How to write progress notes and communicate in
advertisement
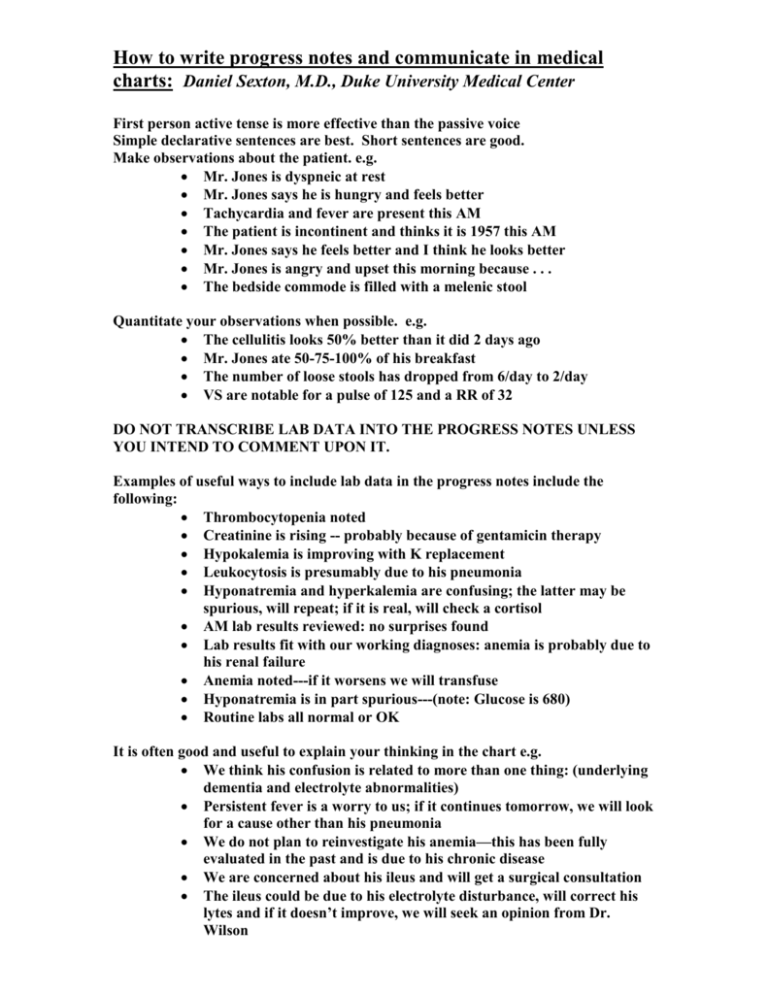
How to write progress notes and communicate in medical charts: Daniel Sexton, M.D., Duke University Medical Center First person active tense is more effective than the passive voice Simple declarative sentences are best. Short sentences are good. Make observations about the patient. e.g. Mr. Jones is dyspneic at rest Mr. Jones says he is hungry and feels better Tachycardia and fever are present this AM The patient is incontinent and thinks it is 1957 this AM Mr. Jones says he feels better and I think he looks better Mr. Jones is angry and upset this morning because . . . The bedside commode is filled with a melenic stool Quantitate your observations when possible. e.g. The cellulitis looks 50% better than it did 2 days ago Mr. Jones ate 50-75-100% of his breakfast The number of loose stools has dropped from 6/day to 2/day VS are notable for a pulse of 125 and a RR of 32 DO NOT TRANSCRIBE LAB DATA INTO THE PROGRESS NOTES UNLESS YOU INTEND TO COMMENT UPON IT. Examples of useful ways to include lab data in the progress notes include the following: Thrombocytopenia noted Creatinine is rising -- probably because of gentamicin therapy Hypokalemia is improving with K replacement Leukocytosis is presumably due to his pneumonia Hyponatremia and hyperkalemia are confusing; the latter may be spurious, will repeat; if it is real, will check a cortisol AM lab results reviewed: no surprises found Lab results fit with our working diagnoses: anemia is probably due to his renal failure Anemia noted---if it worsens we will transfuse Hyponatremia is in part spurious---(note: Glucose is 680) Routine labs all normal or OK It is often good and useful to explain your thinking in the chart e.g. We think his confusion is related to more than one thing: (underlying dementia and electrolyte abnormalities) Persistent fever is a worry to us; if it continues tomorrow, we will look for a cause other than his pneumonia We do not plan to reinvestigate his anemia—this has been fully evaluated in the past and is due to his chronic disease We are concerned about his ileus and will get a surgical consultation The ileus could be due to his electrolyte disturbance, will correct his lytes and if it doesn’t improve, we will seek an opinion from Dr. Wilson It is useful to communicate with consultants using the progress notes. e.g. Question for Dr. Wilson: When do you plan to pull his NG tube? We would like the ID consult team to comment upon their recommendation to change to imipenem: Is it better than the current Rx of flagyl and cipro? If not, why change therapy? When the ID team makes rounds please page me at 970-4556: we need to discuss the duration of antibiotic Rx We would like to arrange a management conference with GI and surgery tomorrow—GI and surgery -- please indicate when you can meet with us. We have asked GI to see the patient and comment upon these questions: o Is endoscopy indicated? o Do they agree that jaundice is out of proportion to his LFT abnormalities? When dealing with a difficult patient or family, write down what was said e.g. Conference was held with the patient’s family this AM; we told them the following: o The pneumothorax that followed attempted placement of a central line will require a chest tube for 3-7 days o That we are aware of their complaints about his nursing care We told the patient that his kidney problems are not getting better. Often direct quotes are useful e.g. o The patient told me: “I don’t want any more tests” o The family told me: “Jack drinks more than he admits” o The patient said: “I can’t eat the food they give me” o The patient’s son told me: “I can’t take care of my mother and she refuses to go to a nursing home.” o The patient told me: I would rather die at home than go to a nursing home.” Do not mindlessly repeat yourself in daily notes It is often useful to list the hospital day, the post-op day and the duration of various treatments. e.g. o This hospital day 24 and day 8 of gentamicin and day 4 of vancomycin) o This is ICU day 6 and day 13 of Vancomycin—21 days of rx are planned WRITE LEGIBLY LENGTH OF NOTES DOES NOT RELATE TO RELEVENCE OF NOTES You should be able to reconstruct the events and the management by reading the daily notes SOMETIMES IT IS BEST TO STATE THE OBVIOUS e.g. o Our working diagnoses remain bacterial pneumonia and renal failure due to obstructive uropathy o We have been unable to find a cause for his lung infiltrates but we believe that they are not due to pulmonary edema o We have not been able to make a conclusive diagnosis that explains his lung infiltrates o Despite our best efforts he is still in CHF o After 5 days in the hospital we have concluded the following: o His CHF is better o His renal function is worse o His confusion and agitation are multi-factorial o He will not be able to live independently in near future It is often useful to summarize findings as a series e.g. o The following have not improved since admission: o Resting tachycardia o Temperature curve o Edema o The following have improved since admission 4 days ago: o Mental status o Renal function o Hyperglycemia o Appetite It is not necessary to put the vital signs in each progress notes; although this can be useful if they are abnormal (in which case, comments about their significance are often helpful and/or appropriate) e.g. o VS normal o Resting pulse 125—believe the reason is hypoxia and CHF o Pulse 120—still in atrial fib Remember to read the nurses notes. This may keep you out of court. ALWAYS TIME ALL NOTES (MAKE THIS A LIFE-LONG HABIT) If you don’t know what is wrong it is sometimes useful to state what isn’t wrong: eg. We are fairly sure that the fever is not due to pneumonia, a UTI, or meningitis.