The Integumentary system
advertisement
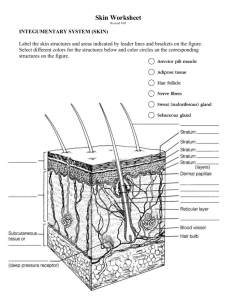
The Integumentary system two major components 1. cutaneous membrane A. epidermis /superficial epithelium B. dermis/underlying connective tissues. C. hypodermis/ Deep to the dermis 2. accessory structures hair, nails, exocrine glands, blood vessels, sensory receptors for touch, pressure, temperature, and pain functions of the skin Protection - organs against shocks, abrasion, and chemical attack.(stratified squamous epithelium) Excretion - salts, water, and organic wastes by glands. Maintenance of temperature - insulation or evaporation Synthesis of vitamin D3 - steroid converted to hormone calcitriol, important to normal calcium metabolism and membrane repair. Storage - nutrients.lipids Detection - touch, pressure, pain, and temperature The Epidermis There are four cell types found in the epidermis Keratinocytes Produces a tough protein called keratin Melanocytes Pigment cells located deep in the epidermis Produce melanin (skin color) Merkel cells Sensory cells Langerhans cells Fixed macrophages The Epidermis Thick and thin skin Thick skin Found on palms and soles Made of five layers of cells Has stratum lucidum Thin skin Found on the rest of the body Made of four layers of cells LAYERS OF THE EPIDERMIS In order, from the basal lamina toward the free surface, are the stratum germinativum(basale), stratum spinosum, stratum granulosum, stratum lucidum, stratum corneum. Stratum granulosum Stratum spinosum stratum germinativum/basale Dermal projections called dermal papillae extend between adjacent epidermal ridges The contours of the skin surface follow the ridge patterns - Fingerprints Large basal cells, or germinative stem cells, dominate the stratum germinativum. Skin surfaces that lack hair also contain Merkel cells that are sensitive to touch; when compressed, they release chemicals that stimulate sensory nerve endings. The brown tones of skin result from the pigment cells called melanacytes, with cell processes extending into more superficial layers. Stratum granulosum Stratum spinosum Stratum Spinosum Each time a stem cell divides, one of the daughter cells is pushed from the stratum germinativum into the stratum spinosum, The stratum spinosum consists of 8 to 10 layers of cells Langerhans cells (fixed macrophages) present, stimulate a defense against (1) microorganisms that manage to penetrate the superficial layers of the epidermis and (2) superficial skin cancers. Stratum granulosum Stratum spinosum Stratum Granulosum consists of three to five layers of keratinocytes displaced from the stratum spinosum. By the time cells reach this layer, most have stopped dividing & they begin making large amounts of keratin and keratohyalin Keratin is a tough fibrous protein component of hair and nails. Keratohyalin forms dense granules that dehydrate the cell and aggregate cross-linking of the keratin fibers. The nuclei and other organelles disintegrate, and the cells die. dehydration creates a tightly interlocked layer of cells of keratin fibers surrounded by keratohyalin. Stratum granulosum Stratum spinosum Stratum Lucidum In the thick skin of the palms and soles, a glassy stratum lucidum covers the stratum granulosum The cells in the stratum lucidum are flattened, densely packed, and filled with keratin. thick skin, on the palms and soles have five layers … lucidum is the 5th layer Stratum granulosum Stratum spinosum Stratum Corneum At the exposed surface of both thick skin and thin skin contains 15 to 30 layers of keratinized cells. remain tightly interconnected by desmosomes. shed in large groups or sheets rather than individually. 15 to 30 days for a cell to move from the stratum germinativum to the stratum corneum. The dead cells remain in the exposed stratum corneum layer for an additional two weeks before they are shed insensible perspiration Water from interstitial fluids slowly evaporates into the surrounding air. You lose roughly 500 ml (about 1 pt) of water in this way each day. Skin Color Three pigments contribute (1) melanin - amount and kind (yellow, reddish brown, or black) (2) carotene - orange-yellow found in carrots & orange, deep yellow, or leafy green vegetables. (3) oxygen – amount bound to hemoglobin people who produce a lot of melanin have brown-toned skin. the crimson color of oxygen-rich hemoglobin gives the skin a rosy color When hemoglobin is poorly oxygenated, the skin appear blue, a condition called cyanosis Cyanosis is common during heart failure and severe breathing disorders. skin color signals disease states: • Rubor, Redness, or erythema - embarrassment (blushing), fever, hypertension, inflammation, or allergy. • Pallor, or blanching - emotional stress (fear, anger, and others), Pale skin may also signify anemia, low blood pressure, or impaired blood flow into the area. • Jaundice, or a yellow- cast – liver disorder excess bile pigments in the blood Bruises - sites where blood has escaped and has clotted in the tissue spaces.(hematomas) unusual bruising may signify a deficiency of vitamin C or hemophilia melanin produced by melanocytes sunlight stimulates the melanocytes to produce more melanin (tanning) Freckles and moles are where melanin is concentrated in one spot. excessive sun eventually damages the skin. basale cells phagocytize the melanin & form a protective "umbrella" over nuclei (DNA) from ultraviolet radiation in sunlight. It causes the elastic fibers to clump, leading to leathery skin. It also depresses the immune system. Overexposure to the sun can also alter the DNA of skin cells and in this way lead to skin cancer. Dermis The dermis is your "hide." It is leather The dense fibrous connective tissue has two major regions— papillary and reticular The papillary layer is the upper region. It is uneven and has fingerlike projections called dermal papillae that create fingerprints They contain capillaries, pain receptors (free nerve endings) and touch receptors called Meissner's corpuscles The reticular layer is the deepest skin layer. It contains blood vessels, sweat and oil glands, and deep pressure receptors called Pacinian corpuscles & phagocytes That attack bacteria As we age we produce less collagen and elastin and fat decreases (wrinkles) hypodermis Foundation that attaches to bone and muscle Supplies skin with blood vessels and nerves Consists of loose connective tissue Called subcutaneous tissue or superficial fascia ½ of the body’s fat is in hypodermis Insulates, energy, padding Used to calculate total body fat The Dermis Wrinkles Under normal circumstances, the fibers of the reticular layer of the skin stretch and recoil. Skin wrinkles are due to: Age UV light The Dermis Stretch Marks Extensive stretching during pregnancy causes reticular fibers to break The skin does not recoil The skin wrinkles and creases resulting in stretch marks The Dermis Lines of Cleavage Fibers have a tendency to organize themselves in a parallel fashion In certain areas of the body, there is a pattern To reduce scar formation (extensive damage to the fibers), surgeons try to cut parallel to the lines of cleavage Accessory Glands in the skin Structures 1. Sebaceous glands 2. Sweat glands Apocrine glands Ceruminous glands (a type of apocrine gland) Mammary glands (a type of apocrine gland) Merocrine glands Both formed by stratum basale & push into dermis. Gland function: Lubricates the epidermis, excretes waste, assists in thermoregulation Cutaneous Exocrine Glands (all are exocrine glands) Glands - release secretions to surface via ducts 1. Sebaceous (Oil) Glands – - all over except on the palms of hands and feet. Their ducts usually empty into a hair follicle but some open directly onto the skin surface.(lips, eyelids, genitalia) sebum (seb = grease), mixture of oily substances and fragmented cells lubricate skin & kill bacteria, male sex hormones produced in both sexes during adolescence increase sebum 2. Sweat Glands (sudoriferous= sweat)— more than 2.5 million per person. There are two types merocrine/eccrine and apocrine. Merocrine/eccrine glands - more numerous all over the body. produce sweat, primarily water plus salts, vitamin C, traces of metabolic wastes (ammonia, urea, uric acid), and lactic acid (attracts mosquitoes). Sweat is acidic (pH from 4 to 6), and inhibits growth of bacteria, which are always present on the skin surface. Apocrine glands - confined to axillary and genital areas their ducts empty onto hair follicles. Their secretion contains fatty acids, proteins, salt & water may have a milky or yellowish color. odorless, but when bacteria that live on skin use its proteins and fats it has an unpleasant odor. Apocrine glands begin to function during puberty under the influence of androgens. Their precise function is not yet known, but they are activated by nerve fibers during pain and stress and during foreplay. Accessory Structures Sweat glands Mammary glands A special type of apocrine gland Produce milk under the control of hormones from the pituitary gland Ceruminous glands A special type of apocrine gland Found only in the ear canal Produce cerumen (ear wax) Provide minimal protection associated with the ear Disorders Sebaceous (Oil) Glands Acne Active infection of sebaceous glands Can be mild or extremely severe Whitehead A sebaceous gland‘s duct becomes blocked by sebum Blackhead Accumulated material oxidized, dries, and darkens Hairs and Hair Follicles Guards the head, shields the eyes (eyelashes) keep foreign particles out of the respiratory tract (nose hairs) A hair is produced by a hair follicle As the daughter cells are pushed away from the growing region they become keratinized and die. root - part of the hair enclosed in the follicle Shaft - projecting from the surface of scalp/skin hair bulb matrix - the growth zone at the inferior end of the follicle medulla - a central core surrounded by a bulky cortex layer cuticle - single layer of cells overlap most heavily keratinized region dermal sheath - dermal connective tissue provides blood to hair bulb. arrector pili - smooth muscle connecting hair follicle to dermal tissue (goose bumps) Accessory Structures Types Vellus Covers most of the body Intermediate of Hair Covers arms and legs Terminal Covers the head Accessory Structures Functions Protection from UV light Insulation Guards entrance to nose and ears Movement of the hair sends impulses via nerves to the brain of Hair Such as when a bug is crawling on your arm Contraction of the arrector pili muscles Results in goose bumps Accessory Structures Hair color Due to: Variation in melanin production by the melanocytes Melanin production decreases with age Influenced by: Genetics Hormones Environmental factors Hair growth Active phase Regression phase Resting phase Reactivation phase Accessory Structures • Nails • Function • Provide protection for the tips of the fingers and toes • Structure • • • • • Free edge Lateral nail fold Lunula Eponychium Hyponychium Hyponychium nails A scalelike modification of the epidermis free edge body (visible attached portion) root (embedded in the skin) Nailfolds - overlapped skin folds cuticle - thick proximal nail fold nail bed - stratum basale beneath the nail nail matrix - thickened proximal area is responsible for nail growth produced by the matrix nails become keratinized and die (nonliving) Nails look pink because of the rich blood supply in the underlying dermis Lunula - white crescent over nail matrix Aging and the Integumentary System Epidermis becomes thinner Dermis becomes thinner Number of Langerhans’ cells decreases Vitamin D production declines Melanocyte activity declines Glandular activity declines Hair follicles stop functioning Skin repair slows down eyelopmental Aspects of Skin l/and Body Membranes During the fifth and sixth months of fetal development, the soon-to-be-born infant is covered with a downy type of hair called lanugo (lah-noo'go), but this hairy cloak has usually been shed by birth. When a baby is born, its skin is covered with vernix caseosa (ver'niks kah-se-o'sah). This white, cheesy-looking substance, produced by the sebaceous glands, protects the baby's skin while it is floating in its water-filled sac inside the mother. The newborn's skin is very thin, and blood vessels can easily be seen through it. Commonly, there are accumulations in the sebaceous glands, which appear as small white spots called milia (mil'e-ah), on the baby's nose and forehead. These normally disappear by the third week after birth. As the baby grows, its skin becomes thicker and moist, and more subcutaneous tat is deposited. During adolescence, the skin and hair become ,,more oily as sebaceous glands are activated, and acne may appear. Acne usually subsides in early adulthood, and the skin reaches its optimal appearance when we are in our 20s and 30s. Then visible changes in the skin begin to appear as it is continually assaulted by abrasion, chemicals, wind, sun, and other irritants and as its pores become clogged with air pollutants and bacteria. As a result, pimples, scales, and various kinds of dermatitis (der"mah-ti'tis), or skin inflammation, become more common. During old age, the amount of subcutaneous tissue decreases, leading to the intolerance to cold so common in the elderly. The skin also becomes drier (because of decreased oil production and declining numbers of collagen fibers) and, as a result, it may become itchy and bothersome. Thinning of the skin, another result of the aging process, makes it more susceptible to bruising and other types of injuries. The decreasing elasticity of the skin, along with the loss of subcutaneous fat, allows bags to form under our eyes, and our jowls begin to sag. This loss of elasticity is speeded up by sunlight, so one of the best things you can do for your skin is to shield it from the sun by wearing sunscreens and protective clothing. In doing so, you will also be decreasing the chance of skin cancer. Although there is no way to avoid the aging of the skin, good nutrition, plenty of fluids, and cleanliness help delay the process. Hair loses its luster as we age, and by age 50 the number of hair follicles has dropped by one-third and continues to decline, resulting in hair thinning and some degree of baldness, or alopecia (al"o-pe'she-ah), in most people. Many men become obviously bald as they age, a phenomenon called male pattern baldness. A bald man is not really hairless— he does have hairs in the bald area. But because those hair follicles have begun to degenerate, the hairs are colorless and very tiny (and may not even emerge from the follicle). Such hairs are called vellus (veil = wool) hairs. Another phenomenon of aging is graying hair. Like balding, this is usually genetically controlled by a "delayed-action" gene. Once the gene takes effect, the amount of melanin deposited in the hair decreases or becomes entirely absent, which results in gray-to-white hair. S Certain events can cause hair to gray or fall out prematurely. For example, many people have claimed that they turned gray nearly overnight because of some emotional crisis in their life. In addition, we know that anxiety, protein-deficient diets, therapy with certain chemicals (chemotherapy), radiation, excessive vitamin A, and certain fungal diseases (ringworm) can cause both graying and hair loss. However, when the cause of these conditions is not genetic, hair loss is usually not permanent. •