Case 2 - VITALS Home
advertisement

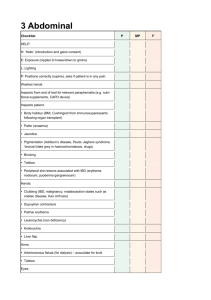
The Acute Abdomen LSI Part 2 Understanding Patients with Reproductive and Surgical Needs David C. Evans, MD Assistant Professor of Surgery david.evans@osumc.edu Acute Abdomen Learning Objectives Primary Objectives Secondary Objectives • Evaluate and determine initial treatment of patients presenting with surgical diseases in all patients as well as medical diseases in pregnant patients. • Evaluate and formulate a management plan for a patient with acute abdominal pain. • Recognize medical or surgical emergencies in the pregnant and nonpregnant female patients. • Evaluate and formulate a management plan for a patient with perforation of the GI tract. • Develop a differential diagnosis for abdominal pain. • Describe the initial evaluation, diagnostic studies management of a patient with an acute abdomen • Decide if a patient with an acute abdomen needs an operation, and justify your decision. • Describe the signs, symptoms and clinical findings associated with acute abdomen. • Recognize patients with extraabdominal causes of abdominal pain. Acute Abdomen Learning Resources Click to link directly to Sabiston: Chapter 47, “Acute Abdomen” (on-campus / proxy server only) Foundational Science – Physiology “How sick is this patient?” Systemic Inflammatory Response Syndrome (SIRS) Criteria Temp >38°C (100.4°F) or < 36°C (96.8°F) Heart Rate > 90 Respiratory Rate > 20 or PaCO2 < 32 mm Hg WBC > 12,000/mm>3, < 4,000/mm>3, or > 10% bands Acute Abdomen Alert Signs + Findings Peritonitis Sepsis / SIRS “Free Air” Likely Need Surgery Peritonitis-Irritation of the Peritoneal Lining Typical signs (most patients have some, not all) Pain with movement or stretching of the peritoneum. Often keep knees and hips flexed Hypersensitive to touch, mild bumps (car rides / hospital cart) Rigid abdomen “Rebound tenderness” Can be focal or diffuse Usually Requires Surgery Don’t always trust a benign exam Steroids Chemo Obesity Limited Mental Capacity Pneumoperitoneum Pneumoperitoneum Algorithm Acute Abdominal Pain with Peritonitis Stable / No SIRS SIRS / Sepsis Operate “Safe Strategies” N.B. Exceptions do exist Pneumoperitoneum On X-ray No Pneumoperitoneum On X-ray Operate Contrast Study (Typically CT) Free Air or Contrast Extravasation -> Operate Contained Collection / Perforation -> Operate vs. Drain Normal Study -> Monitor Closely Algorithm Normal Evaluate for “NonSurgical Causes” Acute Abdominal Pain Without Peritoneal Signs Generalized Pain Focal Pain CT with PO and IV contrast Selective Imaging (History / Exam Dependent) Arterial Ischemia Operate Venous Thrombosis Anticoagulate Positive Negative Operate / Drain Continue to Evaluate- Urgent Surgery Not Required Foundational Science – Anatomy “Where does it hurt?” – Referred Pain Common Causes of the Acute Abdomen Bowel Perforation or Ischemia Infection (Appendicitis / Cholecystitis, etc) Hemoperitoneum (trauma, ruptured ectopic, etc) Hernias (Incarcerated / Strangulated) Always Check for Hernias Sudden Severe Abdominal Pain Kidney Stone (Hematuria, flank pain) Ruptured AAA (Shock, Back Pain, H/O vascular dz) Perforated Ulcer Patients know exactly when these symptoms started! Non-abdominal causes of pain Endocrine and Metabolic Causes • • • • Uremia Diabetic crisis Addisonian crisis Acute intermittent porphyria • Hereditary Mediterranean fever Hematologic Causes • Sickle cell crisis • Acute leukemia • Other blood dyscrasias Toxins and Drugs • Lead poisoning • Other heavy metal poisoning • Narcotic withdrawal • Black widow spider poisoning Case 2 58 yo male 2 day history of left lower quadrant abdominal pain. Pain started L>R, Attempted to take some pepto-bismol but that did not help. He report some associated nausea, he denies any vomiting Some subjective fevers at home. The pain was unrelenting therefore he came to the ED for further evaluation. He reports his abdomen feels more distended and the pain is worse with movement. He has been unable to tolerate much PO. Case 2- order of events Physical Exam / Vitals Labs Imaging Confirmation Treatment Plan Case 2 Findings Abdomen: Tender, distended. Peritonitis 14.8 12.8 44.3 Does he need a CT scan? (87% granulocytes) 243 Case 2 – CT Probably not needed but here it is Free air Inflammation Diverticuli -> perforated diveriticulitis Case 2 Treatment Surgery! Summary Physical Exam, Patient Status (sepsis, etc.) drives algorithm Differential Diagnosis based on exam, confirmed with imaging Take every opportunity to examine patients with pathology now as a student Timing can be crucial to good outcomes Thank you for completing this module Questions? Contact me at: david.evans@osumc.edu 640 Faculty Office Tower (395 W 12th Ave.) Image Credits Slide 1 photo- http://www.enfermeriablog.com/tag/cuidados-peritonitis/ Slide 3- cover images from amazon.com Slide 4- “Know the signs, know sepsis”- Boston Medical Center; http://www.coloribus.com/adsarchive/prints/land-rover-defender-fireball-1965105/ Slide 5-6 photos- OSUMC images Slide 7 photo- http://onemomsbattle.com/TheLiesofaNarcissist Slide 8 image- http://prep-pg.blogspot.com/2012/04/radiological-signs-of-bowel-perforation.html Slide 9 image- OSUMC Slide 12 image from Sabiston, Ch. 47. Slide 14 image from http://www.celebritydiagnosis.com/2013/04/dwayne-the-rock-johnsonundergoes-hernia-surgery/ Slide 15 image- http://www.hongkiat.com/blog/extraordinary-clocks/ Slide 16 table- adapted from Sabiston, Ch. 47. Slide 18 images- http://www.fairview.org/healthlibrary/Article/89315 and cancer.osu.edu Slide 19 image- http://www.pinterest.com/carolinagirl525/x-ray/ Slide 20 image- Van Wagoner ZD, Evans DC, Askegard-Giesmann JR, Kenney BD. Perforated peptic ulcer in a child with a vagus nerve stimulator for seizure control. Brain Stimul. 2013 Nov;6(6):972-3. Slide 24- OSU clinical image Slide 25 image- http://5minuteconsult.com/ViewImage/2027820 Survey We would appreciate your feedback on this module. Click on the button below to complete a brief survey. Your responses and comments will be shared with the module’s author, the LSI EdTech team, and LSI curriculum leaders. We will use your feedback to improve future versions of the module. The survey is both optional and anonymous and should take less than 5 minutes to complete. Survey