Heart
advertisement

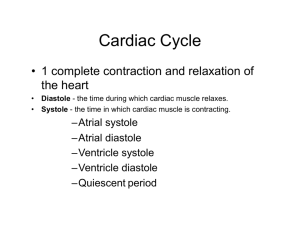
Heart The adult heart has the shape of a blunt cone and is approximately the size of a closed fist. The blunt, rounded point of the cone is the apex; the larger, flat part at the opposite end of the cone is the base.The heart is located in the thoracic cavity between the lungs. The heart, trachea, esophagus, and associated structures form a midline partition called the mediastinum The heart is enclosed in a double-walled sac called the pericardium. The parietal pericardium, the outer layer of the pericardium, consists of a tough layer of fibrous connective tissue and a thin moist serous layer. The inner layer of the pericardium is called visceral pericardium or the epicardium. It covers the surface of the heart. Between the parietal and viscerial pericardia is a space called the pericardial cavity. The heart wall consists of three layers: the epicardium, the myocardium, and the endocardium. The epicardium, previously mentioned, is the outermost layer of the heart wall. It consists of serous membrane. The myocardium, the thickest layer, is cardiac muscle tissue and the endocardium consists of simple squamous endothelium overlying a thin areolar tissue layer Heart Blood Flow The pathway of a red blood cell from the right atrium and back. (1) right atrium -> (2) -> right AV valve -> (3) right ventricle -> (4) pulmonary valve -> (5) pulmonary trunk -> (6) pulmonary arteries -> (7) lungs, for exchange of gases (not shown) -> (8) pulmonary veins -> (9) left atrium -> (10) left AV valve -> (11) left ventricle -> (12) aortic valve -> (13) aorta -> (14) other systemic vessels -> (15) inferior and superior venae cavae -> (16) back to the right atrium. The pathway from 5 to 8 is the pulmonary circuit, and thepathway from 13 to 15 is the systemic circuit. Blood Flow through the Heart The heart operates as two parallel pumps. The right side of the heart circulates blood through the lungs; the left circulates blood through the other parts of the body. Histology Heart muscle demonstrating the structure and arrangement of the individual muscle fibers Conduction System Gap Junctions Gap junctions (electrical synapses) exist between the cardiac muscle cells. They are ion channels between cells that allow cells to stimulate each other. This promotes a unified action. Conduction System The conduction system transmits electrical impulses via specialized cardiac fibers, ensuring that the heart muscle contracts in a coordinated fashion. Sinoatrial Node Atrioventricular Node Atrioventricular Bundle Right and left bundle branches Purkinje fibers The timing of the heart’s beating is coordinated by special conducting fibers. The two atria contract as a unit slightly before the two ventricles do so. The SA node is the pacemaker, which initiates each heartbeat. Electrocardiogram The normal ECG consists of a P wave, a QRS complex, and a T wave. The P wave, which is the result of action potentials that cause depolarization of the atrial myocardium, signals the onset of atrial contraction. The QRS complex is composed of three individual waves: the Q, R, and S waves. The QRS complex results from ventricular depolarization and signals the onset of ventricular contraction. The T wave represents the repolarization of the ventricles and thus precedes ventricular relaxation. A wave representing repolarization of the atria cannot be seen because it occurs during the QRS complex. Electrocardiogram The time between the beginning of the P wave and the beginning of the QRS complex is the PQ interval, commonly called the PR interval because the Q wave is often very small. During the PR interval, which lasts approximately 0.16 second, the atria contract and begin to relax. The ventricles begin to depolarize at the end of the PR interval. The QT interval extends from the beginning of the QRS complex to the end of the T wave, lasts approximately 0.3 second, and represents the approximate length of time required for the ventricles to contract and begin to relax. Electrocardiogram Electrical currents generated in the heart can be detected by electrodes placed on the surface of the body. An electrocardiogram is a graphic display of the heart's electrical activity. Cardiac Cycle The heart's contractile activity results in pressure changes that propel blood through the circulatory system. These pressure changes occur in a cyclic nature and are referred to as the cardiac cycle. Systole and Diastole The term systole means "to contract," and diastole means "to dilate." Atrial systole is contraction of the atrial myocardium, and atrial diastole is relaxation of the atrial myocardium. Similarly, ventricular systole is contraction of the ventricular myocardium, and ventricular diastole is relaxation of the ventricular myocardium. When the words "systole" and "diastole" are used without reference to specific chambers, however, they mean ventricular systole or diastole. The atria (a) empty during atrial systole and (b) fill with blood during atrial diastole. Quiescent period: Atria and ventricles in diastole. AV valves open,blood flows into atrium to ventricles. 70% of blood passively enters ventricles during this period. Atrial pressure is greater than ventricular pressure. Atrial systole: SA node fires, the atria depolarize and stimulates atrial systole, pumping the remaining 30% of blood into ventricles. The volume of blood in ventricles following end-diastolic volume (EDV) is about 130ml. Isovolumetric contraction: Atria repolarize and relax. Ventricles depolarize and begin to contract. Ventricle pressure rises above atrial pressure and AV valves close. Semilunar valves are also closed. Ventricles contract; but there is no change in volume because all valves are closed. Ventricular ejection: As ventricles contract, ventricular pressure builds, finally exceeding arterial pressure. The semilunar valves open and blood is ejected. The volume ejected per contraction (approximately 70ml) is called the stroke volume. The lbood remaining in the ventricle (about 60ml) is called the end-systolic volume. Isovolumetric relaxation: Ventricles relax; blood from the aorta and pulmonary trunk briefly flows backwards but then fills the cusps of the semilunar valves, promting them to close. This creates a small pressure rebound to the dicrotic notch of the aortic pressure curve. Ventricular filling: Ventricular diastole occurs. Ventricular pressure drops below atrial pressure. AV valvesopen and blood flows rapidly into ventricles (rapid ventricular filling.) Pressure gradient decreases;blood flows into ventricles slower (diastasis.) Remaining blood enters ventricle following atrial systole. Ventricular filling includes phases 1 and 2. Heart Sounds The closing of valves in the heart produces sounds that are often described as "lub dub". The "lub" is produced by the closing of the AV valves. The "dub" is produced by the closing of semilunar valves. Heart Murmurs - Normal Aortic Valve A normal aortic valve only allows blood to flow from the left ventricle into the aorta when the ventricular pressure exceeds that in the aorta. Closing of the aortic valve produces the "dub" heart sound. Heart Murmurs - Valvular Insufficiency Valvular insufficiency is a condition in which the cusps of the valve do not form a tight seal when the valve is closed. Aortic valvular insufficiency results in an abnormal sound during ventricular diastole. Heart Murmurs - Valvular Stenosis Valvular stenosis is a condition that results from abnormal constriction of the valve's ability to open fully. Aortic stenosis can be heard during ventricular systole. Cardiac Output Heart rate and stroke volume and thus cardiac output can be altered by a baroreceptor reflex. Baroreceptors located in the aortic arch and the carotid arteries detect changes in blood pressure. If blood pressure decreases, the baroreceptors inform the cardioregulatory center in the medulla oblongata. The medulla oblongata increases sympathetic stimulation to the SA node thus increasing heart rate to the myocardium, which increases calcium availability and thus increases stroke volume.