cardiac_cycle
advertisement

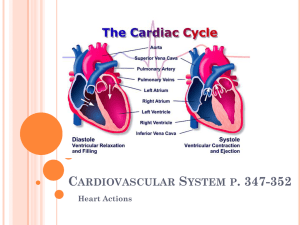
Learning Objectives After reading this chapter you should be able to: 1. Describe the organization of the cardiovascular system. 2. Describe the sequence of events that occur during one cardiac cycle. Explain how pressures and volumes within the heart chambers change. 3. Describe the pressure – volume loop. 4. List the approximate values for mean pressures found at various stages of the cardiac cycle. 5. Explain how an increase in heart rate would affect various stages of the cardiac cycle. 6. Describe and explain the atrial and central venous pressure waves. 7. Explain the ECG in terms of the cardiac cycle. 8. Describe and explain when sounds are heard during the cardiac cycle. 9. Explain why S2 is split. 10. List and explain the common types of heart murmurs. Cardiac cycle describes the sequence of electrical and mechanical events that occur in the heart during one single beat • The cycle is divided into two major phases, both named for events in the ventricles: the period of ventricular contraction and blood ejection, systole, followed by the period of ventricular relaxation and blood filling, diastole. • At an average heart rate of 72 beats/min, each cardiac cycle lasts approximately 0.8 s, with 0.3 s in systole and 0.5 s in diastole Like a pump with a reciprocating piston, the heart alternates between a filling phase and an emptying phase. To understand the Mechanical event you must recall: Anatomy of the Heart • The atrioventricular (AV) valves prevent blood flow from the ventricles back into the atria • The pulmonary and aortic valves prevent backflow from the pulmonary trunk into the right ventricle and from the aorta into the left ventricle respectively Cardiac valves operation. They open when pressure gradient across the valves is increasing in the direction that blood normally flows (forward pressure gradient) (A). A reverse pressure gradient (B) will force the valve closed, which prevents reverse blood flow in response to reverse pressure gradient that occur as a result of the pumping action. (C). A forward pressure gradient forces the semilunar valve to open. Darker colors correspond to higher pressure Isovolumetric ventricular relaxation /phase 4 ventricular filling/phase 1 Diastole = Iso-volumetric ventricular contraction/phase 2 Systole = Ventricular ejection/phase 3 Mechanical events of the cardiac cycle 1 START 5 4 Isovolumic ventricular relaxation: as ventricles relax, pressure in ventricles falls, blood flows back into cups of semilunar valves and snaps them closed. Ventricular ejection: as ventricular pressure rises and exceeds pressure in the arteries, the semilunar valves open and blood is ejected. Late diastole: both sets of chambers are relaxed and ventricles fill passively. Atrial systole: atrial contraction forces a small amount of additional blood into ventricles. 2 3 Isovolumic ventricular contraction: first phase of ventricular contraction pushes AV valves closed but does not create enough pressure to open semilunar valves. Mechanical Events 1 START Late diastole: both sets of chambers are relaxed and ventricles fill passively. 1 START Late diastole: both sets of chambers are relaxed and ventricles fill passively. 2 Atrial systole: atrial contraction forces a small amount of additional blood into ventricles. 1 START Late diastole: both sets of chambers are relaxed and ventricles fill passively. Atrial systole: atrial contraction forces a small amount of additional blood into ventricles. 2 Isovolumic ventricular contraction: first phase of ventricular contraction pushes AV valves closed but does not create enough pressure to open semilunar valves. 3 1 START Late diastole: both sets of chambers are relaxed and ventricles fill passively. Atrial systole: atrial contraction forces a small amount of additional blood into ventricles. 2 Ventricular ejection: as ventricular pressure rises and exceeds pressure in the arteries, the semilunar valves open and blood is ejected. 3 4 Isovolumic ventricular contraction: first phase of ventricular contraction pushes AV valves closed but does not create enough pressure to open semilunar valves. Isovolumic ventricular relaxation: as ventricles relax, pressure in ventricles falls, blood flows back into cups of semilunar valves and snaps them closed. 5 Ventricular ejection: 4 as ventricular pressure rises and exceeds pressure in the arteries, the semilunar valves open and blood is ejected. START 1 Late diastole: both sets of chambers are relaxed and ventricles fill passively. 2 Atrial systole: atrial contraction forces a small amount of additional blood into ventricles. 3 Isovolumic ventricular contraction: first phase of ventricular contraction pushes AV valves closed but does not create enough pressure to open semilunar valves. http://library.med.utah.edu/kw/pharm/hyper_ heart1.html The period lasting from the closure of the atrioventricular (AV) valve to the opening of the aortic valve is generally known as A B C D E Ventricular filling phase Isovolumetric ventricular contraction Ventricular ejection phase Isovolumetric ventricular relaxation Protodiastole period The heart at rest: atrial and ventricular diastole. The atria are filling with blood from the veins, and the ventricles are relaxing – the AV valves between the atria and ventricles open. Blood is flowing by gravity into the ventricles. The relaxing ventricles expand to accommodate the entering blood. At this moment the ventricles are ~ 80 – 90% filled with blood. This is the section to the left of atrial systole on the diagram. 1. Atrial systole and completion of ventricular filling. The generation of an action potential by the SA node results in a wave of depolarization spreading through the atria P wave on the ECG. Atrial muscle contracts (atrial systole) and atrial pressure rises (a wave). A little more blood (10 – 20%), sometimes called the‘atrial kick’ is pushed into the almost full ventricles. However, a small amount of blood is forced backwards into the great veins (there are no one way valves between the veins and the atria) causing a similar a wave in the central veins (vena cava). This wave can be seen as a pulse in the jugular vein of a person who is semirecumbent with the head and chest elevated ~ 30 degrees . If a pulse is seen higher up the jugular vein in a person who is upright it indicates that the right atrial pressure is higher than normal. End Diastolic Volume, end-systolic volume and stroke volume • The amount of blood in the ventricles just before systole is the end-diastolic volume. The volume remaining after ejection is the end-systolic volume, and the volume ejected is the stroke volume •S4- caused by vibration of the ventricular wall during atrial contraction. Generally, it is noted when the ventricle compliance is reduced ("stiff" ventricle) as occurs in ventricular hypertrophy and in many older individuals. 2. Ventricular systole A. Isovolumetric Contraction The wave of depolarization reaches ventricles and we have the QRS complex on the ECG, which denotes ventricular depolarization. Shortly thereafter the ventricles contract and squeeze the blood upward and towards the base. As soon as the pressure in the ventricles rises above the atrial pressure, the AV valves close causing the first heart sound. Since the aortic and pulmonary valves are already closed each ventricle is now a closed chamber. They continue to contract and because they are closed, the pressure within them rises very steeply (more in the LV than the RV). This is called the isovolumetric contraction phase -c wave in the RA pressure tracing. • When Ventricular pressures exceed aortic and pulmonary trunk pressure, the aortic and pulmonary valves open, and V ejection of blood occurs • When the ventricles relax at the beginning of the diastole, the V pressures fall significantly below those in the aorta and pulmonary trunk, and the aortic and pulmonary valves close. Because the AV valves are also still closed, no change in V volume occurs during this isovolumetric ventricular relaxation The vibrations due to closure of the semilunar valves give rise to the second heart sound. • When ventricular pressures fall below the pressures in the right and the left atria, the AV valves open, and the ventricular filling phase of diastole begins • Filling occurs very rapidly at first so that atrial contraction, which occurs at the very end of diastole, usually adds only a small amount of additional blood to the ventricles Fig. 12. Cardiac cycle again Angiography Heart Sounds. The common heart sound are: • The first heart sound is due to the closing of the AV valves • The second heart sound is due to the closing of the aortic and pulmonary valves Heart Sounds Sound Characteristics Associated events S1 First heart sound (sounds like “lub”) Two bursts, a mitral M1 and a tricuspid T1 components Closure of mitral & tricuspid valves S2 Second heart sound (sounds like “dub”) An aortic A2 and a pulmonary P2 component Closure of aortic and pulmonary valves OS Opening Snap Opening of a stenotic mitral valve S3 Third heard sound Diastolic filling gallop or V or protodiastolic gallop S4 Fourth heart sound Atrial sound that creates an atrial or presystolic gallop Note that a physiological S3 sound is present in some normal individuals, particularly children. Occurs in early diastole with rapid filling of the ventricles; When present S4 coincides with atrial contraction but usually it is abnormal Location of the sounds on the chest Each valve is best heard by a stethoscope from 4 distinct areas: Mitral valve: Mid clavicular line of the 5th left intercostal space Tricuspid valve: 5th interspace at the left sternal edge Aortic valve: 2nd interspace at the right sternal edge Pulmonary valve: 2nd interspace at the left sternal edge Heart Murmurs: Abnormal heart sounds heard on auscultation which are due to faulty valves. • Incompetence: Failure of the valve to seal properly (valve may be torn, perforated, affected by rheumatic fever or a failing heart may be enlarged) such that it becomes leaky allowing blood to regurgitate through it • Stenosis: The open valve is narrowed so that a higher pressure gradient is needed to drive blood through (cicatrization after rheumatic or other infection) • Defective valves can be congenital or acquired. Abnormal valve causes blood turbulence which sets up high frequency vibrations which are heard as murmurs through the stetoscope Rheumatic heart disease Heart Murmurs (cont.) • Benign Systolic Murmur • Aortic stenosis: Systolic murmur. Due to narrowing of the aortic valve when the flow during ejection becomes turbulent. Heard during ejection (systolic murmur) as ejection waxes and wanes (a crescendo – decrescendo murmur). Loudest over aortic area Aortic stenosis murmur Mitral Stenosis • left atrial pressure is elevated with mitral stenosis induce hypertrophy of the left atrial muscle. • Elevated left atrial pressure is reflected back into the pulmonary bed and, if high enough, causes pulmonary congestion and "shortness of breath.“ • A diastolic murmur associated with turbulent flow through the stenotic mitral valve can often be heard. If a murmur heard during C and increased A. Thewas aortic valve opens at D2 which and closes at 7then decreased in volume, which of the following valve defects is Thetoaortic valve opens at 3 and closes at 5 mostB. likely be present? C. The mitral valve opens at 2 and closes at 5 A) Aortic incompetence B) Aortic stenosis D. The mitral valve closes at 3 and opens at 5 C) Mitral stenosis E. The mitral valve closes at 3 and opens at 7. D) Mitral incompetence The Atrial and Central Venous Pressure (CVP) waves • Since there are no valves between the jugular veins (JV), v. cavae ant the RA, the right JV are communicated with the RA. • Changes in pressure in the RA produces a series of pressure changes which are reflected in the central veins and recorded from the JV: a, c and v waves. • CVP is the pressure in the vein at the entrance of the RA • a wave is due to increase in pressure caused by atrial systole • av descent (minimum) is due to relaxation of the right atrium and closure of the tricuspid valve • c wave is caused in the RA by the tricuspid valve bulging back into the atrial chamber as it closes. In the internal JV the c wave (c = carotid) is caused partly by expansions of the carotid artery • X descent is a sharp fall in the pressure caused by atrial relaxation • v wave. As the atria fill, A pressure rises producing v wave (v = ventricular systole which is occurring at the same time) • Y descent is a fall in pressure due to the rapid emptying of the atria after the AV valve opens Fig. 13. Jugular venous pressure changes caused by cardiac cycle Clinical examination of the JVP • JP of the internal jugular vein can be assessed by expecting the right side of the neck of a recumbent subject(45 degrees). Two sudden venous collapses (the X and Y descent) should be seen and measured externally on the right side of the neck- positive JVP • In right-side cardiac failure there is a positive JVP due to accumulation of blood into the failing RV and RA Summary of the Cardiac Cycle Assessed at the bedside by noting: • Peripheral pulse at radial artery (heart rate and force) • Systolic and diastolic blood pressure (will be discussed later) • Jugular venous pulse observation • Apex beat (displacement on the left identifies left V hypertrophy) • Heart sounds When pathology is suspected more specialized tests are carried out: • Echocardiography (non-invasive): Observing movement of the valves and walls of the heart (valve lesions, myocardial infarction, cardiac hypertrophy of different origin) • Cardiac catheterization (invasive) Hello Dr. Vishal, My step 1 went well. I ended up with a score of 237. Thanks to you and all the other teachers at Windsor for laying a solid foundation in all the subjects, it made my preparation much easier and a pleasant experience. Many of the concepts we learned in school were tested on the exam so I felt confident having that good foundation. I still remember all the tips you used to give us in class about tackling the exam, they helped a great deal. Thank you again for all that you have done for us, I really appreciate it. Regards,