File - melanie boney
advertisement
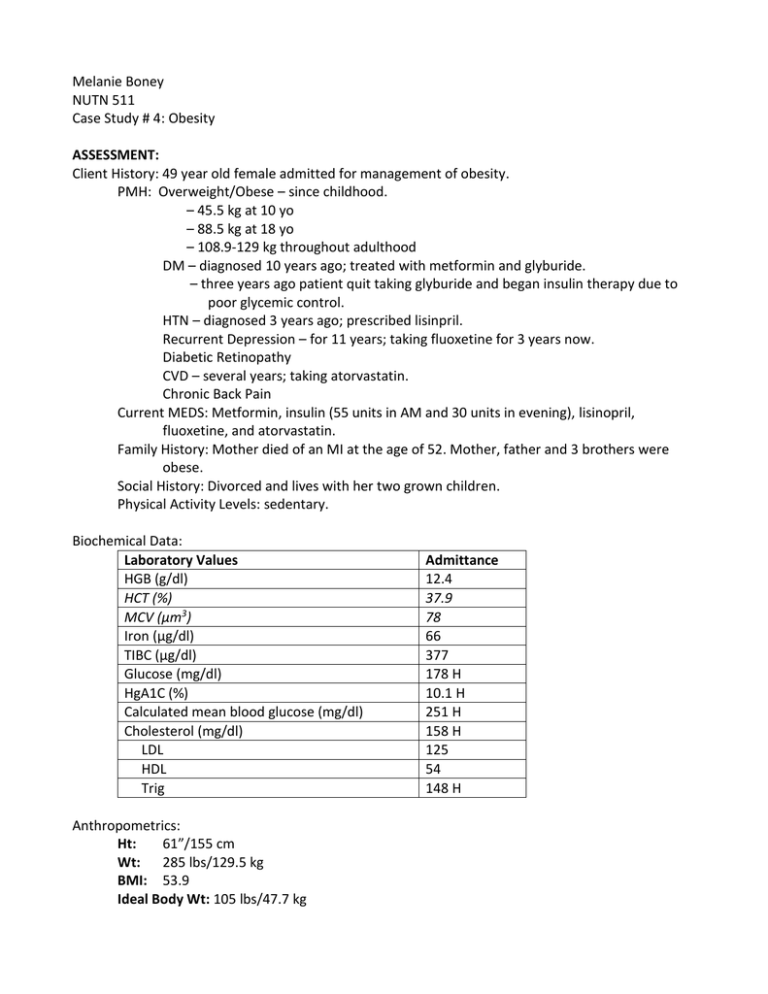
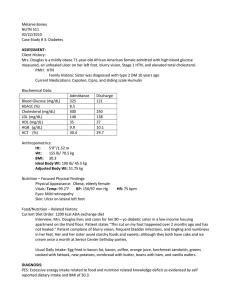
Melanie Boney NUTN 511 Case Study # 4: Obesity ASSESSMENT: Client History: 49 year old female admitted for management of obesity. PMH: Overweight/Obese – since childhood. – 45.5 kg at 10 yo – 88.5 kg at 18 yo – 108.9-129 kg throughout adulthood DM – diagnosed 10 years ago; treated with metformin and glyburide. – three years ago patient quit taking glyburide and began insulin therapy due to poor glycemic control. HTN – diagnosed 3 years ago; prescribed lisinpril. Recurrent Depression – for 11 years; taking fluoxetine for 3 years now. Diabetic Retinopathy CVD – several years; taking atorvastatin. Chronic Back Pain Current MEDS: Metformin, insulin (55 units in AM and 30 units in evening), lisinopril, fluoxetine, and atorvastatin. Family History: Mother died of an MI at the age of 52. Mother, father and 3 brothers were obese. Social History: Divorced and lives with her two grown children. Physical Activity Levels: sedentary. Biochemical Data: Laboratory Values HGB (g/dl) HCT (%) MCV (μm3) Iron (μg/dl) TIBC (μg/dl) Glucose (mg/dl) HgA1C (%) Calculated mean blood glucose (mg/dl) Cholesterol (mg/dl) LDL HDL Trig Anthropometrics: Ht: 61”/155 cm Wt: 285 lbs/129.5 kg BMI: 53.9 Ideal Body Wt: 105 lbs/47.7 kg Admittance 12.4 37.9 78 66 377 178 H 10.1 H 251 H 158 H 125 54 148 H Nutrition – Focused Physical Findings: Physical Appearance: Obese Vitals: BP: 156/93 mm Hg Eyes: Retinopathy Skin: Folliculitis beneath a grade 2 abdominal pannus Food/Nutrient-related Hx: The patient has successfully lost weight on more than 10 separate occasions through diet and exercise but always regained the weight within 2 – 3 years. Her sedentary lifestyle is a result of her chronic back pain. Usual Dietary Intakes: She eats large portions of calorically dense foods during her three daily meals and has a mid-afternoon snack; sometimes she skips lunch. She frequently eats at fastfood restaurants. DIAGNOSIS: Obesity related to excessive oral food/beverage intake as evidenced by high HgA1C percentage, high BMI, elevated triglycerides, and self-reported usual daily intakes. INTERVENTIONS: Nutrition Education: An initial session will be conducted with the patient for 60 minutes and then three 45 minute follow-up visits will be scheduled over 6 months. Counseling sessions will focus on weight loss strategies, reduced energy and fat intake, consistent carbohydrate, simplified meal plans, healthy food choices, individualized meal planning strategies, exchange lists, and insulin-tocarbohydrate ratios. Daily intake pattern based on ADA Dietary Recommendations: Estimated nutrient needs: Recommended kcal intake for wt loss: 1700 [(25 kcals/kg) – 1000] Protein: 130 grams (30%) [1 g/kg] Fat: 42 grams (22%) with less than 7% from saturated fat Carbohydrate: 205 grams (48%) with at least half whole grains Breakfast 55 grams Lunch 60 grams Dinner 60 grams Snacks (2 per day) <15 grams for each snack Total = ~205 grams EAL guidelines are listed below. Realistic Weight Goals: Individualized goals of weight loss therapy should be to reduce body weight at an optimal rate of 1-2 lbs per week for the first 6 months and to achieve an initial weight loss goal of up to 10% from baseline. These goals are realistic, achievable, and sustainable. Sodium Intake: Dietary sodium intake should be limited to no more than 2300 mg sodium (100 mmol) per day. Reduction of dietary sodium to recommended levels lowers systolic blood pressure by approximately 2 - 8 mmHg. CVD and Cardioprotective Nutrition Interventions: Cardioprotective nutrition interventions for prevention and treatment of CVD include reduction in saturated and trans fats and dietary cholesterol, and interventions to improve blood pressure. Studies in persons with diabetes utilizing these interventions report a reduction in cardiovascular risk and improved cardiovascular outcomes. Carbohydrate Intake Consistency: In persons on either MNT alone, glucose-lowering medications or fixed insulin doses, meal and snack carbohydrate intake should be kept consistent on a day-to-day basis. Consistency in carbohydrate intake results in improved glycemic control. Coordination of Care: The RD should implement MNT and coordinate care with an interdisciplinary team. Weight loss and weight maintenance therapy should be based on a comprehensive weight management program including diet, physical activity, physical and/or occupational therapy, and behavior therapy. The combination of therapies is more successful than using any one intervention alone. References: American Dietetic Association Evidence Analysis Library. Adult Weight Management Guideline: Executive Summary of Recommendations. https://www.adaevidencelibrary.com/topic.cfm?cat=3014 Accessed March 10, 2010. American Dietetic Association Evidence Analysis Library. Diabetes Mellitus (DM) Type 1 and 2Evidence-based Nutrition Practice Guideline for Adults http://www.adaevidencelibrary.com/topic.cfm?cat=2651. Accessed March 10, 2010. American Dietetic Association Evidence Analysis Library. Nutrition Guidelines: Disorders of Lipid Metabolism. http://www.adaevidencelibrary.com/topic.cfm?cat=2651. Accessed February 12, 2010. Escott-Stump, Sylvia and Mahan, Kathleen L.; Krause’s Food, Nutrition, & Diet Therapy 11th Edition. Elsevier, USA, 2004. Escott-Stump, Sylvia; Nutrition and Diagnosis-Related Care 6th Edition; Lippincott Williams & Wilkins, USA, 2008. Jeffery R, Drewnowski A, Epstein L, Stunkard A, Wilson G, Wing R. Long-term maintenance of weight loss: current status. Health Psychol. 2000;19:5-16. Wolever TMS, Hamad S, Chiasson JL, Josse RG, Leiter LA, Rodger NW, Ross SA, Ryan EA. Day-to-day consistency in amount and source of carbohydrate intake associated with improved glucose control in type 1 diabetes. J Amer Coll Nutr. 1999;18:242-247.