Acute Abdomen

Acute abdominal pain is a common 911 call. Often times, prehospital care providers do not do complete abdominal exams, and therefore, proper treatment in the prehospital care setting is not achieved. Hopefully these article will help you to fine tune your abdominal pain evaluation skills.
Courtesy of patient.co.uk
The term 'acute abdomen' represents a rapid onset of severe symptoms that may indicate life-threatening intra-abdominal pathology.
Pain is usually a feature but is not always the case. A pain-free acute abdomen is more likely in the elderly, in children and in the third trimester of pregnancy.
[ 1 ]
The differential diagnosis is extremely wide and definitive diagnosis is often difficult, particularly in primary care. This is due to the many different organs within the peritoneal
cavity and the potential for referred pain.
Abdominal pain is a common problem, ranking in the top three symptoms of patients presenting to accident and emergency departments, but only a few of those patients will have an acute abdomen.
[ 2 ]
Management of the acute abdomen in primary care should focus on careful assessment to reach a differential diagnosis list, with close attention paid to symptoms and signs that may indicate a need to investigate the situation further in hospital.
The clinical scenario can change rapidly and conclusions previously reached by you or your colleagues may need to be revised as events evolve. A failure to be open-minded and revise a previous diagnosis is often at the heart of medicolegal claims relating to patients with an acute abdomen.
[ 1 ]
This article will concentrate on diagnosing the important causes of the acute abdomen in primary care/emergency department settings.
Major causes
This list is far from exhaustive but is a useful aide-mémoire for those conditions commonly seen in the community:
[ 1 ]
Acute cholecystitis .
Acute appendicitis or Meckel's diverticulitis .
Acute pancreatitis .
Ectopic pregnancy .
Diverticulitis .
Peptic ulcer disease .
Pelvic inflammatory disease .
Intestinal obstruction , including paralytic ileus (adynamic obstruction).
Gastroenteritis .
Acute intestinal ischaemia /infarction or vasculitis.
Gastrointestinal (GI) haemorrhage.
Renal colic or renal tract pain.
Acute urinary retention .
Abdominal aortic aneurysm (AAA).
Testicular torsion .
Nonsurgical disease, eg myocardial infarction , pericarditis, pneumonia , sickle cell crisis , hepatitis , inflammatory bowel disease , opiate withdrawal, typhoid, acute intermittent porphyria , HIV-associated lymphadenopathy or enteritis.
Rare causes include placenta percreta,
[ 3 ]
phytobezoar
[ 4 ]
and thromboemboli.
[ 5 ]
Classification of causes according to site of pain
Another way to consider the causes of an acute abdomen is by classifying them according to the area of the abdomen most affected by pain (again, the list is not exhaustive):
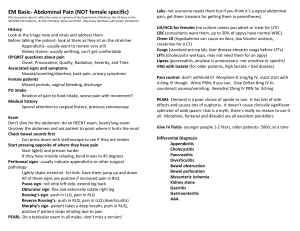
Assessment
Initial impression/observation
Does the patient look ill, septic or shocked?
Are they lying still (think peritonitis ), or rolling around in agony (think intestinal, biliary
or renal colic)?
Assess and manage Airway, Breathing and Circulation as a priority.
In an emergency department setting: if there are signs that the patient is shocked or acutely unwell, assess quickly but carefully and arrange any early investigations.
In a community setting: make arrangements for rapid transfer to hospital for further assessment.
History
This should cover the following points:
Demographic details, occupation, recent travel, history of recent abdominal trauma .
Pain:
Onset (including whether new pain or previously experienced). o o o o o o
Site (ask the patient to point), localised or diffuse.
Nature (constant/intermittent/colicky).
Radiation.
Severity.
Relieving/aggravating factors (eg if worsened by movement/coughing, suspect
active peritonitis; pancreatitis is relieved by sitting forward).
Associated symptoms: o Vomiting and the nature of vomitus (undigested food or bile suggests upper GI pathology or obstruction; faeculent vomiting suggests lower GI obstruction). o o o o o o o o o o
Haematemesis or melaena
Stool/urine colour.
.
New lumps in the abdominal region/groins.
Eating and drinking - including when the patient's last meal occurred.
Bowels - including presence of diarrhoea, constipation and ability to pass flatus.
Fainting, dizziness or palpitations.
Fever/rigors.
Rash or itching.
Urinary symptoms.
Recent weight loss.
Past medical and surgical history/medication.
Gynaecological and obstetric history: o Contraception (including intrauterine contraceptive device (IUCD) use).
Last menstrual period. o o o o o o
History of sexually transmitted infections/pelvic inflammatory disease.
Previous gynaecological or tubal surgery.
Previous ectopic pregnancy.
Vaginal bleeding.
Drug history and allergies - including any complementary medication.
Examination
Pulse, temperature and blood pressure.
Assess respiratory rate and pattern. Patients with peritonitis may take shallow, rapid breaths to reduce pain.
If there is altered consciousness, check Glasgow Coma Scale (GCS) or AVPU ( A lert, V
oice response, P ain response, U nconscious) scale.
Inspection:
o o o
Look for evidence of anaemia/
Look for visible peristalsis or jaundice . abdominal distension .
Look for signs of bruising around the umbilicus (Cullen's sign - this can be present in haemorrhagic pancreatitis and ectopic pregnancy) or flanks (Grey
Turner's sign - this can be present in retroperitoneal haematoma). o Assess whether the patient is dehydrated (skin turgor/dry mucous membranes).
Auscultation: o o
Auscultate the abdomen in all four quadrants.
Absent bowel sounds suggest paralytic ileus, generalised peritonitis or intestinal obstruction. High-pitched and tinkling bowel sounds suggest subacute intestinal obstruction. o Intestinal obstruction can also present with normal bowel sounds. o If there is reason to suspect aortic aneurysm, listen carefully for abdominal and iliac bruits.
Percussion: o Percuss the abdomen to assess whether swelling/distension might be due to bowel gas or ascites . o o o
Patients who display tenderness to percussion are likely to have generalised peritonitis and this should act as a red flag for serious pathology.
Assess for shifting dullness and fluid thrill.
Percussion can also be used to determine the size of an abdominal mass /extent of organomegaly.
Palpation: o Palpate the abdomen gently, then more deeply, starting away from the pain and moving towards it. o Feel for masses, tenderness, involuntary guarding and organomegaly (including the bladder).
o o o
Test for rebound tenderness.
Examine the groins for evidence of herniae .
Always examine the scrotum in men as pain may be referred from unrecognised testicular pathology.
Check supraclavicular and groin lymph nodes. o
Further examination: o Perform rectal or pelvic examination as needed, with an appropriate chaperone in attendance. o o o o
Check lower limb pulses if there could be an abdominal aortic aneurysm.
Dipstick urine and send for culture if appropriate.
In a woman of childbearing age, assume that she is pregnant until proven otherwise - perform a pregnancy test.
Examine any other system that might be relevant, eg respiratory, cardiovascular.
Prehospital/emergency department care of suspected acute abdomen
Keep patient nil by mouth.
Apply oxygen as appropriate.
Intravenous (IV) fluids: set up immediately if the patient is shocked and the equipment is
available. Send blood for group and save/crossmatch and other blood tests as appropriate.
Consider passing a nasogastric (NG) tube if there is severe vomiting, signs of intestinal
obstruction or the patient is extremely unwell and there is danger of aspiration.
Analgesia: the previous practice was to withhold analgesia until surgical review, but a surgical abdomen is very painful and is likely only to be adequately relieved by
parenteral opiates, eg morphine. One recent review showed that opiate administration may alter physical examination findings, but these changes result in no significant increase in management errors.
[ 6 ]
Another study showed that morphine safely provides analgesia without impairing diagnostic accuracy.
[ 7 ]
A Cochrane review also supported the use of analgesia before assessment by a surgeon.
[ 8 ]
Antiemetic : avoid using this as a symptomatic treatment without considering a diagnosis in a community setting.
Antibiotics: if systemic sepsis, or peritonitis, or severe urinary tract infection (UTI) is suspected. IV cephalosporin plus metronidazole are commonly used in acutely unwell patients in whom peritonitis is suspected.
Arrange urgent surgical/gynaecological review as appropriate.
Arrange investigations such as ECG if a medical cause is likely.
Admit: if surgery is considered likely, if the patient is unable to tolerate oral fluids, for pain control, if a medical cause is possible or if IV antibiotics are required.
Investigation
This is mainly relevant to patients being assessed in emergency departments or secondary care.
With the exception of a urinary pregnancy test and urine dipstick, there are few tests that are useful in the community assessment of the patient with acute abdominal pain.
On the whole, if you are concerned enough to be ordering blood tests or imaging, the patient should be referred to secondary care.
The following tests are often used but can be nonspecific and must be interpreted in the clinical context and with appropriate medical/surgical expertise: o Blood tests: FBC, U&Es, LFTs, amylase, glucose, clotting, and occasionally
Ca2+, arterial blood gas (ABG) (pancreatitis), calcium. o o o o o
'Group and save' or crossmatch.
Blood cultures.
Pregnancy test in women of childbearing age.
Urinalysis
Radiology - abdominal X-ray (AXR) (supine), chest X-ray (CXR) (erect looking for gas under the diaphragm), intravenous pyelogram (IVP), CT scan, ultrasound scan, as appropriate.
o o
Consider ECG and cardiac enzymes.
Peritoneal lavage if there is a history of abdominal trauma.
Red flags that raise suspicion of serious pathology
Hypotension.
Confusion/impaired consciousness.
Signs of shock.
Systemically unwell/septic-looking.
Signs of dehydration.
Rigid abdomen.
Patient lying very still or writhing.
Absent or altered bowel sounds.
Associated testicular pathology.
Marked involuntary guarding/rebound tenderness.
Tenderness to percussion.
History of haematemesis/melaena or evidence of latter on examination per rectum (PR).
Suspicion of a medical cause for abdominal pain.
Special situations
Children
Pain etiology varies with age and history. Examination can be difficult.
Always consider ectopic pregnancy in women of childbearing age. Causes of acute abdomen in late pregnancy are different and require expert combined obstetric, gynaecological and surgical evaluation.
Older patients
Tend to show less specific symptoms and signs.
Tend to present later in the course of their illness.
[ 9 ]
Morbidity and mortality in older patients presenting with acute abdominal pain are high.
[ 9 ]
You should have a lower threshold for referral to secondary care/for surgical assessment and a higher index of suspicion of serious pathology.
[ 1 ]
Aortic aneurysm and bowel ischaemia are more prevalent in the elderly.
Angiodysplasia of the colon is more common and can cause GI haemorrhage.
Medical causes of abdominal pain are encountered more frequently.
The 'Top 5' medical causes of an acute abdomen to consider in older patients are: [ 1 ]
Inferior myocardial infarction. o o o o
Lower-lobe pneumonia/pulmonary embolism causing
Diabetic ketoacidosis
Pyelonephritis .
or pleurisy hyperosmolar nonketotic coma
.
(HONK).
o Inflammatory bowel disease.
Biliary tract disease, including cholecystitis, is the most common indication for surgery in older patients with abdominal pain. This is thought to be due to age-related changes in the biliary tract.
[ 9 ]
Medicolegal pitfalls and tips
Careful documentation of the clinical situation and decision-making process is essential.
Failure to appreciate the severity of illness through not assessing vital signs/taking heed of general condition.
Failing to take note of history from carers/parents in a patient who now seems relatively
well, particularly in children.
Failure to examine adequately or to document findings.
Failure to examine for an enlarged bladder, for herniae or to check the scrotum.
Failure to carry out rectal or vaginal examination when it is indicated.
Failing to explain the reason for an intimate examination, leading to an accusation of impropriety.
Treating children as little adults and not considering paediatric-specific diagnoses.
Failing to make concrete follow-up arrangements or advising a patient of when they should seek further assessment, when managing patients in the community.
Delayed transfer of acutely unwell patients to hospital. Use the 999 service where necessary.
Steroids or other forms of immunocompromise may mask symptoms and signs.
When pain outstrips signs, consider gut infarction or AAA.
Don't rely on a normal test result to discount pathology if the clinical condition suggests
otherwise.
Failing to consider pregnancy or conduct a pregnancy test.
Be ready to reassess your initial diagnosis, or a colleague's diagnosis, where the clinical situation has changed.