Insulin Admin - Pitfalls & Perils
advertisement

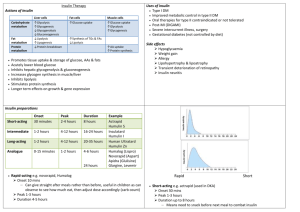
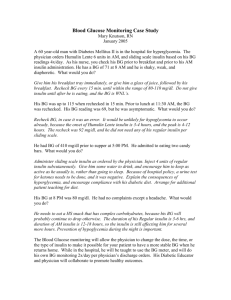
Chris Harrold SpR Diabetes & Endocrinology Diabetes 15% of all inpatients 50% of those are on insulin 20% of patients experienced an insulin error National Inpatient survey 2011 NPSA is common 16th June 2010 Right insulin Right dose Right time Right route Intermediate & Long: BNF has 25 listed insulins All U100 Does not list Humulin R U500 Short: Hypurin Bovine Normal Hypurin Porcine Normal Actrapid Humulin S Insuman Rapid Novorapid Apidra Humalog Levemir Lantus Hypurin Bovine Lente Hypurin Bovine Isophane Hypurin Porcine Isophane Insulatard Humulin I Insuman Basal Hypurin Bovine Protamine Zinc Mixed / Biphasic: Novomix 30 Humalog Mix 25 Humalog Mix 50 Hypurin Porcine 30/70 Humulin M3 Insuman Comb 15 Insuman Comb 25 Insuman Comb 50 Right insulin: Which humulin is this? Humulin I Humulin 3 Humulin M3 Right insulin: Insulin is the only drug prescribed by brand name Insulin detemir Insulin aspart Insulin glulisine Insulin lispro Right Dose Abbreviations “U” and “IU” are NEVER to be used Can be misread as 0 Deaths have occurred from misreading & misadministering doses Right Right time for the right insulin time: Mixed insulins – Breakfast and evening meal Short / rapid insulins – Mealtimes Long / intermediate – Bedtime (and breakfast) Not always true! Factors beyond our control (i.e. Nurses) Right Insulin: Brand name, not generic Right Dose: Clearly written Changes dated and initialled DO NOT USE “U” or “IU” Right time: Mixed insulins – Breakfast and evening meal Short / rapid insulins – Mealtimes Long / intermediate – Bedtime (and breakfast) Right Way: Prefilled (disposable) or 3ml Cartridges Lantus / Apidra – Solostar Novorapid / Novomix 30 / Levemir – Flexpen Humalog / Humalog Mix – Kwikpen www.diabetes.nhs.uk/safu_use_of_insulin Indications: Keto-acidosis – fixed rate infusion Diabetic Ketosis Pre-operative If no more than one meal will be missed (brief starvation) then manage with adaptations to usual regimen. Sick patients who are not eating and drinking General rules: If they can eat and drink they should not be on VRII Continue long acting insulin (Lantus / Levemir) if already taking. Should not be stopped except when converting back to usual treatment (e.g. SC insulin) Give SC insulin (rapid / mixed) with meal, then stop sliding scale after 30-60 minutes. Hypoglycaemia “4 is the floor” 15-20g fast carbohydrate Recheck after 15 mins and retreat as needed Replace carbohydrate Look for a cause! Usually sulfonylureas (dirty drugs) Metformin & gliptins do not cause hypos If not able to take orally / unconscious IV 10% dextrose (160mls over 10 mins) Not 50% IM glucagon 1mg (single dose) Hyperglycaemia Type 1 or type 2 How high? Why high? Steroids, sepsis, missed / omitted insulin Treat the patient (not the nurse) 4-6 units of Novorapid (or patients usual fast) Not Actrapid (oxymoron) 1 unit corrects by ~ 3 mmol/l Look at why and how it can be prevented Dose Watch for trends and look for causes Avoid reflex dose adjustments Allow sufficient time to see results Hyperglycaemia Adjustment Increase dose of appropriate insulin by 10% E.g. 20 units 22 units, 60 units 66 units Hypoglycaemia Reduce does of appropriate insulin by 20% Renal eGFR <30 is the cut off for: Metformin Gliclazide What is safe? failure: Saxagliptin (to eGFR 15) Repaglinide Insulin Stop the unsafe drugs, monitor and treat if needed. 4 full time OP clinics Antenatal Ward referrals Inappropriate referrals (sort it yourselves) Dose adjustment of insulin for hyper / hypoglycaemia Dose adjustment of oral medication If you ask for our help, take it. Diabetes Nurses / SpRs / Consultants www.diabetes.nhs.uk www.diabetes.nhs.uk/safe_use_of_insulin www.diabetesbible.com www.mims.co.uk