bacteria usually grow together in populations containing a number of species. In order to adequately study and characterize an individual bacterial species, one needs a pure culture. In the clinical laboratory, growth of a pure culture is absolutely necessary before any biochemical tests can be performed to identify a suspect micro organism. Aseptic technique Method of handling material without contamination from the environment. Procedure 1. Working in 20 cm diameter around a blue flame (sterile zone). 2. Never leave a culture dish open, even for a short time ,When it is necessary to open a dish, keep the lid close to the dish, and keep the lid between your face and the agar surface. 3. For most bacterial cultures you will use a sterile loop or needle to inoculate or to obtain an inoculums. 4. Flame a loop or needle to red-hot just prior to use, burning off any organic material ,Cool the loop by touching the sterile agar or liquid surface prior to touching a culture. MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. Rev.0. Laboratory Manual in Diagnostic Microbiology I Procedure for Culture Transfer Instruments and Techniques 1. Using a wax pencil, label the tube or plate to be noculated with the date, your name, and the name of the test microorganism (figure 5.1a). 2. Gently mix the primary culture tube in order to put the bacteria into a uniform suspension. (figure5.1b). The tube can be tapped to create a vortex that will suspend the microorganisms, or if a vortex mixer is available, it can be used. 3. Place the stock culture tube and the tube to be inoculated in the palm of one hand and secure with the thumb. The tubes are then separated to form a V in the hand (figure 5.1c). They should be held at an angle so that the open ends are not vertical and directly exposed to airborne laboratory contaminants. 4. Using the other hand, flame the inoculating loopor needle over a Bunsen burner until the wirebecomes red-hot (figure 5.1d). 5. Using the same hand that is holding the inoculatingloop, remove the caps from the two tubes, holdthem between your fingers, and briefly flame thenecks of the tubes over a Bunsen burner (figure5.1e) by passing them through the flame. However, do notallow the tubes tobecome redhot. 6. Cool the hot loop in the broth culture until it stops“hissing.” With the sterile inoculating loop, transfer1 drop of culture from the stock culture tube intothe new broth tube. At this point, one could alsotransfer to a glass slide, streak the surface of a slant,or streak the bacteria onto the surface of a petriplate (figure 5.1f ). When picking up bacteria froma slant, cool the hot loop or needle by holding itagainst the top of the slant until it stops “hissing.” 7. Reflame the neck of the tubes (figure 5.1g). 8. Recap the tubes (figure 5.1h). 9. Reflame or sterilize the loop or needle. (figure 5.1 ).Aseptic Technique for Bacterial Removal and Subculturing MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. Rev.0. Laboratory Manual in Diagnostic Microbiology I Procedure for Isolation of Pure Cultures and Their Maintenance Streak plate technique. 1. Slant inoculation technique. 2. Liquid medium inoculation technique. 3. Semisolid medium inoculation technique. MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. Rev.0. Laboratory Manual in Diagnostic Microbiology I 1. Streak plate technique. Principle Isolated, pure colonies can be obtained by the streak-plate technique. In this technique, the bacterial mixture or samples are transferred to the edge of an agar plate with sterile inoculating loop and then streaked out over the surface in one of several patterns. At some point on the streaks, individual cells will be removed from the loop as it glides along the agar surface and will give rise to separate colonies. Again; one assumes that one colony comes from one cell. The key principle of this method is that by streaking, a dilution gradient is established on the surface of the plate as cells are deposited on the agar surface. Because of this gradient, confluent growth occurs on part of the plate where the cells are not sufficiently separated, and individual, well isolated colonies develop in other regions of the plate where few enough cells are deposited to form separate colonies that can be seen with the naked eye. Cells from the new colony can then be picked up with an inoculating needle and transferred to an agar slant or other suitable medium for maintenance of the pure culture. Procedure 1. Aseptically remove a loopful of the bacterial mixture or clinical samples. (See figure 5.1). 2. Streak out the loopful of bacteria or sample on the agar plate (nutrient agar)as follows: a. Carefully lift the top of the petri plate just enough to insert your inoculating loop easily. b. The top should cover the agar surface as completely as possible at all times in order to avoid contamination. c. Insert the inoculating loopful of bacteria or samples and spread it over a small area (area 1) at one edge of the plate as shown in figure 4.2b in order to make effective use of the agar surface. This is accomplished by letting the loop rest gently on the surface of the agar and then moving it across the surface each time without digging into the agar. d. Remove the inoculating loop and kill any remaining bacteria by flaming them. Then insert the loop under the lid and cool it at the edge of the agar near area 1. e. Rotate the plate while carefully keeping in mind where the initial streaks ended (use the marked quadrants as a guide) and crossover the streaks in area 1 (figure 16.2b).Streak out any bacteria picked up as shown in area 2.Remove the loop, flame it, cool in the agar as before, and repeat the streaking process (figure 16.2b, area 3). f. Repeat this sequence once more to make a fourth set of streaks (area 4). Use fewer crossstreaks here than in the previous quadrant. g. Incubate the plates at 37°C for 24 hours in an inverted position. Afterwards, examine each of the agar plates to determine the distribution and amount of growth in the three or four streaked areas. (Figure 5.2).Preparation of (a) Streak Plate. Arrows indicate motion of the loop. In (b), flame and cool the loop between 1 and 2, 2 and 3, and 3 and 4 the end of the streak. The goal is to thin the numbers of bacteria growing in each successive area of the plate as it is rotated and streaked so that well isolated colonies will appear in quadrant 3& 4. MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. Rev.0. Laboratory Manual in Diagnostic Microbiology I MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. Rev.0. Laboratory Manual in Diagnostic Microbiology I Result 1. Area of initial inoculation and the first streak yield heavy growth. 2. Area of second streak from area 1 yields less dense growth. 3. Area of third streak from area 2 yields weak growth. 4. Area of fourth streak from area 3 yield single colonies (discrete colonies) (pure colonies). 2. Slant inoculation technique 3. Liquid medium inoculation technique. Procedure 1. With a wax pencil, label the nutrient agar slants with the names of the respective bacteria. Do the same for the broth tubes. Add your name and date. 2. Using aseptic technique, select a well-isolated colony for each type of bacteria and pickoff as much of the center of the colony as possible with an inoculating loop. 3. Introduce the inoculating loop in the slant culture then stabbing the agar and do zigzag in the surface of agar. 4. In the broth culture transfer the inoculating loop with colony into tube and scratch the wall of tube over the broth in order to let bacteria drop into the liquid then mixing well. 5. Flame the mouth of the tube and reinsert the cotton plug. Flame-sterilize inoculating loop. 6. If screw-cap tubes are used, they must be loosened slightly before incubation to keep the slant and broth culture aerobic. MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. Rev.0. Laboratory Manual in Diagnostic Microbiology I 7. After incubating 24 hours at 37°C, you should have two pure slant and two pure broth stock cultures. 8. Observe the slant (figure 4.4) and broth cultures (figure 4.5) while taking care not to agitate them. 9. Place the pure cultures in the refrigerator for later use. (figure 5.3) Transferring Techniques. (a)–(c) Stab technique for transferring bacteria. Notice that the inoculating needle is moved into the tube without touching the walls of the tube, and the needle penetrates medium to 2/3 its depth. (d) Technique for streaking the surface of a slant with a loop. Result (Figure 4.4) Some typical growth Patterns in slant media. (Figure 4.4) Some typical growth patterns in broth media. MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. Rev.0. Laboratory Manual in Diagnostic Microbiology I 4. Semisolid medium inoculation technique. It is most commonly used test for motility in microbiology lab. It depends on the ability of motile bacteria to move through semi-solid media. Ordinary solid media contain 1.5-2.0% Agar. The semisolid media contain about 0.4% Agar. Procedure 1. With a wax pencil, label the semi-solid media (deep agar) tube with the names of the respective bacteria. 2. Using aseptic technique, select a well-isolated colony and pick off as much of the center of the colony as possible with an inoculating loop. 3. Insert the inoculating loop in the center of deep agar then stabbing the agar, be cautious not to touch the bottom of the tube, and then draw it out in the same way. (Figure 4.3.d). 4. Flame the mouth of the tube and reinsert the cotton plug. Flame-sterilize inoculating loop. 5. If screw-cap tubes are used, they must be loosened slightly before incubation to keep the deep agar culture aerobic. 6. Incubate the tube at 37°C for 24. Result Motile bacteria will migrate from the line of inoculation to form a diffuse turbidity in the surrounding medium. Non motile bacteria will grow only along the line of inoculation. A colored indicator can be used to make the results easier to see. MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. Rev.0. Laboratory Manual in Diagnostic Microbiology I From left to right: + MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. Rev.0. – + Laboratory Manual in Diagnostic Microbiology 1 Experiment. No. 6 Smear preparation and staining principle Objectives 1. 2. 3. To prepare smears from culture (Preparation and Fixation of Bacteria for Staining). To understand the principle of staining. To know the different types of staining techniques. Materials Clean glass slide. Inoculating loops. Pure culture. Sterile Distilled water. Bunsen burner or alcohol lamp. Absolute methanol. Background Smear is a distribution of bacterial cells on a slide for the purpose of viewing them under the microscope. Proper preparation of smear from samples or bacterial growth is important for adequate visualization of bacteria under routine bright-field microscopy. Bacteria cells are almost colorless , transparent and minute A staining technique is often applied to the cells to kill and color them so the their shape and size can be easily determined under the microscope Principle Stain (dye): is a salt composed of two ions, and one will contain the choromogen ( the colored part of the molecule). a) Positive ion( cation) b) Negative ion ( anion) Most dyes used are basic dyes with a positive chromogen - The interior of the cell (cell`s cytoplasm) is negatively charged. - The negative cytoplasm attracts the positively charged chromogen Chemically, a stain may be defined as an organic compound containing a benzene ring plus a chrmophore and auxohrome. MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. rev.0 Laboratory Manual in Diagnostic Microbiology 1 Benzene: organic colorless Chromogen: colored solvent compound, not stain chromophore: chemical group that impart color to benzene Auxochrome: chemical compound the conveys the property of ionization of the chromogen( ability to form salts) and bind to fibers or tissues STAIN Stains → combine chemically with the bacterial protoplasm. Commonly used stains are salts ( two ions and one will contain chromogen): Basic dyes: colored cation + colorless anione.g. methylene blue (methylene blue chloride)MB+ + ClAcidic dyes: colored anion + colorless cation e.g. eosin ( Na+ + eosin-). Bacterial cells are slightly negatively charged ( rich in nucleic acids bearing negative charges as phosphate groups)→ combine with positively charged basic dyes Acidic dyes do not stain the bacterial cell → can stain the background material with a contrasting color. Examples for acidic dyes (anionic): picric acid, Nigrosin, Eosin, and India ink. Examples of basic dyes (cationic): MB, S, CV, CF and MG. MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. rev.0 Laboratory Manual in Diagnostic Microbiology 1 Types of staining techniques Simple staining (use of a single stain) Direct (basic stain) Indirect (Negative or acidic stain) For visualization of morphological shape & arrangement. MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. rev.0 Differential staining (use of two contrasting stains separated by a decolorizing agent) Identification Gram stain Acid fast stain Visualization of structure Spore stain Capsule stain Laboratory Manual in Diagnostic Microbiology 1 Procedure 1. Take a clean glass slide and gently heat one side to remove any grease that may present. 2. Sterilize the wire loop. - There are two source of specimen (bacteria) either growing on 1. Solid media. 2. Liquid media Smear preparation :If source of specimen (bacteria growing) in solid media 3. Place a loop full of distilled water in the center of the slide. 4. With sterile wire loop pick a colony and emulsify in the drop of distilled water on the slide. 5. Lay the prepared smears on the table and allow drying by air. 6. Fix the smear with heat by passing the slides (with the smear side up) over flames 5 to 6 times. 7. Placing the slide on the staining rack and ready for staining. Smear preparation : If source of specimen (bacteria growing) in liquid media 3. Place directly a loop full of specimen in the center of the slide. 4. There is no need to mix such material with D.W unless the culture or material is stick. 5. Lay the prepared smears on the table and allow drying by air. 6. Fix the smear with heat by passing the slides (with the smear side up) over flames 5 to 6 times. 7. Placing the slide on the staining rack and ready for staining. MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. rev.0 Laboratory Manual in Diagnostic Microbiology 1 Experiment. No. 7 Direct staining Objectives 1. The student should perform the direct staining procedure. 2. The student should understand the morphology of bacteria. Materials Glass slides Bacterial culture Basic stain( Methylene blue or crystal violet) Loops Methanol or direct flaming Distilled water Background It is the use of single basic dye to color the bacterial organism. E.g. methylene blue, crystal violet, safranin. All bacteria take the color of the dye. Principle The direct staining technique stain the bacteria due ionic attraction Basic dyes: colored cation+ colorless anion. The negative charge is the most charge carried by the bacterial cell The attraction will occur after addition of basic stain Procedure 1. 2. 3. 4. 5. Prepare bacterial smear Allow to air dry and fix it Flood the bacterial smear with one of the basic dye for 1- 2 minute Wash off with tap water then blot the slide Examine under oil immersion lens MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. rev.0 Laboratory Manual in Diagnostic Microbiology 1 Experiment. No.8 Negative staining (Indirect) Objectives 1. The student should apply the negative staining technique. 2. The student should understand the morphology of bacteria. Materials Glass slides Acidic stains( Nigrosin or India ink) Slide dryer Capillary tubes Bacterial culture Loops Background This technique uses acidic stain Used to study the shape, morphology and arrangement The bacteria will appear colorless against a dark background. No heat fixation or strong chemicals are used→ the bacteria are less distorted than in other staining procedure. Example: Nigrosine , India ink Principle The negative staining technique does not stain the bacteria due ionic repulsion, but stain the background. Acidic dyes: colored anion + colorless cation. The negative charge is the most charge carried by the bacterial cell The repulsion will occur after addition of acidic stain Procedure 1. Place a small drop of nigrosin towards one end of a clean microscope slide. 2. Using your sterile inoculating loop, aseptically add a small amount of bacteria to the dye and mix gently with the loop. 3. Using the edge of another slide, spread the mixture with varying pressure across the slide so that there are alternating light and dark areas. Make sure the dye is not too thick or you will not see the bacteria! 4. Let the slide air dry completely on the slide. Do not heat fix and do not wash off the dye. 6. Observe using oil immersion microscopy. Find an area that has neither too much nor too little dye (an area that appears light purple where the light comes through the slide). If the dye is too thick, not enough light will pass through; if the dye is too thin, the background will be too light for sufficient contrast. MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. rev.0 Laboratory Manual in Diagnostic Microbiology 1 Experiment. No.9 Gram staining Objectives 1. The student should be able to perform the gram staining procedure properly. 2. The student should understand the principle of gram staining technique. 3. The student should differentiate between gram positive and gram negative bacteria. Materials Cultures of Staphylococcus aureus, Candida albican, Bacillus subtilis, E.coli Gram stain: Crystal violet (primary stain) Gram’s iodine (mordant) Acetone-alcohol (decolorizing agent) Safranin (counter stain) Glass slides Loops Distilled water Background It is the most important differential stain used in bacteriology because it classified bacteria into two major groups: gram positive (violet) and gram negative( red) It is based on the chemical and physical properties of their cell walls. Primarily, it detects peptidoglycan, which is present in a thick layer in Gram positive bacteria. A Gram positive results in a purple/blue color while a Gram negative results in a pink color. The Gram stain is almost always the first step in the identification of a bacterial organism, and is the default stain performed by laboratories over a sample when no specific culture is referred. While Gram staining is a valuable diagnostic tool in both clinical and research settings, not all bacteria can be definitively classified by this technique, thus forming Gram-variable and Gramindeterminate groups as well. The word Gram is always spelled with a capital, referring to Hans Christian Gram, the inventor of Gram staining. MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. rev.0 Laboratory Manual in Diagnostic Microbiology 1 Principle Gram-positive bacteria Have a thick peptidoglycan layer surrounds the cell. The stain gets trapped into this layer and the bacteria turned purple. The crystal violet and iodine combine to form a larger molecule that precipitates out within the cell. The alcohol/acetone mixture then causes dehydration of the multilayered peptidoglycan, thus decreasing the space between the molecules and causing the cell wall to trap the crystal violet-iodine complex within the cell and retain the color of primary stain Gram-negative bacteria Have a thin peptidoglycan layer that does not retain crystal violet stain. Instead, it has a thick lipid layer which dissolved easily upon decolorization with AcetonAlcohol. Therefore, cells will be counterstained with safranin and turned red. MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. rev.0 Laboratory Manual in Diagnostic Microbiology 1 Procedure Transfer a loopful of the liquid culture to the surface of a clean glass slide, and spread over a small area. Two to four cultures may be stained on the same slide, which can be divided into 2-4 sections with vertical red wax pencil lines. To stain material from a culture growing on solid media, place a loopful of tap water on a slide; using a sterile cool loop transfer a small sample of the colony to the drop, and emulsify. Allow the film to air dry. Fix the dried film by passing it briefly through the Bunsen flame two or three times without exposing the dried film directly to the flame. The slide should not be so hot as to be uncomfortable to the touch. 1. Flood the slide with crystal violet solution for up to one minute. Wash off briefly with tap water (not over 5 seconds). Drain. 2. Flood slide with Gram's Iodine solution, and allow to act (as a mordant) for about one minute. Wash off with tap water. Drain. 3. Remove excess water from slide and blot, so that alcohol used for decolorization is not diluted. Flood slide with 95% alcohol for 10 seconds and wash off with tap water. (Smears that are excessively thick may require longer decolorization. This is the most sensitive and variable step of the procedure, and requires experience to know just how much to decolorize). Drain the slide. 4. Flood slide with safranin solution and allow counterstaining for 30 seconds. Wash off with tap water. Drain and blot dry with bibulous paper. Do not rub. 5. All slides of bacteria must be examined under the oil immersion lens Note: To remove immersion oil from a slide without damaging the smear, lay a piece of lens tissue on the slide, add a drop or two of xylene and draw the lens tissue across the slide. Repeat if necessary. MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. rev.0 Laboratory Manual in Diagnostic Microbiology 1 Experiment. No. 10 Acid-fast staining (Ziehl-Neelsen and kinyoun) Objectives Each student should be able to 1. Understand the biochemical basis of the acid-fast stain. 2. Perform an acid-fast stain. 3. Differentiate bacteria into acid-fast and non-acid-fast groups. Materials Bacterial culture (E. coli and M. smegmatis). Ziehl-Neelsen stain (Carbol fuchsin, Acid alcohol, Loeffeler`s alkaline methylene blue). Glass slides, inoculating loop, immersion oil, staining racks, bibulous paper, towel paper Hot plate. Microscope Background In the Medical laboratory, the acid-fast stain is important in identifying bacteria in the genus Mycobacterium; specifically, M.leprae (leprosy) and M. tuberculosis (tuberculosis). This differential stain is also used to identify members of the aerobic actinomycete genus Nocardia; specifically, the opportunistic pathogens N. brasiliensis and N. asteroids that cause the lung disease nocardiosis. The waterborne protozoan parasite Cryptosporidium that causes diarrhea in humans (cryptosporidiosis) can also be identified by the acid-fast stain. Principle A few species of bacteria in the genera Mycobacterium and Nocardia, and the parasite Cryptosporidium do not readily stain with simple stains. However, these microorganisms can be stained by heating them with carbol fuchsin .The heat drives the stain into the cells. Once the microorganisms have taken up the carbol fuchsin, they are not easily decolorized by acidalcohol, and hence are termed acid-fast. This acid-fastness is due to the high lipid content (mycolic acid) in the cell wall of these microorganisms. The Ziehl-Neelsen acid-fast staining procedure (developed by Franz Ziehl, a German bacteriologist, and Friedrich Neelsen, a German pathologist, in the late 1800s) is a very useful differential staining technique that makes use of this difference in retention of carbol fuchsin. Acid-fast microorganisms will retain this dye and appear red (figure 9.1a, b). Microorganisms that are not acid-fast, termed non-acid-fast, will appear blue or brown due to the counterstaining with methylene blue after they have been decolorized by the acid-alcohol. A modification of this procedure that employs a wetting agent (Tergitol No. 7) rather than heat to ensure stain penetration is known as the Kinyoun staining procedure (developed by Joseph Kinyoun, German bacteriologist, in the early 1900s).Kinyoun carbol fuschsin has a greater concentration of phenol and basic fuchsin than Ziehl carbol fuschsin. MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. rev.0 Laboratory Manual in Diagnostic Microbiology 1 Figure 10.1 Ziehl-Neelsen Stain of Mycobacterium Acid-fast Rods. (a) Mycobacterium smegmatis stained red (×1,000). (b) In this photomicrograph, Mycobacterium smegmatis stains red and the background cells blue-brown. (a) (b) Procedure Ziehl-Neelsen (Hot Stain) Procedure: 1. Prepare a smear consisting of a mixture of E. coli and M. smegmatis. 2. Allow the smear to air dry and then heat-fix or by one or two drops of 70% v/v methanol or ethanol alcohol. 3. Place the slide on a hot plate that is within a chemical hood (with the exhaust fan on), and cover the smear with a piece of paper towelling that has been cut to the same size as the microscope slide. Saturate the paper with Ziehl’s carbol fuchsin (figure 10.2a). Heat for 3 to 5 minutes. Do not allow the slide to dry out, and avoid excess flooding! Also, prevent boiling by adjusting the hot plate to a proper temperature. A boiling water bath with a staining rack or loop held 1 to 2 inches above the water surface also works well. (Instead of using a hot plate to heat drive the carbol fuchsin into the bacteria, an alternate procedure is to cover the heat-fixed slide smegmatis. with a piece of paper towel. Soak the towel with the carbol fuchsin and heat, well above a Bunsen burner flame.). 4. Remove the slide, let it cool, and rinse with water for 30 seconds (figure 10.2b). 5. Decolorize by adding acid-alcohol drop by drop until the slide remains only slightly pink. This requires 10 to 30 seconds and must be done carefully (figure 10.2c). 6. Rinse with water for 5 seconds (figure 10.2d). 7. Counterstain with alkaline methylene blue or malachite green for about 2 minutes (figure 10.2e). 8. Rinse with water for 30 seconds (figure 10.2f). 9. Blot dry with bibulous paper. 10. There is no need to place a cover slip on the stained smear. 11. Examine the slide under oil immersion. MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. rev.0 Laboratory Manual in Diagnostic Microbiology 1 Figure 10.2 Acid-fast Staining Procedures. Kinyoun (Cold Stain) Procedure: (This may be used instead of or in addition to the Ziehl-Neelsen procedure.) 1. Prepare a smear as previously directed. 2. Flood the slide for 5 minutes with Kinyoun carbol fuchsin in prepared (heat is not necessary). 3. Decolorize with acid-alcohol and wash with tap water. Repeat this step until no more colour runs off the slide. 4. Counterstain with alkaline methylene blue for 2minutes. Wash and blot dry. 5. Examine under oil lens. Result Acid-fast bacteria (AFB)............................................................................................Red, straight or slightly curved rods, occurring singly or in small groups, may appear beaded. Cells …..........................................................................................................Green or blue Background material...................................................................................Green or blue MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. rev.0 Laboratory Manual in Diagnostic Microbiology 1 Experiment. No. 11 Endospore staining (Schaeffer-Fulton or wirtz-conklin) Objectives Each student should be able to 1. Understand the biochemistry underlying endospore staining 2. Perform an endospore stain 3. Differentiate between bacterial endospore and vegetative cell forms Materials 24- to 48-hour nutrient agar slant cultures of Bacillus megaterium (ATCC 12872). 5% malachite green solution, safranin. Glass slides, inoculating loop, immersion oil, staining racks, bibulous paper, paper towelling and forceps. Hot plateor boiling water bath. Microscope Background Only a few bacteria produce endospores. Those of medically importance include Bacillus anthracis (anthrax), Clostridium tetani (tetanus), C botulinium (botulism), and C. perfringens (gas gangrene). In the clinical laboratory, the location and size of endospores vary with the species; thus, they are often of value in identifying bacteria. Principle Bacteria in genera such as Bacillus and Clostridium produce quite a resistant structure capable of surviving for long periods in an unfavourable environment and then giving rise to a new bacterial cell (figure10.1). This structure is called an endospore since it develops within the bacterial cell. Endospores are spherical to elliptical in shape and may be either smaller or larger than the parent bacterial cell. Endospore position within the cell is characteristic and may be central, subterminal, or terminal. Endospore could not be stained easily, but, once stained, they strongly resist decolorization. This property is the basis of the Schaeffer-Fulton (Alice B. Schaeffer and MacDonald Fulton were microbiologists at Middlebury College, Vermont, in the 1930s) or WirtzConklin method (Robert Wirtz and Marie E. Conklin were bacteriologists in the early 1900s) of staining endospores. The endospores are stained with malachite green. Heat is used to provide stain penetration. The rest of the cell is the decolorized and counterstained a light red with safranin. Figure 11.1 The Life Cycle of Endospore-forming Bacteria. MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. rev.0 Laboratory Manual in Diagnostic Microbiology 1 Figure 11.2 Examples of Endospores. (a) Central spores of Bacillus stained with malachite green and counterstained with safranin(×1,000). Notice that the cells are rod-shaped and straight, often arranged in pairs or chains, with rounded squared ends. The endospores are oval and not more than one spore per cell. (b) Clostridium tetani showing round, terminal spores that usually distend the cell (×1,000). Notice that the cells are rod-shaped and are often arranged in pairs or short chains with rounded or sometimes pointed ends. (c) Bacillus megateriumshowing short oval to elongate spores. (a) (b) (c) Procedure Endospore Staining procedure: 1. With a wax pencil, place the names of the respective bacteria on the edge of four clean glass slides. 2. Aseptically transfer one species of bacterium with an inoculating loop to each of the respective slides, air dry (or use a slide warmer), and heat-fix. 3. Place the slide to be stained on a hot plate or boiling water bath equipped with a staining loop or rack. Cover the smear with paper towelling that has been cut the same size as the microscope slide. 4. Soak the paper with the malachite green staining solution. Gently heat on the hot plate (just until the stain steams) for 5 to 6 minutes after the malachite green solution begins to steam. Replace the malachite green solution as it evaporates so that the paper remains saturated during heating (figure11.3a). Do not allow the slide to become dry. 5. Remove the paper using forceps, allow the slide to cool, and rinse the slide with water for 30seconds (figure 11.3b). 6. Counterstain with safranin for 60 to 90 seconds (figure 11.3c). MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. rev.0 Laboratory Manual in Diagnostic Microbiology 1 7. Rinse the slide with water for 30 seconds (figure 11.3d). 8. Blot dry with bibulous paper (figure 11.3e) and examine under oil immersion. A cover slip is not necessary. Result The spores, both endospores and free spores.................................................................Green Vegetative cells stain…........................................................................................... Red (figure 11.4)Endospore-forming bacterium Bacillus subtilis [ MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. rev.0 Laboratory Manual in Diagnostic Microbiology 1 Experiment. No. 12 Identification of Staphylococci species Objectives Each student should be able to 1. Perform selected clinical procedures to isolate staphylococci from certain areas of the human body. 2. Perform selected clinical procedures that distinguish the pathogenic species of staphylococci from the non-pathogenic species. Materials Slant cultures of staphylococcus.aureus (ATCC 6538), staphylococcus.epidermidis (ATCC 12228) and staphylococcus.saprophyticus. Or Streak-plate cultures. Sterile Nutrient agar (NA). Sterile blood agar plate (BAP). Sterile mannitol salt agar plate (MSA). Sterile DNase agar plate. Citrated rabbit plasma tube (0.5 ml). Gram-staining material. Wax pencil. Inoculating loop, inoculating needle. Bunsen burner & vortex mixer (if available). 3% Hydrogen peroxide solution Background The genus Staphylococcus (staphylo, bunch of grapes) consists of gram-positive cocci, 0.5 to 1.5μm in diameter, usually in irregular clusters, within which pairs and tetrads are commonly seen. They are nonmotile and non sporing. Members of this genus are facultative anaerobic. Colonies are round, convex, mucoid, and adherent to the agar. They are chemoorganotrophic, requiring nutritionally rich media. Staphylococci have respiratory and fermentative metabolism, producing acid but no gas from carbohydrates. They are able to grow on nutrient agar with 5% NaCl and are usually positive for catalase. Oxidase negative members contain cytochromes and are Voges-Proskauer positive. Most species reduce nitrate to nitrite. Optimum growth is at 37°C. Staphylococci are commensals on the skin and in the human mouth and upper respiratory tract. They can be human pathogens .S. aureus (aureus, golden) is the most important clinical member of this genus. It may be isolated. From the skin or mucous membranes of the body. It can cause various infections (e.g., carbuncles, abscesses, pneumonia, endocarditis, food poisoning, toxic shock syndrome) throughout the body. In addition some of these staphylococci are resistant to penicillin. This resistance comes about when the bacteria produce penicillinase (ß-lactamase), which hydrolyzes the ß-lactam ring of penicillin. S. epidermidis (epidermidis, the outer skin) is anon-pathogenic member of this genus (It is part of the normal microbiota of the skin. Additionally, S. saprophyticus (sapro, putrid) can be isolated and may be responsible for urinary tract infections especially in females. MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. rev.0 Laboratory Manual in Diagnostic Microbiology 1 Principle Clinical tests for staphylococci are directed toward (1) Distinguish of the genus Staphylococcus from other gram-positive cocci (such as Micrococcus or Streptococcus) by catalase test. (2) Differentiate the species within the genus. To differentiate Between the three most commonly isolated Staphylococcus species. By coagulase test, DNase test. One of the most popular ways to isolate and identify and other gram-positive cocci of medical importance is through the use of blood agar plates. Haemolysis patterns are particularly useful in identification (figure 13.1). Mannitol salt agar also can be used for the selective isolation, cultivation, and enumeration of staphylococci from clinical and non clinical specimens. Mannitol-using bacteria (e.g., S. aureus) turn the medium yellow, whereas those that do not use mannitol (e.g., S. epidermidis, S. saprophyticus) produce no colour change (figure 13.1). Laboratory Diagnosis of staphylococcus species Infections 1.Specimen Depends on the type of infection. (Pus, joint aspirate, blood, sputum, stools. Urine). 2. Culture Staphylococcus spp are growing well on the most lab media that will support the growth of gram positive organisms. Within 24 hours smooth, circular colonies with a buttery consistency will grow. cultivate the specimen on a) Nutrient agar : on which it produces pigment: Golden yellow: Staphylococcus. aureus but many clinical isolates have a creamy or white pigmentation. White: Staphylococcus.epidermidis. Lemon yellow: Staphylococcus.saprophyticus. b) Blood agar plate (BAP): for haemolysis patterns Complete haemolysis (Beta haemolysis): Staph. sureus No hemolysis: Staph. epidermidis and Staph. Saprophyticus c) Mannitol salt agar MSA: Selective medium for isolating Staph. aureus from stool in case of food poisoning. Staph. aureus give yellow colour because of mannitol fermentation. MSA contains High salt (7.5%) inhibits the growth of most other organisms, but Staph.spp are facultative halophiles and can grow in up to 10% salt. MSA also contains mannitol and the pH indicator phenol red. If an organism growing on MSA ferments mannitol, the acid produced turns the colonies yellow .S. aureus ferments mannitol and S. epidermidis does not. MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. rev.0 Laboratory Manual in Diagnostic Microbiology 1 (Figure 12.1) growth pattern of Staphylococcus. aureus in culture media Nutrient agar Golden yellow endopigment Mannitol salts agar (MSA) MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. rev.0 Blood agar plate Beta haemolysis Laboratory Manual in Diagnostic Microbiology 1 3. Microscopy (In Direct Gram smear) Gram Stain Technique. Gram positive cocci in Clusters 4. Biochemical Reaction A. Catalase Test Principle This test is used to differentiate those bacteria that produce the enzyme catalase, such as staphylococci, from non-catalase producing bacteria such as streptococci. Procedure 1.Pour 2–3 ml of the hydrogen peroxide solution into a test tube. 2.Using a sterile wooden stick or a glass rod (not a nichrome wire loop), remove several colonies of the test organism and immerse in the hydrogen peroxide solution. Interpretation: Rapid effervescence (Air bubble) indicates oxygen production and a positive test. Positive Negative MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. rev.0 Laboratory Manual in Diagnostic Microbiology 1 B. Coagulase Test Principle: 1. Bound coagulase (clumping factor) which converts fibrinogen directly to fibrin without requiring a coagulase reacting factor. It can be detected by the clumping of bacterial cells in the rapid slide test. 2. Free coagulase which converts fibrinogen to fibrin by activating a coagulase-reacting factor present in plasma. Free coagulase is detected by clotting in the tube test. Procedure: 1. Bound coagulase: Homogenous suspension of the test organism is made in a drop of saline on a slide then mixed with a drop of undiluted human or rabbit plasma. 2. Free coagulase It is done by adding 5 drops of an overnight broth culture of the test organism to 0.5 ml of human or rabbit plasma diluted 1/10 in sterile saline. The tubes are incubated for 6-12 hours at 37 degree and inspected hourly for coagulation. Interpretation 1. Bound coagulase: Staphylococcus aureus clumps within 15 sec. because the clumping factor precipitates the fibrin in the plasma on the cell surface. + 2.Free coagulase Free coagulase is detected by clotting in the tube test. MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. rev.0 Laboratory Manual in Diagnostic Microbiology 1 Positive Negative C. DNAase Test Principle: This test is used to identify Staph. aureus as it produces DNAase enzyme. Procedure: The tested organism is cultured on a medium which contains DNA. After overnight incubation at 37°Cthe plate is flooded with weak HCL. The acid precipitates un hydrolysed DNA. Interpretation: DNAase producing colonies are surrounded by clear areas due to DNA hydrolysis. Differentiation within the Coagulase Negative Staphylococcus spp (CNS ) We usually only distinguish between the CNS on urinary tract isolates. For these isolates we want to distinguish between S. epidermidis and S. saprophyticus. By MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. rev.0 Laboratory Manual in Diagnostic Microbiology 1 Novobiocin (5ug disk) susceptibility test 1. S. epidermidis is sensitive, giving a zone of inhibition greater than or equal to 17 mm. in diameter in blood agar plate after incubation 24 hours at 37°C. 2. S. saprophyticus is resistant, giving a zone less than 17 mm. in diameter. MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. rev.0 Laboratory Manual in Diagnostic Microbiology 1 Experiment. No.13 Identification of Streptococci Objectives 1. The student should be able to identify different species of streptococci based on key reactions. 2. The student should perform the procedure of identification properly. 3. To understand the principle of each test. Materials Different strains of streptococci. Discs (bacitracin and optochin). S.aureus isolates. Forceps Swabs Media Background Characters of Streptococci – Gram positive cocci – 1µm in diameter – Chains or pairs – Usually capsulated – Non motile – Non spore forming – Facultative anaerobes – Fastidious – Catalase negative (Staphylococci are catalase positive) Streptococci can be classified according to: – Oxygen requirements Anaerobic (Peptostreptococcus) Aerobic or facultative anaerobic (Streptococcus) – Serology (Lanciefield Classification) – Hemolysis on Blood Agar (BA) Streptococci classified into many groups from A-K & H-V One or more species per group Classification based on C- carbohydrate antigen of cell wall – Groupable streptococci o A, B and D (more frequent) o C, G and F (Less frequent) – Non-groupable streptococci o S. pneumoniae (pneumonia) o viridans streptococci – e.g. S. mutans Causing dental carries MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. rev.0 Laboratory Manual in Diagnostic Microbiology 1 Hemolysis on BA – -hemolysis o Partial hemolysis o Green discoloration around the colonies o e.g. non-groupable streptococci (S. pneumoniae & S. viridans) – -hemolysis o Complete hemolysis o Clear zone of hemolysis around the colonies o e.g. Group A & B (S. pyogenes & S. agalactiae) – -hemolysis o No lysis o e.g. Group D (Enterococcus spp) Differentiation between -hemolytic streptococci The following tests can be used to differentiate between -hemolytic streptococci – Lanciefield Classification – Bacitracin susceptibility Test o Specific for S. pyogenes (Group A) – CAMP test o Specific for S. agalactiae (Group B) – Hippurate hydrolysis o Differentiates Group B streptococci from other beta hemolytic streptococci o Group B streptococci hydrolyzes sodium hippurate Differentiation between -hemolytic streptococci The following definitive tests used to differentiate between S. pneumoniae & viridans streptococci – Optochin Test – Bile Solubility Test – Inulin Fermentation Identification of Group D streptococci Bile Esculin hydrolysis – Ability to grow in 40% bile and hydrolyze Esculin are features of streptococci that possess Group D antigen. Growth in 6.5% NaCl broth – Differentiates Group D streptococci from enterococci PYR test: – for Group A and D MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. rev.0 Laboratory Manual in Diagnostic Microbiology 1 Principle Bacitracin Sensitivity – Bacitracin test is used for presumptive identification of group A – To distinguish between S. pyogenes (susceptible to B) & non group A such as S. agalactiae (Resistant to B) – Bacitracin will inhibit the growth of gp A Strep. pyogenes giving zone of inhibition around the disk CAMP test – Group B streptococci produce extracellular protein (CAMP factor) – CAMP act synergistically with staph. -lysin to cause lysis of RBCs Trimethoprim sulfamethoxazole (SXT) – Inhibits beta-hemolytic streptococcal groups other than A and B Optochin susceptibility test – Optochin (OP) test is presumptive test that is used to identify S. pneumoniae – S. pneumoniae is inhibited by Optochin reagent (<5 µg/ml) giving a inhibition zone ≥14 mm in diameter. Bile solubility test – S. pneumoniae produce a self-lysing enzyme to inhibit the growth – The presence of bile salt accelerate this process PYR hydrolysis – Substrate L-pyrrolidonyl-b-napthlyamide (PYR) is hydrolyzed by Group A Streptococci and Enterococcus sp. – As specific as 6.5% NaCl broth for Enterococcus sp. – More specific than Bacitracin for Group A streptococci . MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. rev.0 Laboratory Manual in Diagnostic Microbiology 1 Procedure Bacitracin test – – – Inoculate BAP with heavy suspension of tested organism Bacitracin disk (0.04 U) is applied to inoculated BAP After incubation, any zone of inhibition around the disk is considered as susceptible. CAMP test – Single streak of Streptococcus to be tested and a Staph. aureus are made perpendicular to each other – 3-5 mm distance was left between two streaks – After incubation, a positive result appear as an arrowhead shaped zone of complete hemolysis – S. agalactiae is CAMP test positive while non gp B streptococci are negative. Optochin test – – – BAP inoculated with organism to be tested OP disk is placed on the center of inoculated BAP After incubation at 37oC for 18 hrs, accurately measure the diameter of the inhibition zone by the ruler – ≥14 mm zone of inhibition around the disk is considered as positive and ≤13 mm is considered negative. S. pneumoniae is positive (S) while S. viridans is negative (R). Bile solubility test – – – – – – Add ten parts (10 ml) of the broth culture of the organism to be tested to one part (1 ml) of 2% Na deoxycholate (bile) into the test tube Negative control is made by adding saline instead of bile to the culture Incubate at 37oC for 15 min Record the result after 15 min Positive test appears as clearing in the presence of bile while negative test appears as turbid S. pneumoniae soluble in bile whereas S. viridans insoluble MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. rev.0 Laboratory Manual in Diagnostic Microbiology 1 Experiment. No 14 Disinfection and Sterilization techniques Objectives 1. To understand the differences between sterilization and disinfection. 2. To know the different types of sterilization and disinfection. Background Disinfection: Reducing the number of viable microorganisms present in inanimate objects Sterilization is the killing of all microorganisms in a material or on the surface of an object. A disinfectant is a chemical or physical agent that is applied to inanimate objects to kill microbes. Antiseptic is a chemical agent that is applied to living tissue to kill microbes. Common Chemical Disinfectants 1. Chlorine Compounds (Halogens) Generally used in the form of sodium hypochlorite. Less suitable in the presence of organic matter (such as blood). Concentration must be increased to retain action (0.5%). High concentrations corrode metal surfaces, and bleach and damage fabrics. Bleach solution is corrosive and will corrode stainless steel surfaces 2. Alcohols Ethanol (80% v/v ethyl alcohol) or 2-propanol (60-70% v/v iso-propyl alcohol) solutions are used to disinfect skin and decontaminate clean surfaces. Methanol is poor disinfectant. Most effective at 70% in water ( water will enhance the protein denaturation) Skin irritant, volatile (evaporates rapidly), inflammable. 3. Iodine (Halogens) Iodine vapor is highly toxic and is absorbed through the skin. Iodine is used in alcoholic solution. Stains skin and may cause irritation. Most commonly used for skin disinfection and decontaminating clean surfaces. They are rapidly inactivated in the presence of organic matter. Iodine is corrosive and staining. MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. rev.0 Laboratory Manual in Diagnostic Microbiology 1 4. Formaldehyde(Aldehydes) Formalin is 37% w/v formaldehyde gas in water. 13% v/v formalin is a good decontaminant (but has an irritating odor). 5. Glutaraldehyde (Aldehydes) Glutaraldehyde is commercially available as 2% w/v aqueous solution which must be made alkaline to "activate" (e.g. by addition of 0.3% sodium bicarbonate). 6. Chorohexidine Chlorhexidine as chlorhexidinegluconate is dissolved in 70% alcohol. Use as antiseptic. 7. Hydrogen Peroxide(oxidizing agents) A concentration of 3% w/v generally used for disinfection. 8. Ethylene oxide (EO): It is an alkylating agent. It is highly toxic, irritating to eyes, skin, highly flammable, mutagenic and carcinogenic. 9. Phenolics Synthetic phenolics (clear soluble fluids) can be used as general disinfectants in the laboratory. Active in presence of organic matter. Use for disinfecting floors, walls, benches and other furniture. 5 % phenol, 1-5% Cresol, 5% Lysol (a saponified cresol), hexachlorophene, chlorhexidine, chloroxylenol(Dettol) It is toxic, corrosive and skin irritant. Chlorhexidine is inactivated by anionic soaps. Chloroxylenol is inactivated by hard water. 10. Quaternary Ammonium Compounds Quaternary ammonium compounds are positively charged (cationic) surface-active disinfectants. Effective against Gram-positive bacteria and lipid-containing viruses. Not recommended as general disinfectants (they have a narrow antibacterial spectrum). Inactivated by proteins, soap and anionic detergents. 11. Dyes: Acridine dyes are bactericidal because of their interaction with bacterial nucleic acids. Examples: Aniline dyes such as crystal violet, malachite green and brilliant green. Acridine 12. Heavy metals: They are bacteriostatic. E.g. Mercuric chloride, silver nitrate, copper sulfate, organic mercury salts. MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. rev.0 Laboratory Manual in Diagnostic Microbiology 1 Spriocidal disinfectant 1. 2. 3. 4. 5. 6. Glutaraldehyde (Aldehydes) Formaldehyde (Aldehydes) Ethylene oxide Hypochlorites Hydrogen peroxides Peracetic acids PHYSICAL METHODS OF STERILIZATION: Sunlight: The microbicidal activity of sunlight is mainly due to the presence of ultra violet rays in it. It is responsible for spontaneous sterilization in natural conditions. In tropical countries, the sunlight is more effective in killing germs due to combination of ultraviolet rays and heat. By killing bacteria suspended in water, sunlight provides natural method of disinfection of water bodies such as tanks and lakes. Sunlight is not sporicidal, hence it does not sterilize. Heat: Heat is considered to be most reliable method of sterilization of articles that can withstand heat. Heat acts by oxidative effects as well as denaturation and coagulation of proteins. Those articles that cannot withstand high temperatures can still be sterilized at lower temperature by prolonging the duration of exposure. Action of heat: Dry heat acts by protein denaturation, oxidative damage and toxic effects of elevated levels of electrolytes. The moist heat acts by coagulation and denaturation of proteins. Moist heat is superior to dry heat in action. Temperature required to kill microbe by dry heat is more than the moist heat. Thermal death time is the minimum time required to kill a suspension of organisms at a predetermined temperature in a specified environment. DRY HEAT: Red heat: Articles such as bacteriological loops, straight wires, tips of forceps and searing spatulas are sterilized by holding them in Bunsen flame till they become red hot. This is a simple method for effective sterilization of such articles, but is limited to those articles that can be heated to redness in flame. Flaming: This is a method of passing the article over a Bunsen flame, but not heating it to redness. Articles such as scalpels, mouth of test tubes, flasks, glass slides and cover slips are passed through the flame a few times. Even though most vegetative cells are killed, there is no guarantee that spores too would die on such short exposure. This method too is limited to those articles that can be exposed to flame. Cracking of the glassware may occur. Incineration: This is a method of destroying contaminated material by burning them in incinerator. Articles such as soiled dressings; animal carcasses, pathological material and bedding etc should be subjected to incineration. This technique results in the loss of the article, hence is suitable only for those articles that have to be disposed. Burning of polystyrene materials emits dense smoke, and hence they should not be incinerated. Hot air oven: This method was introduced by Louis Pasteur. Articles to be sterilized are exposed to high temperature (160o C) for duration of one hour in an electrically heated oven. Since air is poor conductor of heat, even distribution of heat throughout the chamber is achieved by a fan. The heat is transferred to the article by radiation, conduction and convection. The oven should be fitted with a thermostat control, temperature indicator, meshed shelves and must have adequate insulation. Articles sterilized: Metallic instruments (like forceps, scalpels, and scissors), glass wares (such as petri-dishes, pipettes, flasks, all-glass syringes), swabs, oils, grease, petroleum jelly and some MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. rev.0 Laboratory Manual in Diagnostic Microbiology 1 pharmaceutical products. Sterilization process: Articles to be sterilized must be perfectly dry before placing them inside to avoid breakage. Articles must be placed at sufficient distance so as to allow free circulation of air in between. Mouths of flasks, test tubes and both ends of pipettes must be plugged with cotton wool. Articles such as petri dishes and pipettes may be arranged inside metal canisters and then placed. Individual glass articles must be wrapped in kraft paper or aluminum foils. Sterilization cycle: This takes into consideration the time taken for the articles to reach the sterilizing temperature, maintenance of the sterilizing temperature for a defined period (holding time) and the time taken for the articles to cool down. Different temperature-time relations for holding time are 60 minutes at 160oC, 40 minutes at 170oC and 20 minutes at 180oC. Increasing temperature by 10 degrees shortens the sterilizing time by 50 percent. The hot air oven must not be opened until the temperature inside has fallen below 60oC to prevent breakage of glass wares. Sterilization control: Three methods exist to check the efficacy of sterilization process, namely physical, chemical and biological. Advantages: It is an effective method of sterilization of heat stable articles. The articles remain dry after sterilization. This is the only method of sterilizing oils and powders. Disadvantages: �since air is poor conductor of heat, hot air has poor penetration. � Cotton wool and paper may get slightly charred. � Glasses may become smoky. � Takes longer time compared to autoclave. Infra-red rays: Infrared rays bring about sterilization by generation of heat. Articles to be sterilized are placed in a moving conveyer belt and passed through a tunnel that is heated by infrared radiators to a temperature of 180oC. The articles are exposed to that temperature for a period of 7.5 minutes. Articles sterilized included metallic instruments and glassware. It is mainly used in central sterile supply department. It requires special equipment, hence is not applicable in diagnostic laboratory. MOIST HEAT: Moist heat acts by coagulation and denaturation of proteins. At temperature below 100oC: Pasteurization: This process was originally employed by Louis Pasteur. Currently this procedure is employed in food and dairy industry. There are two methods of pasteurization, the holder method( batch method) (heated at 63oC for 30 minutes) and flash method (heated at 72oC for 15 seconds) followed by quickly cooling to 13oC. Other pasteurization methods include Ultra-High Temperature (UHT), 140oC for 15 sec and 149oC for 0.5 sec. This method is suitable to destroy most milk borne pathogens like Salmonella, Mycobacteria, Streptococci, Staphylococci and Brucella, however Coxiella may survive pasteurization. Efficacy is tested by phosphatase test and methylene blue test. At temperature 100oC: Boiling: Boiling water (100oC) kills most vegetative bacteria and viruses immediately. Certain bacterial toxins such as Staphylococcal enterotoxin are also heat resistant. Some bacterial spores are resistant to boiling and survive; hence this is not a substitute for sterilization. The killing activity can be enhanced by addition of 2% sodium bicarbonate. When absolute sterility is not required, certain metal articles and glasswares can be disinfected by placing them in boiling water for 10-20 minutes. The lid of the boiler must not be opened during the period. Steam at 100oC: Instead of keeping the articles in boiling water, they are subjected to free steam at 100oC. MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. rev.0 Laboratory Manual in Diagnostic Microbiology 1 The steam that is generated sterilizes the articles when exposed for a period of 90 minutes. Media such as TCBS, DCA and selenite broth are sterilized by steaming. Sugar and gelatin in medium may get decomposed on autoclaving; hence they are exposed to free steaming for 20 minutes for three successive days. This process is known as tyndallisation(after John Tyndall) or fractional sterilization or intermittent sterilization. The vegetative bacteria are killed in the first exposure and the spores that germinate by next day are killed in subsequent days. The success of process depends on the germination of spores. At temperature above 100oC: Autoclave: Sterilization can be effectively achieved at a temperature above 100oC using an autoclave. Water boils at 100oC at atmospheric pressure, but if pressure is raised, the temperature at which the water boils also increases. In an autoclave the water is boiled in a closed chamber. As the pressure rises, the boiling point of water also raises. At a pressure of 15 lbs inside the autoclave, the temperature is said to be 121oC. Exposure of articles to this temperature for 15 minutes sterilizes them. To destroy the infective agents associated with spongiform encephalopathies (prions), higher temperatures or longer times are used; 135oC or 121oC for at least one hour are recommended. Advantages of steam: It has more penetrative power than dry air, it moistens the spores (moisture is essential for coagulation of proteins), condensation of steam on cooler surface releases latent heat, and condensation of steam draws in fresh steam. Different types of autoclave: Simple “pressure-cooker type” laboratory autoclave, Steam jacketed downward displacement laboratory autoclave and high pressure pre-vacuum autoclave RADIATION: Two types of radiation are used, ionizing and non-ionizing. Non-ionizing rays are low energy rays with poor penetrative power while ionizing rays are high-energy rays with good penetrative power. Since radiation does not generate heat, it is termed "cold sterilization". In some parts of Europe, fruits and vegetables are irradiated to increase their shelf life up to 500 percent. Ionizing radiation: Gamma rays Non-ionizing: UV lights It is used commercially to sterilize disposable petri dishes, plastic syringes, antibiotics, vitamins, hormones, syringes, gloves, dressing packs, foods and pharmaceuticals, glasswares and fabrics. FILTRATION: Filtration does not kill microbes, it separates them out. Membrane filters with pore sizes between 0.2-0.45 μm are commonly used to remove particles from solutions that can't be autoclaved. It is used to remove microbes from heat labile liquids such as serum, antibiotic solutions, sugar solutions, urea solution. Various applications of filtration include removing bacteria from ingredients of culture media, preparing suspensions of viruses and phages free of bacteria, measuring sizes of viruses, separating toxins from culture filtrates, counting bacteria, clarifying fluids and purifying hydatid fluid. Filtration is aided by using either positive or negative pressure using vacuum pumps. The older filters made of earthenware or asbestos are called depth filters. SONIC AND ULTRASONIC VIBRATIONS: Sound waves of frequency >20,000 cycle/second kills MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. rev.0 Laboratory Manual in Diagnostic Microbiology 1 bacteria and some viruses on exposing for one hour. Microwaves are not particularly antimicrobial in themselves, rather the killing effect of microwaves are largely due to the heat that they generate. MLT-Lab Manual, 1433-1434 H Dec. 29, 2012. rev.0