Cells - mustafaaltinisik.org.uk
advertisement

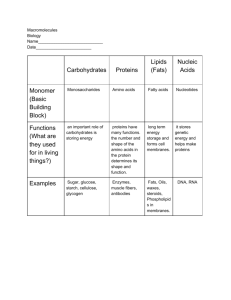
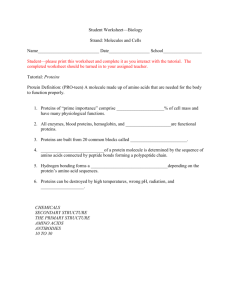
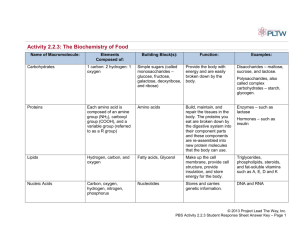
Blood - Biochemical Aspects Functions • Respiratory – Transport O2 from lungs to tissues – Transport CO2 from tissues to lungs • Nutrition – Transport “food” from gut to tissues (cells) • Excretory – Transport waste from tissues to kidney (urea, uric acid, water) • Regulatory – Water Content of Tissues • Water exchanged through vessel walls to tissue (interstitial fluid) • Body Temperature – Water- high heat capacity, thermal conductivity, heat of vaporization – Typical heat generation is 3000 kcal/day • Protective – Antibodies, antitoxins, white blood cells (WBC) • Blood composition – 5-6 L in an adult – 70 mL/kg of body weight – Suspension of cells in a carrier fluid (plasma) • Cells - 45% by volume • Plasma - 55% by volume • Cells – Red cells (erythrocytes) • 5x106/mL – White cells (leukocytes) • 7x103/mL – Platelets (thrombocytes) • 3x105/mL • Plasma composition – Water - 90% of plasma volume – Proteins - 7% of plasma volume – Inorganic - 1% of plasma volume • Na+, K+, Mg2+, Ca2+, PO43-… – Organic - 2% of plasma volume • urea, fats, cholesterol, glucose ... • Male versus female – Hematocrit (% volume that is red cells) • 40-50% in males • 35-45% in females Proteins See Lehninger Chapter 3-6 • Proteins are polyamino acids • Macromolecules - MW 5000 - several million – Insulin - MW = 6000 – Hemoglobin - MW = 68 000 Amino Acid Structure R NH2CH COOH Protein Structure O O ~NHCHC-NHCHC~ R1 R2 Peptide bond • 20 common amino acids (AA) • Classified based on the properties of the R groups Acidic Glutamic Acid Basic Lysine Polar Tyrosine Apolar Glycine Amino Acids and Proteins • Acidic and basic groups are charged at blood / physiologic pH • Proteins are polyelectrolytes • pH of zero net charge (pI or isoelectric point) depends on amino acid composition of protein • Blood proteins negative at pH 7.4 – more COO- than NH3+, pI < 7.4 pI • • • • Protein has many negative charges Requires H+ to neutralize Therefore low pI Consider a protein with pI = 4 – If pH increases above pI protein becomes? – If pH decreases below pI protein becomes? • Higher the pI the more +,- is protein? • Need to go to a higher pH to neutralize or compensate for + charges • Minimum solubility occurs at pI since there is no intermolecular repulsion • At pH 7.4 (blood pH), all blood proteins are negative and therefore have pI’s less than 7.4 Protein Structure • Four levels – Primary structure: sequence of amino acids • 20 amino acids in long chain molecules • many possible combinations – Secondary structure: arrangement of the chains in space (conformation of chains) a-helix: coil shape (due to H bonding) b-sheet: stretched zig-zag peptide chain (H bonding • random coil: similar to synthetic polymers – Tertiary structure: folding of chains into 3 dimensional shape due to H bonding, S-S bonds and hydrophobic interactions • Several different types of secondary structure within the full three dimensional structure of a large protein – Quaternary structure: present in proteins with several polypeptide chains, arrangement and interelationship of the chains due to S-S bridging • Four levels result in well defined shape and chemical structure essential for function of protein Plasma Proteins • More than 200 • Most abundant – Albumin - 4-5 g/100 mL g-glubulins - ~1 g/100 mL – fibrinogen - 0.2-0.4g/100 mL • Original classification by zone electrophoresis at pH 8.6 • Separation by pI with several molecular weight species within each group Zone Electrophoresis of Plasma Proteins + globulins g pI 6.0 b a1 a2 5.6 5.1 albumin 4.7 Protein Separation • Size Exclusion Chromatography (SEC) – Porous matrix (sephadex) • Affinity chromatography – molecule attached to a column that specifically binds the protein of interest • Coenzyme / enzyme • Antigen / Antibody • SDS-PAGE (polyacrylamide gel electrophoresis) – Separates by size – Proteins are complexed with SDS to give the same charge density Two Dimensional Electrophoresis Decreasing Mr Decreasing pI Functions of Plasma Proteins • Maintenance of: – Colloid osmotic pressure (p) – pH – electrolyte balance • COP relates to blood volume DP = p Protein sol’n Water • If membrane present p important • “Isotonic” - same osmotic pressure • Human blood - 300 milliOsmoles /L • Normal saline - 0.9% NaCl by weight – 0.15 mol/L – 0.30 mol/L of particles • Calculate osmotic pressure from concentration? • By analogy with the ideal gas law n p RT V CRT (C in mol/L) c RT (c in g/L) M •In blood, which protein contributes most to p? •Low molecular weight, high concentration • Colloid - large particle that cannot easily cross a membrane – Stays in the compartment – In blood pprotein = 20-30 mmHg – Total ~ 5000 mmHg • Protein stays in the blood as p is maintained in the blood • Water content is therefore maintained • Hypotonic - lower p than normal – Hemolysis of RBC Hb H 2O Ghost Cells Hypertonic - higher p than normal Hemolysis of RBC Hypertonic 1.5% NaCl Crenated Cells H2O Functions of Plasma Proteins (cont’d) • Transport of ions, fatty acids, steroids, hormones etc. – Albumin (fatty acids), ceruloplasmin (Cu2+), transferrin (Fe), lipoproteins (LDL, HDL) • Nutritional source of amino acids for tissues • Hemostasis (coagulation proteins) • Prevention of thrombosis (anticoagulant proteins) • Defense against infection (antibodies, complement proteins) Function and Properties of Selected Plasma Proteins • Consider three abundant plasma proteins • Structure, function • Coagulation, fibrinolysis, complement Albumin • MW 66 000 • Single chain, 580 amino acids, sequence is known • Dimensions - Heart shaped molecule • 50% a helix [He and Carter, Nature, 358 209 (1992)] • Modeled as: 80 Å 30 Å • Synthesis – Mainly liver cells then exported – Assembly time on ribosome ~ 1-2 min – t0.5 in circulation - 19 days – 14 g lost per day – 0.4 mg synthesized per hour per g of liver – Need liver of approximately 1.5 kg in weight to maintain • Functions – “Colloid” osmotic pressure of blood is 80% due to albumin • relatively low molecular weight • regulates water distribution – Transport of fatty acids • Liver to tissues, binding – Source of amino acids for tissue cells (pinocytosis) • 60% albumin in tissue (interstitial) fluid g-Globulins • 20% of plasma proteins • “g” refers to electrophoretic mobility • Represents a group of proteins of variable structure – immunoglobulins • Main functional task is immunochemical – Antibodies - combine with specific antigens • Basic 4 chain structural unit – MW = 2x55000 +2x27000 = 160000 • Variable region varies with respect to primary, secondary and tertiary structures • Basis of specificity of antigen binding (106 average number) • 5 classes of immunoglobulins – IgG, IgA, IgM, IgD, IgE – Different structures of constant regions of heavy chains – Some are polymers (multiples of 4 chain unit - IgA - dimer - MW 350 000, IgM - pentamer - MW 900 000 – See any immunology book for more details • Functions – Primary function is antigen binding (immune response) – Secondary function is complement binding (after antigen) – Each class has different functions • IgE - allergic reactions (defence) • IgA - secretory protein, high concentration in external fluids (saliva, tears) • IgD - ? Involved in differentiation of B lymphocytes (found on the surface of Blymphocytes) • Synthesis – In lymphocytes (T and B) – Made in response to presence of antigen (“foreign” macromolecule, virus particle etc.) Fibrinogen • Coagulation • Structure – MW 340 000 – Sequence of amino acids is known (3000) – 4y, 3y structure • 6 polypeptide chains, 2a (67,000), 2b (56,000), 2g (47,000) a b g disulfide Triple dumbell model (EM) 450 Å 90 Å D E a’s, b’s and g’s are intertwined D • Function – Blood coagulation (clotting) Fibrinogen Fibrin Thrombin Plasmin Fibrin Degradation (FDP) Plasmin is end product of fibrinolytic system Clot needs to be removed Not needed forever Could embolize to lungs, brain Sickle Cell Anemia • Occurs because of a minor variation in one amino acid in the b chain of Hb • Results in Hb that, when exposed to low O2 concentrations precipitates into long crystals • Elongate cell • Damage cell membrane • Decrease in amount of RBC Cellular Elements of Blood • Red cells – 40 - 50% of blood volume – 5 x 106 cells /mL – “bag” of hemoglobin • non-nucleated • no proliferation • cell membrane in excess so that deformation does not rupture – Shape • Biconcave disc • 8 mm in diameter, 2.7 mm thick, volume ~ 90 mm3, area ~ 160 mm2 Scanning Electron Micrograph of Red Blood Cells • Why this shape? – Area to volume ratio is high (maximal?) – Facilitates diffusion of O2 and CO2 • minimal distance of contents from surface • Originates in bone marrow (hematopoiesis) – Molecular explanation based on the properties of the proteins in the cell membrane is found in Elgsaeter et al. Science, 234, 1217 (1986) Oxygen Binding of Hb • Blood must carry 600 L of O2 from lungs to tissues each day – Very little carried in plasma since O2 only sparingly soluble – Nearly all bound and transported by Hb of RBC – Possible for Hb to carry four O2 molecules, one on each a chain, one on each b chain • O2 depleted Hb solution placed in contact with O2(g) • Equilibrium reaction • Fraction (s) of Hb converted to oxyhemoglobin • Described by empirical equation s K ( pO2 ) n 1 K ( pO2 ) n K depends on ionic strength and pH of Hb solution n generally given as 2.5 -2.6 • Binding of O2 to 4 heme sites given by: Hb O2 HbO2 HbO2 O2 Hb (O2 ) 2 Hb (O2 ) 2 O2 Hb (O2 ) 3 Hb (O2 ) 3 O2 Hb (O2 ) 4 Equilibrium constants for different reactions different Binding of first O2 relatively low affinity 2nd, 3rd and 4th - much higher affinity Cooperative effect • Compare with binding curve for myoglobin • Myoglobin - oxygen reaction k1 Mb O2 MbO2 At equilibrium k 1 k1CMbCO2 k 1CMbO2 s CMbO2 CMbO2 CMb k1 CMbCO2 k 1 k1 CMbCO2 CMb k 1 KCO2 1 KCO2 Acid Effect - O2 Dissociation HHb O2 HbO2 H • O2 binding causes release of H+ • pH decreases, [H+] increases then the equilibrium moves to left • % saturation decreases, more dissociation for a given pO2 • Tissues are at a lower pH than the lungs due to CO2 which facilitates release of O2 to tissues Hb versus Mb • Hb carry O2 to tissues where it is released – Releases quickly in tissues where pO2 is lower • Mb store O2 in the muscle, make available to cells – Releases very little in tissues Reference: Science 255 54 (1992) RBC - Reversible Shape Changes • Surfactants result in cells becoming more spherical • Mechanical stress - deformation in capillaries to allow for passage of cells • Disease eg. Sickle Cell Anemia • Hemolysis - release of Hb from the cell – Osmotic swelling – Surface collisions with artificial organs White Blood Cells (Leukocytes) • Total count - approximately 7000/mL • Various types – – – – – – Neutrophils 62% Eosinophils 2.3% Basophils 0.4% Monocytes 5.3% Lymphocytes 30% Plasma cells (mainly in the lymph) • Monocytes in tissue become macrophages • Function – Defense against foreign invaders • bacteria • viruses • foreign materials (including biomaterials) • Phagocytosis – Neutrophils, macrophages – Move to foreign particle by chemtaxis • Chemicals induce migration • Toxins, products of inflamed tissues, complement reaction products, blot clotting products – Response is extremely rapid (approx 1 h) • Lymphocytes – B cells - responsible for humoral immunity – T cells - responsible for cell mediated immunity • B cells responsible for production of antibodies – Receptor matches antigen – Cells multiply – Antibodies • Abs are just immunoglobulins discussed earlier • T cells – Cytotoxic T cells (Killer T cells) • Bind to cytotoxic cells (eg infected by virus) • Swell • Release toxins into cytoplasm – Helper T cells • • • • Most numerous Activate B cells, killer T cells Stimulate activity by secretion of IL2 Stimulate macrophages – Suppressor T cells • Regulate activities of other cell types AIDS • HIV - attacks many cell types – – – – epithelial cells macrophages neurons lymphocytes (helper T) • Infected helper T cells when stimulated, produces viral proteins which kill the cell • Helper T cell population disappears Platelets • • • • • • Non-nucleated disk shaped cells 3-4 mm diameter Volume 10 x 10-9 mm3 250 000 cells/mL 10 day circulation time Surface contains membrane bound receptors (GP Ib and IIb/IIIa) – mediate surface adhesion reactions, aggregation reactions – interact with coagulation proteins • Contain muscle proteins actin and myosin which contract when platelet is activated • Also a granules, dense granules, lysosomal granules • Platelets activated by minimal stimulation – Become sticky – Shape change – Release of cell contents • Stimulate other platelets • Function – Initially arrest bleeding through formation of platelet plugs – Stabilize platelet plugs by catalyzing coagulation reactions leading to formation of fibrin • Platelet Adhesion – Site of injury - exposure of connective tissue elements (eg collagen) – Artificial surfaces through forming thrombi (clots) • Platelet Aggregation – Caused by ADP, collagen, thrombin, epinephrine, PAF, TXA2 • Release of cell contents – Induced by ADP, collagen, thrombin, TXA2 and epinephrine Coagulation • Maintenance of hemostasis (prevention of blood loss) • At least 12 plasma proteins interact in series of reactions • Cascade of reactions • Inactive factors become enzymatically active following surface contact, proteolytic cleavage by other enzymes • Amplification is rapid • Reactions are localized • Extrinsic system – Blood comes in contact with traumatized vascular wall or extravascular tissues • Intrinsic system – Initiated by surface contact (often negatively charged surface) • Most reactions are Ca++ dependent • Chelaters of Ca++ effective anticoagulants Fibrinolysis • Results in dissolution of fibrin clot