ANATOMY & PHYSIOLOGY OF THE INTEGUMENTARY SYSTEM
advertisement

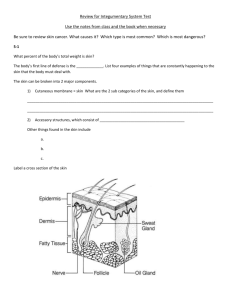
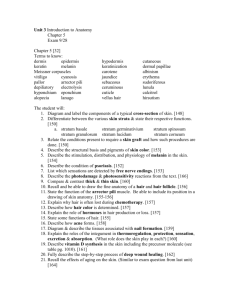
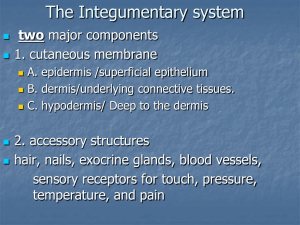
ANATOMY & PHYSIOLOGY OF THE INTEGUMENTARY SYSTEM ANATOMY & PHYSIOLOGY 13-14 Artificial Heart Artificial Ear Artificial Nose Artificial Eye WHY HAS ARTIFICIAL SKIN BEEN SO DIFFICULT TO CREATE? Electronic Nanoskin? Forms and Functions Of The Integumentary System FORMS FUNCTIONS • Skin • Hair • Scales • Nails • Hooves • Feathers • Protection • Waterproofing • Excretion of Wastes • Thermoregulation • Vitamin Synthesis • Attachment For Sensory Structures Histology of Integumentary System • Epithelium • Squamous • Cuboidal • Columnar • Visceral Muscle (i.e. arrector pili) • Follicular (i.e. hair) • Glandular Tissue (apocrine, eccrine, sebaceous) • Nervous Tissue SKIN BY THE NUMBERS • Largest organ in body • 1-2 m2 surface area • 12-15% of body mass • 30,000 skin cells lost/min • Skin cycles every 28 days • Varying Thickness & Elasticity • 0.02-0.6mm (eyelids) • 1.4-3 mm (sole of foot) STRATIFICATION OF SKIN Epidermis • Outermost layer of skin • Derived from ectoderm during cellular differentiation • Comprised of squamous epithelium (~95% keratinocytes) • Avascular • Protects the organism (pH 5/dry) • Regulates water loss via Transepidermal Water Loss (TEWL) Epidermal Histology • Stratum Corneum = 10-30 layers of corneocytes (thickest in palms and soles). Barrier function • Stratum Lucidum = 4-5 cells thick (only in palms and soles) • Stratum Granulosum = anucleate, fatty layer • Stratum Spinosum = Interconnected keratinocytes with immunological functions • Stratum Basale = Contains melanocytes and Merkel Cells (light touch) Melanocytes • Melanin producing cells of Stratum Basale • 1000-2000 cells/mm2 • Skin color attributed to activity of melanocytes, NOT their density • Human skin color takes up to 6 months to fully develop • Two types of melanin • Pheomelanin = yellow->red • Eumelanin = brown->black • Melanin protects against UV radiation. • UV damage to DNA stimulates melanogenesis Albinism/Achromasia • 1:110,000 humans lacks the enzyme tyrosinase • Recessive condition • Tyrosinase required for melanogenesis • Two forms • Oculocutaneous = eye and skin • Ocular = eye only Fingernails •Epidermal extension •Nail Plate (non-living) •Nail Bed (living) •Lunula Dermis • Layer between epidermis and subcutaneous • Made of connective tissues (collagen & elastic fibers) and cells (fibroblasts, macrophages & adipocytes) • Vascular • Two Dermal Regions • Stratum Papillare (bordering epidermis) • Blood vessels • Meissner’s Corpuscles • Stratum Reticulare (deep) • Follicular Roots • Sebaceous Glands • Apocrine & Eccrine Glands Folliculus pili • Comprised of epithelial cells, visceral muscle and adjacent sebaceous glands • Activity of Folliculus pili • Anagen = 1cm growth/28 days for 2-7 years • Catagen = 2-3 weeks where hair is cut off from blood supply and forms a “club” end • Telogen = 3 months. Hair at rest. Stress may cause 70% of hair to enter telogen • Exogen – loss of hairs (20-100 day) Arrector pili • Visceral muscle connected to club/base of hair shaft • Autonomic control via sympathetic nervous system • Causes erection of hair shaft (piloerection) • In many species, piloerection allows for retention of heat • Function in humans is vestigial Sebaceous Glands • Apocrine Gland = expressed when cells rupture • Most common in scalp and face, part of pilosebaceous unit along with hair shaft and arrector pili • Sebum = Fatty mixture of waxes, triglyceride oils and fatty ester • Keep hair shaft flexible, antibacterial and slows evaporation • Vernix caseosa = white sebaceous layer on newborns. • Food source for Demodex mites Sudoriferous Glands • Two types • Eccrine = distributed all over body • Apocrine = concentrated in armpits, anus • Produce sweat; a mixture of water, salt, urea and vitamin C • Essential homeostatic structures utilized for thermoregulation and antibacterial properties • Only areas that do not sweat are fingernails, eardrums, lip margins and glans • Other modified sweat glands include • Ceruminous = ear wax • Ciliary = eyelids • Mammary = milk Dermal Papillae and Friction Ridges • “fingerprints” • Genetically determined but do not develop until 3rd gestational month • Derived from the dermal papillae, replaced when eroded • Basis of dactyloscopy • Naegeli Syndrome = no fingerprints! Hypodermis/Subcutaneous Layer • Lowest of all skin layers • Derived from mesoderm (not ectoderm) • Contents • Adipose • Vascular and Lymphatic Tissue • Ruffini and Pacinian Corpuscles (sensory)