Microorganism Identification Process *Lecture 1*
advertisement
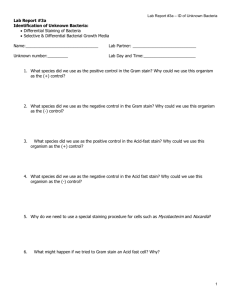
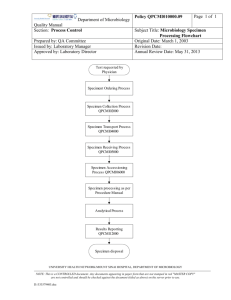
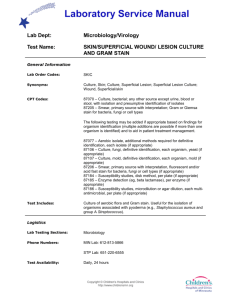
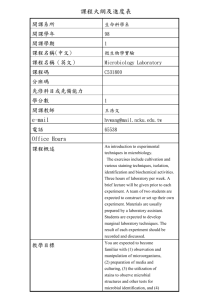
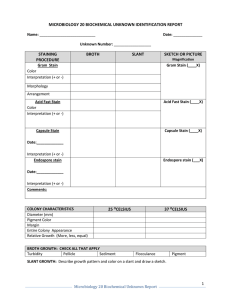
Microorganism Identification Process *Lecture 1* Diagnostic Microbiology Laboratory -2015- Introduction to Bacterial Identification Accurate and definitive microorganism identification, including bacterial identification and pathogen detection, is essential for correct disease diagnosis, treatment of infection and trace-back of disease outbreaks associated with microbial infections. Bacterial identification is used in a wide variety of applications including microbial forensics, criminal investigations, bioterrorism threats and environmental studies. Approach to Laboratory Diagnosis o o The laboratory diagnosis of infectious diseases involves two main approaches: Bacteriological approach; in which the organism is identified by: microscopic observation, macroscopic identification, biochemical reactions and molecular diagnosis techniques. Immunological (serological) approach; in which the organism is identified by detection of antibodies against the organism in the patient’s serum. Cultural Characteristics Microorganisms may show distinguishing gross morphologies when cultured on different media. This macroscopic appearance of bacteria (characteristic growth patterns which can be observed with the naked eye) is often used in their identification. Cultural Characteristics are observed according to 1. Observe the amount of growth o none = 0 o slight = + o moderate = ++ o abundant = +++ 2. Coloration- Two types of pigmentation may occur: a. pigmentation occurring within the organism itself; or b. water soluble pigment that diffuses into the surrounding medium. Most organisms will lack chromogenesis (pigment production), exhibiting a white, beige, or gray growth. Pigmentation within the organism may be red, yellow, violet, or other colors. Soluble pigments may be blue, green, yellow, brown, or other colors. Hold the plate up to the light to examine for diffusible pigments. It may be helpful to compare the color of the agar with an uninoculated media. 3. Opacity- Surface growth can be termed as opaque, as transparent, or as translucent partial transparency) depending on the degree of growth. 4. Form- The gross or macroscopic appearance of the growth from the single streak inoculation is described by: a. filiform - uniform growth along the line of inoculation. b. echinulate- margins of growth have a toothed appearance. c. beaded- separate or semi confluent colonies. d. effuse- growth is thin, veil-like, unusually spreading. e. arborescent- branched, tree-like growth. f. rhizoid- root-like appearance Morphology and staining There are many different ways to stain bacteria so that they can be more easily visualized under the microscope. Some stains can also be used to identify and classify bacteria. o 1. Gram stain o 2. Acid fast Stain Other stains used to visualize bacterial structure o Spore stain o Flagellar stain o Capsule stain Biochemical Characteristics 1. Fermetation & oxidation. 2. IMVIC tests. 3. Biochemical tests. 4. API 20 E. Other techniques 1. PCR 2. Phage typing 3. Other molecular techniques Serological characteristics To Identify several strains of the same type of bacteria we need to perform serotyping of them such as: 1. Widal test 2. Lancefield grouping 3. Protien A latex 4. others How to handle microbiological sample Some samples will demonstrate microbial growth and require further laboratory analysis to identify the contaminants. When growth is detected, the sample should be taken from the clean section of the laboratory to the live culture section without undue delay. Subculturing, staining, microbial identification, or other investigational operations should be undertaken in the live culture section of the laboratory. If possible, any sample found to contain growing colonies should not be opened in the clean zone of the laboratory. Careful segregation of contaminated samples and materials will reduce false-positive result. . How to handle microbiological sample Soo it necessary to ensure: 1. Proper collection of the sample 2. Adequate amount 3. Requisitions 4. Tightly capped container How to handle microbiological sample When needed, a written test request must include the following information: 1. Hospital No. 2. Full name 3. Gender 4. Date of birth 5. Address 6. Social security no. 7. For female pregnant/ lactating 8. Date of illness 9. Signs/ symptoms 10. Date of onset 11. Recent travel history 12. Immunization Identification of samples 1. Type of specimen 2. Collection date and time 3. Laboratory number 4. Laboratory findings 5. Test requested 6. Ordering physician Specimen handling and storage Samples should be delivered to microbiology central processing area, within the specified period and then CPA will 1. Check requisition for completeness. 2. Store the sample until they are picked up to microbiology staff. When STAT requests are received, the CPA staff should inform the microbiology supervisor. Specimen rejection criteria 1. The information in the label doesn’t match the information on the request form. 2. The specimen was transported in improper container or at wrong temperature. 3. Leaking specimen. 4. The quantity of specimen is insufficient. Comments 1. Blood received in blood culture is unsuitable for fungal isolation. 2. Saliva is unacceptable for culture. 3. Multiple samples sent with the same request should be noticed. Samples not satisfactory for culturing 1. Sample in fixative 2. Dried out swab 3. 24hrs urine or sputum 4. Urine still more than 2hrs at room temperature. 5. Antibiotic medicated patient 6. Anaerobic culture for vaginal, cervical, or urine samples 7. Stool samples from more than 5 days inpatient. Media Classification Consistency Nutritional component Functional use Solid Simple Basic-General- media Semisolid Complex Selective Liquid –Broth- Synthetic or Chemically Defined Media: Exact chemical composition is known Differential Enriched Enrichment Transport End of Lecture