Connective tissue
advertisement

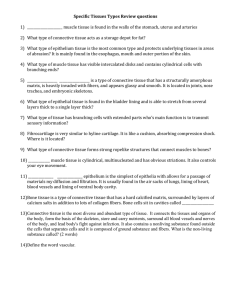
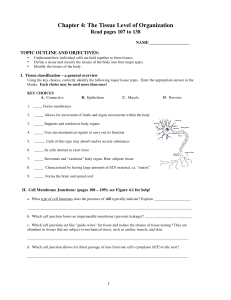
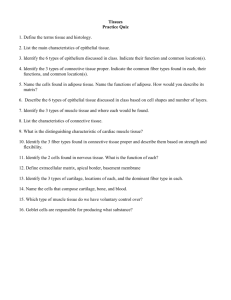
PowerLecture: Chapter 4 Tissues, Organs, and Organ Systems Learning Objectives Understand the various levels of animal organization (cells, tissues, organs, and organ systems). Know the characteristics of the various types of tissues. Know the types of cells that compose each tissue type and cite some examples of organs that contain significant amounts of each tissue type. Describe how the four principal tissue types are organized into an organ such as the skin. Learning Objectives (cont’d) Explain how the human body maintains a rather constant internal environment despite changing external conditions. Impacts/Issues Stem Cells Stem Cells Stem cells are the first to form when a fertilized egg starts dividing. Adults have stem cells in some tissues such as bone marrow and fat; these cells have shown some promise as therapy. Embryonic stem cells can be coaxed to differentiate into many different types of cells, which can replace damaged or worn out body cells perhaps to an extent greater than adult stem cells. Stem Cells The human body is an orderly assembly of parts (anatomy). A tissue is an aggregation of cells and intracellular substances functioning for a specialized activity. Various types of tissues can combine to form organs, such as the heart. Organs may interact to form organ systems such as the digestive system. Homeostasis allows for the stable functioning (physiology) of all our combined parts. How Would You Vote? To conduct an instant in-class survey using a classroom response system, access “JoinIn Clicker Content” from the PowerLecture main menu. Should researchers be allowed to start embryonic stem cell lines from human embryos that are not used for in vitro fertilization? a. Yes, most unimplanted embryos are destroyed anyway; the potential of stem cells is too great to ignore. b. No, any human embryo has the potential to become a human and so deserves protection from destruction. Section 1 Epithelium: The Body’s Covering and Linings Epithelium Epithelial tissue covers the surface of the body and lines its cavities and tubes. One surface is free and faces either the environment or a body fluid; the other adheres to a basement membrane, a densely packed layer of proteins and polysaccharides. Cells are linked tightly together; there may be one or more layers. free surface of epithelium simple squamous epithelium basement membrane connective tissue Fig. 4.1a, p. 69 Epithelium There are two basic types of epithelia. Simple epithelium is a single layer of cells functioning as a lining for body cavities, ducts, and tubes. • • Simple epithelium functions in diffusion, secretion, absorption, or filtering of substances across the cell layer. Pseudostratified epithelium is a single layer of cells that looks like a double layer; most of the cells are ciliated; examples are found in the respiratory passages and reproductive tracts. Stratified epithelium has many layers—as in human skin. Table 4.1, p. 68 Epithelium Both simple and stratified epithelium can be subdivided into groups based on shape at the tissue surface: • Squamous epithelium consists of flattened cells; examples are found in the lining of the blood vessels. • Cuboidal epithelium has cube-shaped cells; examples are found in glands. • Columnar epithelium has elongated cells; examples are found in the intestine. cilia columnar cells basement membrane TYPE: Simple squamous TYPE: Simple cuboidal DESCRIPTION: FrictionDESCRIPTION: Single layer reducing slick, single layer of of squarish cells flattened cells COMMON LOCATIONS: COMMON LOCATIONS: Ducts, secretory part of Lining of blood and lymph small glands; retina; kidney vessels, heart; air sacs of tubules; ovaries, testes; lungs; peritoneum bronchioles FUNCTION: Diffusion; filtration; secretion of lubricants FUNCTION: Secretion; absorption TYPE: Simple columnar DESCRIPTION: Single layer of tall cells; free surface may have cilia, mucus-secreting glandular cells, microvilli COMMON LOCATIONS: Glands, ducts; gut; parts of uterus; small bronchi FUNCTION: Secretion; absorption; ciliated types move substances Fig. 4.2b-d, p. 70 Epithelium Glands develop from epithelium. Glands are secretory structures derived from epithelium that make and release specific substances, such as mucus. Glands are classified according to how their products reach the site where they are used. • • Exocrine glands often secrete through ducts to free surfaces; they secrete mucus, saliva, earwax, milk, oil, and digestive enzymes for example. Endocrine glands have no ducts but distribute their hormones via the blood. Section 2 Connective Tissue: Binding, Support, and Other Roles Connective Tissue Connective tissue binds together, supports, and anchors body parts; it is the most abundant tissue in the body. Fibrous connective tissues and specialized connective tissues are both found in the body. Fiber-like structural proteins and polysaccharides secreted by the cells make up a matrix (ground substance) around the cells that can range from hard to liquid. Connective Tissue Fibrous connective tissues are strong and stretchy. Fibrous connective tissue takes different forms depending on cell type and the fibers/matrix produced. Loose connective tissue collagenous fiber fibroblast elastic fiber Dense, irregular connective tissue collagenous fibers Dense, regular connective tissue collagenous fibers Cartilage ground substance with collagen fibers fibroblast cartilage cell (chondrocyte) Fig. 4.2a-d, p. 70 Connective Tissue Types and examples of fibrous connective tissue: • Loose connective tissue supports epithelia and organs, and surrounds blood vessels and nerves; it contains few cells and loosely arrayed thin fibers. • Dense, irregular connective tissue has fewer cells and more fibers, which are thick; it forms protective capsules around organs. • Dense, regular connective tissue has bundled collagen fibers lying in parallel; such arrangements are found in ligaments (binding bone to bone) and tendons (binding muscle to bone). • Elastic connective tissue contains fibers of elastin; this tissue is found in organs that must stretch, like the lungs. Connective Tissue Cartilage, bone, adipose tissue, and blood are specialized connective tissues. Cartilage contains a dense array of fibers in a rubbery ground substance; cartilage can withstand great stress but heals slowly when damaged. • • • Hyaline cartilage has many small fibers; it is found at the ends of bones, in the nose, ribs, and windpipe. Elastic cartilage, because of its elastin component, is able to bend yet maintain its shape, such as in the external ear. Fibrocartilage is a sturdy and resilient form that can withstand tremendous pressure such as in the disks that separate the vertebrae. Connective Tissue Bone tissue is composed of collagen, ground substance, and calcium salts; minerals harden bone so it is capable of supporting and protecting body tissues and organs. Adipose tissue cells are specialized for the storage of fat; most adipose tissue lies just beneath the skin. compact bone tissue blood vessel bone cell (osteocyte) nucleus cell bulging with fat droplet TYPE: Bone tissue TYPE: Adipose tissue DESCRIPTION: Collagen fibers, matrix hardened with calcium DESCRIPTION: Large, tightly packed fat cells occupying most of matrix COMMON LOCATIONS: Bones of skeleton COMMON LOCATIONS: Under skin, around heart, kidneys FUNCTION: Movement, support, protection FUNCTION: Energy reserves, insulation, padding Fig. 4.2ef, p. 71 Connective Tissue Blood is a fluid connective tissue involved in transport; plasma forms the fluid “matrix” and blood proteins, blood cells, and platelets compose the “fiber” portion of the tissue. Figure 4.3 Table 4.2, p. 71 Section 3 Muscle Tissue: Movement Figure 4.4 Muscle Tissue: Movement Muscle tissue contracts in response to stimulation, then passively lengthens; movement is a highly coordinated action. There are three types of muscle: skeletal muscle Skeletal muscle tissue attaches to bones for voluntary movement; long muscle cells are bundled together in parallel arrays, which are enclosed in a sheath of dense connective tissue. Figure 4.4a Muscle Tissue: Movement Smooth muscle tissue contains tapered, bundled cells that function in involuntary movement; it lines the gut, blood vessels, and glands. Cardiac muscle is composed of short cells that can function in units due to the signals that pass through special junctions that fuse the cells together; cardiac muscle is only found in the wall of the heart. cardiac muscle smooth muscle Figure 4.4b-c Section 4 Nervous Tissue: Communication Nervous Tissue: Communication Nervous tissue consists mainly of cells, including neurons (nerve cells) and support cells; nervous tissue forms the body’s communication network. Neurons carry messages. Neurons have two types of cell processes (extensions): branched dendrites pick up chemical messages and pass them to an outgoing axon. Figure 4.5a Nervous Tissue: Communication A cluster of processes from different neurons is called a nerve. Nerves move messages throughout the body. Neuroglia are support cells. Glial cells (neuroglia) make up 90 percent of the nervous system. Neuroglia provide physical support for neurons. Other glial cells provide nutrition (astrocytes), clean-up, and insulation services (Schwann cells). Figure 4.5b Table 4.4, p. 85 Section 5 Cell Junctions: Holding Tissues Together Cell Junctions Epithelial cells tend to adhere to one another by means of specialized attachment sites. Tight junctions link cells of epithelial tissues to form seals that keep molecules from freely crossing the epithelium. Adhering junctions are like spot welds in tissues subject to stretching. Gap junctions link the cytoplasm of adjacent cells; they form communication channels. Cell Junctions Sites of cell-to-cell contact are especially profuse when substances must not leak from one body compartment to another. cell basement membrane intermediate filaments plaques TIGHT JUNCTION ADHERING JUNCTION protein channel GAP JUNCTION Fig. 4.6, p. 74 Section 6 Tissue Membranes: Thin, Sheetlike Covers Tissue Membranes Epithelium membranes pair with connective tissue. Mucous membranes line the tubes and cavities of the digestive, respiratory, and reproductive systems where embedded glands secrete mucus. Serous membranes such as those that line the thoracic cavity occur in paired sheets and do not contain glands. Cutaneous membranes are hardy and dry— and better known as skin. Tissue Membranes Membranes in joints consist only of connective tissue. Synovial membranes line the sheaths of tendons and the capsule-like cavities around certain joints. Their cells secrete fluid that lubricates the ends of the moving bones. mucous membrane serous membrane cutaneous membrane (skin) synovial membrane Fig. 4.7, p. 75 Section 7 Organs and Organ Systems Organs and Organ Systems An organ is a composite of two or more tissue types that act together to perform one or more functions; two or more organs that work in concert form an organ system. The major cavities of the human body are: cranial, spinal, thoracic, abdominal, and pelvic. cranial cavity spinal cavity thoracic cavity abdominal cavity pelvic cavity Fig. 4.8a, p. 76 SUPERIOR (of two body parts, the one closer to head) distal (farthest from trunk or from point of origin of a body part) frontal plane (aqua) midsagittal plane (green) ANTERIOR (at or near front of body) INFERIOR (of two body parts, the one farthest from head) proximal (closest to trunk or to point of origin of a body part) POSTERIOR (at or near back of body) transverse plane (yellow) Fig. 4.8b, p. 76 Organs and Organ Systems Eleven organ systems (integumentary, nervous, muscular, skeletal, circulatory, endocrine, lymphatic, respiratory, digestive, urinary, and reproductive) contribute to the survival of the living cells of the body. Section 8 The Integument – Example of an Organ System The Integument Humans have an outer covering called the integument, which includes the skin and the structures derived from epidermal cells including oil and sweat glands, hair, and nails. The skin performs several functions: The skin covers and protects the body from abrasion, bacterial attack, ultraviolet radiation, and dehydration. The Integument It helps control internal temperature. Its receptors are essential in detecting environmental stimuli. The skin produces vitamin D. Epidermis and dermis—the two layers of skin. outer epidermal layer (all dead cells) keratinized cells being flattened rapidly dividing cells of epidermis dermis Fig. 4.10b, p. 79 The Integument Epidermis refers to the thin, outermost layers of cells consisting of stratified, squamous epithelium. • • • Keratinocytes produce keratin; when the cells are finally pushed to the skin surface, they have died, but the keratin fibers remain to make the outermost layer of skin (the stratum corneum) tough and waterproof. Deep in the epidermis are melanin-producing cells (melanocytes); melanin, along with carotene and hemoglobin, contribute to the natural coloration of skin. Langerhans cells and Granstein cells are two important cells in skin that contribute to immune function. The Integument The dermis is the thicker portion of the skin that underlies the epidermis. • • The dermis is mostly dense connective tissue, consisting of elastin and collagen fibers. Blood vessels, hair follicles, nerve endings, and glands are located here. The hypodermis is a subcutaneous layer that anchors the skin; fat is also stored here. smooth muscle melanocyte sweat pore sebaceous gland Langerhans cell keratinized layer living layer hair shaft EPIDERMIS keratinocyte Granstein cell DERMIS HYPODERMIS adipose cells nerve fiber hair follicle pressure receptor sweat gland Fig. 4.10a, p. 78 The Integument Sweat glands and other structures are derived from epidermis. Sweat glands secrete a fluid (mostly water with a little dissolved salt) that is useful in regulating the temperature of the body. Oil (sebaceous) glands function to soften and lubricate the hair and skin; acne is a condition in which the ducts become infected by bacteria. The Integument Hairs are flexible, keratinized structures rooted in the skin and projecting above the surface; growth is influenced by genes, nutrition, and hormones. Figure 4.11 The Integument Sunlight permanently damages the skin. Ultraviolet (UV) radiation and the light from tanning beds stimulate melanin production in skin, resulting in a tan; too much UV exposure, however, can damage the skin. UV light can activate protooncogenes in skin cells, leading to cancer. Rates of skin cancer are on the rise due to continued destruction of the atmospheric ozone layer that normally protects the Earth from too much UV light. Section 9 Homeostasis: The Body in Balance Homeostasis: The Body in Balance The internal environment: A pool of extracellular fluid. The trillions of cells in our bodies are continuously bathed in an extracellular fluid that supplies nutrients and carries away metabolic wastes. The extracellular fluid consists of interstitial fluid (between the cells and tissues) and plasma (blood fluid). Cell Interstitial (tissue) fluid Blood Blood vessel Extracellular fluid In-text Fig., p. 80 Homeostasis: The Body in Balance The component parts of an animal work together to maintain the stable fluid environment (homeostasis) required for life. Homeostasis requires the interaction of sensors, integrators, and effectors. Homeostatic mechanisms operate to maintain chemical and physical environments within tolerable limits and to keep the body close to specific set points of function. Homeostasis: The Body in Balance Homeostatic control mechanisms require three components: • • • Sensory receptor cells detect specific changes (stimuli) in the environment. Integrators (brain and spinal cord) act to direct impulses to the place where a response can be made. Effectors (muscles and glands) perform the appropriate response. STIMULUS (input into the system) receptor integrator effector (such as a nerve ending in the skin) (such as the brain or spinal cord) (a muscle or gland) RESPONSE to stimulus causes change. The change is “fed back” to receptor. In negative feedback, the system’s response cancels or counters the effect of the original stimulus. Fig. 4.12, p. 80 Homeostasis: The Body in Balance Feedback mechanisms are important homeostatic controls. A common homeostatic mechanism is negative feedback. • • It works by detecting a change in the internal environment that brings about a response that tends to return conditions to the original state. It is similar to the functioning of a thermostat in a heating/cooling system. Positive feedback mechanisms may intensify the original signal; childbirth is an example. dead, flattened skin cells sweat gland pore Fig. 4.13a, p. 81 STIMULUS After overexertion on a hot, dry day, surface temperature of body rises. RESPONSE Body temperature falls,receptors initiate shifts in effector output. receptors In skin and elsewhere; detect the temperature change. effectors integrator Pituitary gland & thyroid gland trigger widespread adjustments in many body organs. The hypothalamus, a brain region, compares input from the receptors against the set point for the body. Effectors These carry out specific responses, including: Skeletal muscles in chest wall work to get additional oxygen into lungs. Smooth muscle in blood vessels dilates; blood transporting metabolic heat shunted to skin; some heat lost to surroundings. Sweat glands secrete more, with cooling effect on the brain especially. Overall slowing of activity results in less metabolically generated heat. Fig. 4.13b, p. 81 Section 10 How Homeostatic Feedback Maintains the Body’s Core Temperature How Homeostatic Feedback Maintains the Body’s Core Temperature Humans are endotherms, heated from within by metabolic processes. Core temperature of the head and torso is roughly 37C (98.6F). Above this temperature (~41C) proteins begin to denature; below this temperature (35C and below) the body stops functioning. Fig. 4.14a, p. 82 Fig. 4.14b, p. 82 How Homeostatic Feedback Maintains the Body’s Core Temperature Responses to cold stress. Cold responses are controlled by an area of the brain called the hypothalamus. Several things happen when the outdoor temperature drops: • • Peripheral vasoconstriction occurs when the hypothalamus commands the muscles around blood vessels to contract; this diverts blood flow away from the body surface. The pilomotor response causes your body hair to stand on end to trap air around the body to prevent heat loss. How Homeostatic Feedback Maintains the Body’s Core Temperature • • Skeletal muscle contractions cause you to shiver in an attempt to generate heat. In babies, who can’t shiver, hormones raise the rate of metabolism in a nonshivering heat production response; this response occurs in a special type of adipose tissue called brown fat. If body temperature cannot be maintained, damage to the body occurs. • • Hypothermia is characterized by mental confusion, coma, and possibly death. Physical freezing can lead to frostbite and death of the affected tissues. How Homeostatic Feedback Maintains the Body’s Core Temperature Responses to heat stress. Heat responses are also controlled by the hypothalamus. • • Peripheral vasodilation causes blood vessels to expand in the skin, allowing excess body heat to dissipate. Heat is also dissipated in sweat from sweat glands; water and salts both are lost to cool the body. How Homeostatic Feedback Maintains the Body’s Core Temperature Various levels of heat stress (hyperthermia) can be experienced: • • Heat exhaustion occurs under mild heat stress; blood pressure drops as fluid is lost and the person can collapse. Heat stroke occurs when the body ceases to be able to control temperature; death is one possible outcome. A fever is a natural rise in core temperature used to fight off disease; severe fevers, however, should be controlled to avoid serious damage to the body. Table 4.3, p. 83