File
advertisement

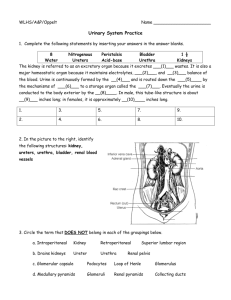
The Urinary System The Urinary System Paired kidneys A ureter for each kidney Urinary bladder Urethra 2 Main Functions of Urinary System Kidneys filter blood to keep it pure Toxins Metabolic wastes Excess water Excess ions Dispose of nitrogenous wastes from blood Urea Uric acid Creatinine Regulate the balance of water and electrolytes, acids and bases 3 Kidneys : (renal = pertaining to the kidney) Lateral surface is convex Medial surface is concave Hilus* is cleft: vessels, ureters and nerves enter and leave Adrenal glands lie superior to each kidney (the yellow blob in pic) * * 4 5 6 7 Kidney has two regions Cortex: outer Columns of cortex divide medulla into “pyramids” Medulla: inner Darker, cone-shaped medullary or renal pyramids Parallel bundles of urine-collecting tubules 8 The human kidney has lobes Pyramid and cortical tissue surrounding it 5-11 per kidney Renal pelvis (=basin) Expanded, funnel shaped, superior part of ureter Branches to form two or three major calices (seen best on right pic below) Each of these divides again, minor calices: collect urine from papillae of pyramids 9 The Arteries Aorta gives off right and left renal arteries Renal arteries divides into 5 segmental arteries as enters hilus of kidney Segmentals branch into lobar arteries Lobars divide into interlobars Interlobars into arcuate in junction of medulla and cortex Arcuates send interlobular arteries into cortex Cortical radiate arteries give rise to glomerular arterioles 10 Vasculature of the kidney The glomerular capillary bed is unusual in having arterioles going both to it and away from it (afferent and efferent), instead of a vein going away as most It is also unusual in having two capillary beds in series (one following the other) 11 Uriniferous tubule is the main structural and functional unit To left is a single, generalized uriniferous tubule More than a million of these tubules act together to form the urine Three main mechanisms a. Glomerular filtration b. Tubular reabsorption c. Tubular secretion Two major parts 1. A urine-forming nephron 2. A collecting duct which concentrates urine by removing water from it 12 Outline Uriniferous tubule (anatomical unit for forming urine) Nephron Renal corpuscle (in cortex) – Glomerulus (tuft of capillaries) – Glomerular (Bowman’s) capsule Tubular section – Proximal convoluted tubule – Loop of Henle – Distal convoluted tubule Collecting duct 13 Outline Uriniferous tubule (anatomical unit for forming urine) Nephron Renal corpuscle (in cortex) – Glomerulus (tuft of capillaries) – Glomerular (Bowman’s) capsule Tubular section – Proximal convoluted tubule – Loop of Henle – Distal convoluted tubule Collecting duct 14 Understand at least this much: Filtration a. Fluid is squeezed out of the glomerular capillary bed Resorption b. Most nutrients, water ad essential ions are returned to the blood of the peritubular capillaries Secretion c. Moves additional undesirable molecules into tubule from blood of peritubular capillaries 15 Nephron Renal corpuscle Tubular section Uriniferous tubule (anatomical unit for forming urine) Nephron Renal corpuscle (in cortex) Glomerulus (tuft of capillaries) Glomerular (Bowman’s) capsule Tubular section Proximal convoluted tubule Loop of Henle Distal convoluted tubule Collecting duct Renal corpuscle: only in cortex Tuft of capillaries called glomerulus Surrounded by cup-shaped, hollow glomerular (Bowman’s) capsule 16 Uriniferous tubule (anatomical unit for forming urine) Nephron Nephron Renal corpuscle Tubular section Renal corpuscle (in cortex) Glomerulus (tuft of capillaries) Glomerular (Bowman’s) capsule Tubular section Proximal convoluted tubule Loop of Henle Distal convoluted tubule Collecting duct (processes the filtrate) Proximal convoluted tubule Loop of Henle Distal convoluted tubule (ends by joining collecting duct) 17 Uriniferous tubule (anatomical unit for forming urine) Proximal convoluted tubule Confined to renal cortex Cuboidal epithelial cells with long microvilli (fuzzy appearance in pics) Resorption of water, ions and solutes Nephron Renal corpuscle (in cortex) Glomerulus (tuft of capillaries Glomerular (Bowman’s) capsu Tubular section Proximal convoluted tubule Loop of Henle Distal convoluted tubule Collecting duct * 18 Uriniferous tubule (anatomical unit for forming urine) Nephron Loop of Henle Descending limb Renal corpuscle (in cortex) Glomerulus (tuft of capillaries) Glomerular (Bowman’s) capsule Tubular section Proximal convoluted tubule Loop of Henle Distal convoluted tubule Collecting duct Thin segment Thick ascending limb 19 Uriniferous tubule (anatomical unit for forming urine) Nephron Distal convoluted tubule Confined to the renal cortex Simple cuboidal epithelium Selective secretion and resorption of ions Renal corpuscle (in cortex) Glomerulus (tuft of capillaries Glomerular (Bowman’s) caps Tubular section Proximal convoluted tubule Loop of Henle Distal convoluted tubule Collecting duct 20 Classes of nephrons Cortical nephrons 85% of all nephrons Almost entirely within cortex Juxtamedullary nephrons Renal corpuscles near cortexmedulla junction 21 Uriniferous tubule (anatomical unit for forming urine) Nephron Renal corpuscle (in cortex) Glomerulus (tuft of capillaries) Glomerular (Bowman’s) capsule Tubular section Proximal convoluted tubule Loop of Henle Distal convoluted tubule Collecting duct Collecting Ducts Collecting Duct Each receives urine from several nephrons Run straight through cortex into the deep medulla 22 Uriniferous tubules 1. Nephron 2. Collecting ducts Collecting Ducts * At papilla of pyramid* ducts join to form larger papillary ducts Empty into minor calices Role: conserve 23 body fluids The collecting ducts The most important role is to conserve body fluids When the body must conserve water, the posterior pituitary gland secretes ADH (antidiuretic hormone) ADH increases the permeability of the collecting tubules and distal tubules to water so more is reabsorbed This decreases the total volume of urine Alcohol inhibits the release of ADH, so less water is reabsorbed producing copious amounts of dilute urine (can cause dehydration) 24 Vessels Afferent and efferent arterioles associated with glomerular capillaries Allows high pressure for forcing filtrate out of blood About 20% of renal plasma flow is filtered each minute (125 ml/min): this is the glomerular filtration rate (GFR), an important clinical measure of renal function This is about one liter every 8 minutes (only 1% ends up as urine) Peritubular capillaries arise from efferent arterioles Absorb solutes and water from tubule cells 25 (vessels, continued) The Vasa recta The Vasa recta is a portion of the peritubular capillary system which enters the medulla where the solute concentration in the interstitium is high. It acts with the loop of Henle to concentrate the urine by a complex mechanism of counter current exchange using urea. If the vasa recta did not exist, the high concentration of solutes in the medullary interstitium would be washed out. ____vasa recta 26 Histology 27 28 29 For studying Parts of the kidney: 1. Renal pyramid 2. Efferent vessel 3. Renal artery 4. Renal vein 5. Renal hilum 6. Renal pelvis 7. Ureter 8. Minor calyx 9. Renal capsule 10. Inferior renal capsule 11. Superior renal capsule 12. Afferent vessel 13. Nephron 14. Minor calyx 15. Major calyx 16. Renal papilla 17. Renal column 30 The Ureters Slender tubes about 25 cm (10 “) long leaving each renal pelvis One for each kidney carrying urine to the bladder Descend retroperitonealy and cross pelvic brim Enter posterolateral corners of bladder Run medially within posterior bladder wall before opening into interior This oblique entry helps prevent backflow of urine 31 Three basic layers Transitional epithelium of mucosa stretches when ureters fill Muscularis Ureters play an active role in transporting urine (it’s not just by gravity) Inner longitudinal, outer circular layers Inferior 3rd with extra longitudinal layer) Stimulated to contract when urine in ureter: peristaltic waves to propel urine to bladder Adventitia (external) 32 Urinary Bladder See also brief atlas Collapsible muscular sac Stores and expels urine Lies on pelvic floor posterior to pubic symphysis Males: anterior to rectum Females: just anterior to the vagina and uterus 33 34 35 36 If full: bladder is spherical and extends into abdominal cavity (holds about 500 ml or 1 pt) If empty: bladder lies entirely within pelvis with shape like upside-down pyramid Urine exits via the urethra Trigone is inside area between ureters and urethra: prone to infection (see slide 38) 37 Bladder wall has three layers (same as ureters) Mucosa with distensible transitional epithelium and lamnia propria (can stretch) Thick muscularis called the detrusor muscle 3 layers of highly intermingled smooth muscle Squeezes urine out Fibrous adventitia 38 The Urethra Smooth muscle with inner mucosa Changes from transitional through stages to stratified squamous near end Drains urine out of the bladder and body Male: about 20 cm (8”) long Female: 3-4 cm (1.5”) long Short length is why females have more urinary tract infections than males ascending bacteria from stool contamination urethra Urethra____ 39 Urethral sphincters Internal: involuntary sphincter of smooth muscle External: skeletal muscle inhibits urination voluntarily until proper time (levator anni muscle also helps voluntary constriction) Males: urethra has three regions (see right) _________trigone 1. Prostatic urethra__________ 2. Membranous urethra____ 3. Spongy or penile urethra_____ female 40 With all the labels 41 Micturition AKA: Voiding Urinating Emptying the bladder (See book for diagram explanation p 701) KNOW: Micturition center of brain: pons (but heavily influenced by higher centers) Parasympathetic: to void Sympathetic: inhibits micturition 42