notes from Exam 2

ENDOCRINE
CONDITION
Hyperthyroid
Primary vs secondary
Graves, goiter, amiodarone-induced
Who is at risk?
Family history of thyroid/AI disease
Recent pregnancy
Excess iodine
Meds (amioadarone)
Hypothyroid
(Myxedema)
Primary vs secondary
Hashimoto – hyper then hypo
Family history of thyroid disease
History of autoimmune disease (women)
Aging
Inadequate dietary iodine
Previous tx for hyperthyroidism
Hypoparathyroid
Hyperparathyroid
Primary: gland enlargement; hyper-Ca
Neck sx/radiation
Comorbidity
Family hx, heredity
Menopause
Prolonged Ca/vit. D deficiency
Neoplasm
Signs/Symptoms
Tachycardia, a-fib
Tremors
Goiter
Warm, moist skin
Hair falls out
Irritability
Heat intolerance
Hyperactiviy
Weight loss
Diarrhea
Proptosis/exophthalmos
Bradycardia
Peripheral edema
Tiredness
Amenorrhea
Weakness
Cold intolerance
Difficulty concentrating
Weight gain
Dry skin
Cold extremities
Hair breakage, dry hair
Delayed DTR relaxation
Carpal tunnel
Constipation
Hoarse voice
Hypocalcemia
Hyperphosphatemia
Numbness, tingling
Muscle cramps
Chvostek’s Trousseau’s
Bone fx/weakness
Oliguria, kidney stones, acidosis
Weakness, fatigue,
Lab/Diagnostics
Serum antibodies
Decreased TSH
Increased T3 & T4
Uptake/suppression
T4 and TSH
Antibodies (Hashimoto)
Nursing Management
Tapazole, PTU
Beta-blockers
131I
Thyroidectomy
Thyroid storm o Assess for fever, diaphoresis, S/S o Antithyroid drugs o Hormones
Post-op o Respiratory distress o Hemorrhage o Hypocalcemia o Thyroid storm
Levothyroxine (1º)
TSH stimulation (2º)
Myxedema crisis o Cardiac – IV fluids o Neuro o Respiratory – monitor; ventilator o Rewarm
P: increased
Ca and P levels
Ca: decreased
Increased PTH
Ca: increased
Bone density test =
Osteopenia: weak bones
Ca, calcitrol, vit. D
Fall and fracture prevention
Parathyroidectomy + Ca supplements (1500-2000 mg/day) o Hemorrhage
Secondary: dx causing hypo-Ca
Addison’s
1º adrenal insufficiency (AI)
Cushing’s – chronic exposure to cortisol
1º: excess aldosterone by adrenal cortex
2º Caused by excess renin
Exogenous: excess glucocorticoids (COPD,
RA)
Neck radiation
Lithium (bipolar)
Adrenal gland removal
Autoimmune disorder
Infections/invasive disease
depression, NM probs
EKG changes, HTN
Constipation, peptic ulcer
Hypovolemia
Fluid/electrolyte imbalance
Postural hypotension
LOC changes
Hyperkalemia
Fatigue, weakness
GI complaints (slow)
Decreased urine output
(adrenal crisis)
Hyperpigmentation or orange skin
Decreased libido
Obesity
Moon face, acne
Hirsutism – facial hair
Buffalo hump, striae
Plethora (excess fluid/blood)
HNT
Fatigue, muscle weakness
Hyperglycemia
Bruising
Depression to psychosis
Osteoporosis
Menstrual disorders,
Sodium, potassium,
BUN levels (low Na, high
K, high BUN)
Blood sugar (low)
Cortisol levels (low)
Urinary metabolites
ACTH stimulation test o Hypocalcemia o Laryngeal spasm o Neuro check – electrolyte imbalance o Check voice
Tx secondary disease
Non-pharm tx
Lab studies
Nutrition
Fluid – kidney stones
Fall prevention
Rest
Analgesics/comfort
Adrenal crisis o Dehycration, fever, hypoNa, hyperK, vascular collapse, death o IV hydrocortisone o Normal saline o Vasopressors o Electrolytes (Na)
Hormone replacement
Increase Na intake
Treat hypoglycemia 1st
Glucose (high)
High WBC
HypoK, HyperNa
Serum/salivary cortisol
Dexamethasone
suppression test
24-hour urine (cortisol
and Cr)
ACTH stimulation test
Aldosterone antagonist
(spironolactone)
Surgery
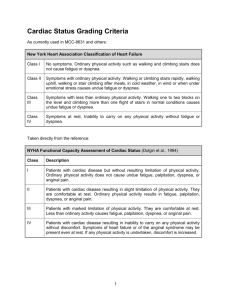
CARDIOVASCULAR
CONDITION
CAD
Angina Pectoris
Stable – predictable, goes away with rest
Unstable – unpredictable, may involve clot, vasoconstriction, risk for MI
Prinzmetal or vasospastic
Myocardial
Infarction
Who is at risk?
Increasing age
Genetic predisposition
Gender - male
Diet
Sedentary lifestyle - obesity
Smoking
High LDL
Low HDL
High total cholesterol
HTN
DM
High CRP
Same as above
Complications of angina (high
MI risk):
Increased angina duration, frequency or at rest (unstable)
ST or T wave changes
Signs of HF
Pulmonary edema
Tachycardia
Hypotension decreased libido, impotence
Kidney stones
Signs/Symptoms
Atherosclerosis
Angina pectoris
Unstable angina
Myocardial infarction
Sudden cardiac death
Supply & demand of myocardial tissue
Ischemia – ECG changes; angina pectoris
Lab/Diagnostics
Lipid panel
CRP – inflammation
Homocysteine – inflammation
Intravascular US
Cardiac cath and percutaneous coronary intervention (PCI)
Coronary angiography
Sudden onset of discomfort in chest, jaw, shoulder, back, or arm
Nursing Management
CV modifiable risk factor reduction
Physical activity
Dietary changes
Monitor weight, exercise, food intake
Support groups
Catheterization and PCI
Balloon or stent
Ca-channel blockers
Nitrates
Beta-blockers
Activity restriction
Remove precipitating factors
Supplemental O2 during pain
Assess: PQRST, hx, physical findings, VS, ECG changes
Acute: chest pain more intense than angina
Diaphoresis
SOB
Generalized weakness
May mistake S/S for indigestion
Troponin – 4-6 h post up to
4-7 days; serial pattern
Creatine kinase – (CK-NB) 6-
8 h to 48-72 h
Myoglobin – damage to heart muscle
EKG changes – place in tele
MONA - Dilate coronary arteries
Thrombolytics
CABG
Prevent ACS: O2, vasodilate, reperfuse, prevent thrombus, blood flow
IHI:
1early admin of aspirin
2aspirin @ d/c 325 mg
3beta-blocker @ d/c
Rheumatic Heart
Disease
Pericarditis
Acute infectious:
Dry vs exudative
Exudative decreases
CO and perfusion
Myocarditis
Pharyngeal strep infection – beta hemolytic
AI response (women)
Infectious:
Lung/URI
Non-infectious:
Uremia
AMI
Cardiotomy
Acute non-infectious:
Blunt trauma
Surgery & other tissue injury
Autoimmune/acute infectious:
Connective tissue disorders –
SLE, RA
Drug reactions
Rheumatoid heart disease
Pericarditis
Genetics?
Immunosuppression
Acute: open heart surgery
Infection elsewhere (viral, bacterial, fungal
AI/connective tissue dx
Drug reactions
Sarcoidosis
Hypersensitive immune rxn
Postcardiotomy syndrome
Toxins
Chest pain
Murmurs
Tachycardia
EKG changes
Friction rub
CHF
Cardiomegaly
Mitral/aortic stenosis
Anginal-type pain or sharp pleuritic-type pain
Worse with inspiration, coughing, movement, deep breathing
Worse when lying flat
Relieved by sitting up and leaning forward
Dyspnea
Infectious: high fever, chills, high WBCs, joint pain, elevated
ESR
Anorexia, weight loss, nausea
ECG changes
Pericardial friction rub
Pericardial effusion
Hoarseness, hiccups
May involve:
Heart valve function
Mural endocardium – blood clots on heart wall
Septal defect
Fatigue
Malaise
SOB
Fever
GI upset
Aching joints
CHF symptoms
H&P
CRP
ECG
Antistreptolysin O titer
Elevated WBCs
Elevated ESR
Elevated CRP
Elevated CK-MB, Troponin
CXR – pericardial eff, cardiac enlargement
Elevated WBC
Elevated ESR
Elevated CRP
Elevated CK-MB, Troponin
ECG changes
Enlarged heart and lung congestion (CXR)
Echo – depressed systolic function, dilated chambers, pericardial effusion
4ACEI/ARB if systoli dysfunction
5Reperfusion (PCI, thrombolysis)
6Smoking cessation
Early antibiotic tx
Antibiotics, NSAIDs
Steroids
Bed rest – decrease demand
Pain relief
Emotional support
Monitor for HF, change in murmur
Antibiotics
NSAIDs
Steroids
Diuretics
Anticoagulant tx
Anti-anxiety agents
Ca-Channel blockers
Nitrates
Beta blockers
ACEIs
ARBs
For pericarditis:
Pericardiocentesis
Hemodynamic monitoring
ECG monitoring
Fluid replacement
Pericardiectomy or pericardial window
Surgical resection
Endocarditis
Acute: rapid onset, virulent
Subacute: low virulent organism
Cardiac tamponade
Chemicals
Alcohol use
Nosocomial infections
Chest radiation
Recent dental sx
Illegal drug use
Weakened valves
Previous hx
PNA
Valve dysfunction
Nosocomial infections
Chest trauma
Septal defects
Bleeding gums
Long-term central line
Prosthetic valves
Congenital heart disease
Cellulitis
Rheumatic fever
Marfan’s syndrome
HIV
Pericarditis
Thoracic surgery
Trauma
Mitral valve disease Pulmonary hypertension
Decreased CO
Increased pulse pressure
Stenosis:
SCD
Fever
Chills, Night sweats
Tachycardia
Fatigue
Malaise
Anorexia
Weight loss
Headache
Arthralgias
Myalgias
Back pain
Abdominal discomfort
Clubbing
Splinter hemorrhages on nails
Petechiae
Osler’s nodes (painful lesions))
Janeway’s lesions
Roth’s spots on retina
Chest pain worsened by deep breathing or coughing
Difficulty breathing
Discomfort, sometimes relieved by sitting upright or leaning forward
Pale, gray, or blue skin - cyanosis
Palpitations - tachycardia
Rapid breathing
Dizziness
Drowsiness
Weak or absent pulse
Anxiety
Decreased LOC
Regurgitation:
Dyspnea, weakness, fatigue
Orthopnea, paroxysmal nocturnal dyspnea, peripheral
Mild elevation of WBC in IE
Elevated Erythrocyte
Sedimentation Rate (ESR) in
IE
Elevated CRP in IE
Elevated CK-MB, Troponin
Conduction delay, ST changes
CHF symptoms of ECG
CXR – septic pulmonary emboli
Elevated venous pressure
Decreased CO
Decreased BP
Loss of tissue perfusion
Narrowed pulse pressure
<30 mmHg
Beck’s triad – low BP, muffled heart sounds, JVD
Weak peripheral pulses
Pulsus paradoxus - >10 drop in SBP during inspiration
ECG – low QRS
Murmurs
Echocardiogram
Transesophageal echocardiography (TEE)
Pericardiocentesis
Hemodynamic monitoring
ECG monitoring
Fluid replacement
Pericardiectomy or pericardial window
Surgical resection
ECG monitoring for a-fib
Monitor for cardiomegaly
Maintain CO and activity tolerance
Dyspnea
A-fib
Murmur
Dry cough, dysphasia, bronchitis
Fatigue, weakness
Right-sided heart failure
Palpitations, angina
Crackles in lung bases
Hemoptysis
Aortic valve disease Decreased CO
Exercise intolerance
Stenosis:
Dyspnea, angina, fatigue, syncope that increases with exertion
Murmur
Increased pulmonary artery pressure
Prominent S4
Lung congestion
L and R sided HF
Palpitations
Tricuspid valve disorders
From rheumatic fever
Pulmonic valve disease
From congenital anomalies
Dilated cardiomyopathy
Follows MI and
Decreased CO
Increased CVP
Dyspnea
Fatigue
Peripheral edema
Pulmonary hypertension
Dyspnea, fatigue
Murmur
R sided HF
Primary: unknown etiology
Secondary: ischemia, viral infections
Alcohol intake, drug abuse edema
Murmur
Cough, crackles
A-fib
Prolapse:
Palpitations, irregular heartbeat, chest pain,
Dizziness
Regurgitation:
Murmur
Decreased DBP, widening pulse pressure
Pistol-shot femoral pulse
Head bobbing with heartbeat
Palpitations
Waterhammer pulse
Dyspnea, orthopnea, PND
Nocturnal angina w/ diaphoresis
Bounding atrial pulse, apical displaced to left
Inc SBP, dec DBP
Dizziness, exercise intolerance
L and R sided HF
Murmur
R sided HF
Low CO
A-fib
Tall peaked T waves – atrial hypertrophy
A-fib
HF symptoms
Reduced tissue perfusion
Baked up pulmonary system
Insidious onset
Chest X-Ray
Cardiac catheterization
ECG
Cardiac MRI
CXR
ECG
Echo
Cardiac catheterization
Prevent complications:
CHF
Acute pulmonary edema
Thromboembolism
Recurrent endocarditis
Increase CO
Prophylactic ABx
Cardioversion
Anticoagulation
Rest w/ limited activity
Digoxin – increase CO
SX – open up valve, replace ring, new valve
Repair
Balloon valvuloplasty
Valve annuloplasty
Replacement
Gas exchange
Activity intolerance
Pain management
Inotropics
Diuretics
Antidysrhythmics
Rest
ventricular tissue remodeling
CAD
Genetic
Idiopathic
Hypertrophic obstructive cardiomyopathy
Usually <30 y/o
Sudden death
Disorder of sarcomere
Genetic
HTN, hypoparathyroidism
Idiopathic
Restrictive cardiomyopathy
Endocardial scarring
Fibrosis & thickening
Impaired diastolic stretch
Ventricular stretch
Cocaine use
Sarcoidosis
Restrictive pulmonary disease
Arrhythmogenic
Right Ventricular
Cardiomyopathy
Electrical disturbance because of scarring in
RV
Inherited disorders
Pregnancy
HTN
CAD
Viral myocarditis
Cocaine
Calcium overload
Hyperlipidemia
Obesity
DM
Idiopathic
Chemotherapy
Genetic
Neuromuscular disorders
Endocrine (DM, Cushing’s)
Abnormal electrolytes
Antiviral meds
Cardiac valve disease
Congenital heart disease
Sleep apnea
Radiation therapy
Amyloidosis, sarcoidosis
Smoking
Familial cardiomyopathies
Cardiac surgery
Bacterial/parasitic infections
Stress, sedentary lifestyle
Toxins
Pregnancy, PP period
Connective tissue disorders
Nutritional deficiency
Genetic
Mitral/tricuspid insufficiency Endomyocardial biopsy
Radionuclide study
LV hypertrophy
Hypertrophy in septum
Sudden death, severe HF
Dyspnea
Chest pain
Presyncope, syncope
Paroxysmal nocturnal dyspnea
Echo
CXR
ECG, resting & ambulatory
Cardiac catheterization
Endomyocardial biopsy
Radionuclide study
Pulmonary/systemic congestion
Dyspnea
Palpitations, fatigue, syncope, angina, weakness, exercise intolerance
R or L sided HF
S3, systolic murmur
CXR
ECG
Echo
Cardiac catheterization
Endomyocardial biopsy
Radionuclide study
Palpitations, light-headedness, fatigue
Sudden cardiac death
RV: prominent neck veins, liver distention, swollen legs and ankles
LV: (advanced stage) fatigue,
SOB
Good family hx
Palliative
Heart transplant
Permanent mechanical assist devices
Detailed hx
ADLs
Paced/reduced activity
Positioning
O2 therapy
Find/treat underlying cause
Control S/S
Prevent progression
Improve QOL
Genetic testing
Meds
Activity restriction
Fluid stabilization
Decrease cardiac workload
Teach to avoid situations that impair venous filling or lower
CO
Heart transplant
NO OTHER CURE
Antidysrhythmic
Decrease workload
Energy conservation
May involve LV
Peripheral arterial disease
Older age
Male gender
African American
Smoking
DM
Hyperlipidemia
HTN
Peripheral venous disease
Varicose veins
DVT
Older age
Female
Obesity
Jobs w/ prolonged standing
Low-fiber diet
Smoking
HTN
Pregnancy
Injury
Immobility – SCI, paresis
Fx of pelvis, hip, long bones
Multiple trauma, burns, sx, infection, inflammation
Hypercoagulability states
Previous DVTs, PE
Malignancy
MI, HF, respiratory failure, sepsis, ulcerative colitis
ICU admission
Age >40
Obesity
Immobility 3 days or more
Varicose veins
Pregnancy, PP
Oral contraceptive use
Intermittent claudication
Muscle/limb weakness
Absent/diminished pulses
Poor hair growth
Resting limb pain
Paresthesia
Poor healing
Ankle-brachial index
Treadmill exercise arterial studies
Duplex US
Segmental arterial pressures
Angiography
CT
MRI/MRA
Lifelong aspirin tx
Meds
Angioplasty
Stenting
Radiation tx
Percutaneous transluminal angioplasty
Arterial bypass
Amputation
Acute arterial ischemia: immediate heparin tx or embolectomy
Streptokinase (not for DVT)
Vena cava filters – prevents
PE, stroke
Swelling, tightness, discomfort in one or both Les
Unilateral = DVT
Stasis dermatitis, stasis ulcers
Dilated tortuous veins
Often none
Sensation of heaviness, tiredness, itching
Visible during pregnancy or menstruation
Recurrence
Virchow’s triad:
Venous stasis
Damage of endothelium
Hypercoagulability
Asymptomatic until PE
Unilateral pain, edema, warmth, tenderness
Slightly puffier than other leg
Homan’s sign
Duplex US
Venography
CT and MRI
Venous duplex imaging
Photoplethysmography
Ambulatory venous pressure
Ligation
Stripping
Laser therapy
Radiofrequency ablation of vein
Wear compression stockings after venous sclerotherapy
Avoid venous pooling
Walking program, weight loss
Early ambulation as tolerated
Elevate 10 to 20º above level of heart
Moist heat
AVOID MASSSAGING
Graduated compression stockings
Anticoagulants (heparin, thrombin inhibitors, warfarin)
Venous thrombectomy
Percutaneous interruption of vena cava
AROM, PROM
Avoid prolonged sitting, standing, crossing legs
Intermittent pneumatic
Abdominal aortic aneurysms and dissection
Dissection
Life-threatening, tear in the lumen
Diminished blood supply distal to dissection
Central venous catheters
Major surgery
Heart Failure
Neurohormonal response
SNS activation
RAAS activation – sodium and fluid retention, myocardial hypertrophy
Cardiac remodeling
Exacerbation and stabilization
HTN
CAD
Dilated cardiomyopathy
Hyperlipidemia
Metabolic syndrome
Obesity
Sedentary lifestyle
Smoking
Valvular abnormalities
Age
Family hx of CAD
Gender
Genes
Often asymptomatic
Pain with gnawing quality, unaffected by movement, lasts for hours/days
Pain in abdomen, flank, back
Pulsatile abdominal mass
Activity intolerance
Fluid retention
SOB
Fatigue
L-sided: fatigue, activity intolerance, SOB, cough, orthopnea, paroxysmal nocturnal dyspnea
R-sided: abdominal bloating and discomfort, poor appetite, nausea
Bivent: combination of L and R
Confusion, forgetfulness, loss of concentration, disorientation
Cardiac cachexia
JVD
Crackles
Abdominal imaging (X-rays)
CT – size and location
Aortic angiography
Abdominal US
Abdominal angiography
MRA
AAA >3cm in diameter
LV systolic dysfunction:
Volume overload
Decreased contractility
LVEF < 40% to 45%
Diastolic Dysfunction
HF with normal LVEF
Slow relaxation
HTN, DM, obesity, a-fib
Reduced stroke volume
Stiff heart
CBC – anemia, liver/renal
BNP – LV stretch, high
High microalbumin
Electrolytes & Cr
Liver function test
Urinalysis devices
Venous foot pumps
Monitor growth with abdominal US q6 months
Maintain normal BP - meds
Smoking cessation
Control of fasting lipid
D/C steroids
Endovascular stent graft
Surgical repair, endovascular repair
Monitor S?S of impending rupture:
Restlessness
Abdominal pain, tenderness
Prep for emergent sx
Post-op care:
Risk factor reduction
Wound care
Activity restriction
Medication regime
Reportable symptoms
Meds if <5.5 cm
Cool forearms and legs
Assess response to diuresis
Assess CO
Monitor I&O
Monitor for dysrhythmias
Encourage increasing levels of activity
Perform ADLs
Patient knowledge of dx
O2 sat – administer O2
Assess temperature
Assess for cyanosis
Assess neuro status
Auscultate
Meds
Cardiac devices
Control comorbidities
RESPIRATORY
CONDITION
Obstructive Sleep
Who is at risk?
Obesity
Cough
Abrupt decline in CO:
Narrow pulse pressure
Althered mentation
Hypotension
Resting tachycardia
Oliguria
Tachypnea
Signs/Symptoms
Serum ferritin
Lipid panel
Digoxin level
ABGs
CXR – enlarged heart, patchy infiltrates
EKG
Echo – ejection fraction
Cardiac cath R or L
Selective coronary angiography
Cardiac MRI
Lab/Diagnostics
Adequate hours of sleep but no Polysomnography in sleep
Control volume status
Cardiac transplant or mechanical assist device
Reduce readmission
Palliative care
Echo, ACEI or ARB if EF<40% unless C/I
Smoking cessation
Fluid restriction
Dietary changes
Refer to community resources
Educate: meds, activity, weight
UNLOAD FAST upright nitrates lasix oxygen aminophyllin digoxin fluid restriction after load - decrease sodium restriction test - digoxin levels, ABGs,
BNP
7 Key interventions
LVS heart function assess
ACEI/ARB @ d/c
Anticoagulant w/ a-fib
Flu vaccine
Pneumococcal vaccine
Smoking cessation counsel
D/C instructions: activity, diet, meds, follow-up, weight, worsening S/S
Nursing Management
Change of sleep position
Apnea
Upper airway obstruction
Life-threatening
Head and Neck
Cancer
Pneumonia
Smoking
Age > 65
Male gender
Postmenopausal females
Foreign bodies
Infectin
Smoke
Anaphylactic reaction
Angioedema
Smoking
Excessive alcohol energy the rest of the day
Inability to concentrate
Irritability laboratory
H&P
Weight loss
CPAP or BiPAP
Denoidectomy
Uvulectomy
Antibiotic therapy
Immunocompromised
Stroke, trach, dysphagia, near drowning, post op N/V
Dyspnea
Hypoxemia
Ventilation-perfusion mismatch
Fever, chills
Increased RR
Rusty bloody sputum
Crackles
X-ray abnormalities
Non-respiratory symptoms
Dehydration
CXR – usually upper lobe densities
Radiation therapy – dysphagia, nutrition
Chemotherapy
Radical neck dissection – puts airway at risk
Laryngectomy:
Good suctioning
Care of permanent trach
Communication support
Nutrition – dysphagia
Body image issue
Maintain airway/ventilation
Wound care
Bleeding –behind neck
Pain management
Nutrition
Speech/language rehab – esophageal speech
Stoma care
Smoking cessation
Psychosocial
High risk for lower airway infection
Administer ABx
Airway – O2 sat > 93%
Nutrition, hydration
Small, frequent, high-carb, high-protein meals
Bronchodilators
Suction, C&DB
IS
Gradual increase in activity, sit up for meals
Pulmonary tuberculosis
Lung abscess
Necrotizing PNA
Bacterial, fungal, parasitic
Pulmonary empyema
COPD: Emphysema
COPD: Chronic bronchitis
HIV/AIDS
Immunocompromised
Dyspnea
Weight loss
Cough
Sputum production
Sleep disturbances
Rust colored sputum
Night sweats
Low grade fever
Advanced:
Activity intolerance, fatigue
Low grade fever, night sweats
Blood-streaked sputum
Dullness w/percussion over involved area
Bronchial breath sounds, increased transmission of whispered sound
Pus in the lung itself
Fever
Chills
Chest tube for pleural effusion Pus in pleural space
Dyspnea/wheezing
Use of accessory muslces
Vent/perfusion mismatch
Decreased forced expiratory volume
Involvement of alveoli
Cachexia
Barrel chest
Changed muscle definition
Clubbing – chronic hypoxia
Dyspnea/wheezing
Use of accessory muslces
Tuberculin skin test – read
48-72 hours, 10mm (5mm for immunocompromised)
CXR – if BCG vaccinated
Acid-fast bacillus smear – 3 positives on 3 different days
Sputum culture
Nutrition, fluid
Avoid exposure to others with infections
Meds
S/S to watch out for
Drug tx
Negative pressure room
Airborne isolation until 3 sputum cultures are neg
Pain management
Fatigue management
Good nutrition
ABG:
PaO2 <80-50 mmHg
PaCO2 – increased to 50
Polycythemia vera – high
H/H
Sputum samples
Serum electrolytes
Serum AAT levels
CXR:
Emphysema = Lots of black space/air
High-dose antibiotics
Drainage of pus
Re-expand the lung
Control the infection
Assess O2 first
Admin O2
Antibiotics - infection
Bronchodilators – reduce airway resistance
Anticholinergics – bronchodilate and decreases secretions
Corticosteroids – decrease inflammation, decrease bronchoconstriction
Pleural effusion CHF
Bacterial PNA
Malignancy
Vent/perfusion mismatch
Decreased forced expiratory volume
Involves airway
Inflamation, vasodilation, congestion, mucosal edema, bronchospasm
Airway enlargement
Large amount of thick mucus
Hypoxemia
Acidosis
Respiratory infections
Cardiac failure – cor pulmonale
Cardiac dysrhythmias
Clubbing – chronic hypoxia
Bronchitis = not enough air, clouding over
Pulmonary function test
Impaired gas exchange;
Airway
Cough & DB
O2 therapy
Pulmonary rehab
Ineffective breathing pattern
Specific breathing techniques
Positioning – dyspnea
Energy conservation
Diaphragmatic breathing
Pursed-lip breathing
Relaxation techniques
Positioning
Ineffective airway clearance
Chest physiotherapy w/ postural drainage
Suctioning
Positioning
Hydration
RT – flutter valve
Tracheostomy
Imbalanced nutrition
Activity intolerance
Anxiety
Potential for PNA
Avoid large crowds
PNA vaccine
Flu vaccine
Indwelling pleural catheter w/ intermittent drainage
Pleural-peritoneal shunt
Thoracentesis
Pleurodesis
Pleurectomy
Chest tube – pleural space
RENAL
CONDITION
Polycystic kidney disease
Hydronephrosis
Also:
Hydroureter
Urethral stricture
Pyelonephritis
Who is at risk?
Congenital anomaly
Enlarged prostate
Urethral/ureteral strictures
Renal calculi
Abdominal tumors
Blood clots
Ureteritis/prostatitis
Neurogenic bladder
Congenital abnormalities
Women
Inability to empty bladder
Sexually active
Pregnancy
Diabetes
Compromised renal function
Instrumentation
Signs/Symptoms
Abdominal/flank pain
HTN
Increased abd girth
Constipation
Bloody/cloudy urine
Kidney stones
Uremia and death
Slight discomfort
Slightly decreased urine flow
Acute: Severe, colicky renal/flank pain
Chronic: vague abd/back pain
May be unilateral
Fever, nausea
Pain on urination
Fever, chills, tachycardia, tachypnea
Flank/back/loin pain
Abdominal discomfort
N/V, urgency, frequency, nocturia
Malaise or fatigue
Chronic:
HTN
HypoNa
Decreased concentration
HyperK and acidosis
Lab/Diagnostics
Ultrasonography, tomography, radioisotope scans
Retrograde ureteropyelography
Urinalysis - for protein/blood
Serum Cr >1.5 mg/dL
BUN >25 mg/dL
Intravenous pyelogram (IVP)
Renal US
BUN, Cr, Cr clearance
Urinalysis
Cloudy urine
Foul smelling urine
Low specific gravity
Proteinuria
Hematuria
Positive WBC
Casts
Urine culture
KUB
Repiratory assessment
Assess site
Assess system – upright, below chest, patent, water levels, no air leaks, drainage, tubing - kinks
Flap or shunt if pneumothorax - air
Nursing Management
Preserve renal fxn, prevent complications
Control HTN
Dialysis
Treat cause of obstruction
Remove obstruction
Prostatectomy
Dilation of stricture
Sx removal of stone/tumor
Nephrostomy tube
Diet low in protein, Na, K
Check for bleeding, hematuria, infection
Antipyretics
Clean-catch urine specimen
Antibiotic tx
2,000-3,000 mL fluids/day
Activity & rest
Urinary analgesics
Glomerulonephritis
May cause nephrotic syndrome
Prior strep infection - acute
Males
Younger age (5-15 y/o)
SLE
DM
Goodpasture’s syndrome
Blood in urine (dark, rustcolored, brown)
Foamy urine (excess protein)
Edema (generalized)
Acute: no pus, no bacteria
HTN
Hypoalbuminemia
High cholesterol
N/V, fever, rash
Low urine output
Nephrotic syndrome
Acute renal failure
Sudden onset, reversible
CKD
Chronic renal failure
ESRD (loss of 7/8 of filtration capacity)
Insidious, chronic, irreversible
Diabetes
Drugs that cause kidney damage
Glomerulonephritis
Increased age
Vascular disease
Diabetes
African American
Men
Age 65 and older
Hereditary diseases: polycystic kidney disease, Alport syndrome
Diabetes
HTN
High levels of protein in urine – foamy urine
Low levels of protein in blood - hypoalbuminemia
Edema (generalized)
High cholesterol
HTN
Low urine output
Early signs:
Oliguria
Azotemia
Anuria
Late signs (systemic):
SEE BELOW
HTN or hypotension
Anasarca (total edema)
Coagulation changes
Metabolic acidosis – ammoniabreath, Kussmaul’s
HyperK – cardiac arrest
HypoNa, fluid overload
Tumorlike calcium precipitates
Neuro: confusion, lethargy, decreased LOC, stupor
GI: N/V, anorexia, distention, constipation or diarrhea
Respiratory: crackles, pulmonary edema, pleural eff, risk for infection
Urinalysis
Proteinuria
Hematuria
Casts
Elevated Cr
Decreased Cr clearance
Elevated serum antistreptolysin-O titer
Urinalysis
Protein (high)
Serum protein (low)
Lipid panel (high cholesterol)
Chronic:
BP
I&O
Daily weight
Dietary plan (low protein, low
Na)
Diuretics & anti-HTN
Corticosteroids
Plasmapheresis
Teaching:
Nutrition, meds, skin care
(pruritis, edema), infections
Address underlying cause
May develop CKD -> ESRD
Corticosterioids
ACEI – BP down, decrease protein loss
Heparin
Low-salt diet
Mild diuretics
BUN, Cr, K, PO4 – increased
Na, Ca – decreased
U/A: RBCs, casts, proteinuria, low sp.gr. low osmolality
GFR – lower than 40 or decreased by >75% (failure)
Increased BUN and Cr
Increased BUN/Cr ratio
Increased serum PO4
K normal or elevated
Decreased Na, HCO3 and Ca
Renal failure
Maintain fluid balance
Protein intake 0.8 g/kg/day
25-35 kcal/kg – high carb
Monitor K
Adjust meds, avoid NSAIDs,
ACEI
Avoid Mg antacids
Control metabolic acidosis
Strict aseptic technique
Remove indwelling caths
Avoid nephrotoxic agents
Watch for infections
Monitor drug levels
Low protein, low Na, low K levels
Monitor electrolytes
Prevent injury
Fatigue/weakness
Peritoneal Dialysis
Hemodialysis
NEUROLOGICAL
CONDITION
Multiple Sclerosis
Urinary tract obstruction
Chronic glomerulonephritis
Chronic infection
Acute tubular necrosis
Nephrotoxic agents (antibiotics,
NSAID, contrast media)
Hyperkalemia (also Kayexalate, glucose & insulin, bicarb, calcium gluconate)
Who is at risk?
Women (AI)
Cold climates
Genetic factors
CV: tachycardia, dysrhythmia, rub, pericarditis, inc BP
Skin: dry, pruritis, edema, bruising, pallor, uremic frost
HyperK, HypoNa, HypoCa, hyper-PO4
Complications:
Infection – biggest risk
Peritonitis – rigid, board-like abdomen
Poor dialysate flow
Dialysate leakage
Oliguria/anuria
Azotemia (high BUN)
Complications:
Thrombosis/stenosis
Infection
Aneurysm
Ischemia
Heart failure
Dialysis disequilibrium syndrome
CNS – big change in osmolality cause fluid shift into cerebral cavity = cerebral edema: HA, dizziness, disorientation, restlessness, blurred vision
Confusion, seizures, coma, death
Signs/Symptoms
Remission and exacerbation
Exacerbation: triggered by fatigue, stress, illness
Fatigue
Muscle control difficulties
Flexor spasms at night
Intention tremors
Gait disturbances
Lab/Diagnostics
More on symptomatology
CSF studies:
Elevated IgGs
Presence of oligoclonal bands
MRI: white matter lesions
Genetic markers
CBC outside normal
R/O syphilis, HIV, heavy
Monitor ECG, neuro
Dialysis
Monitor H&H
Administer epogen
Skin integrity
Note dwell time, initiate outflow
Should be getting more than what was put in, clear fluid
Use gravity to get extra fluid out
Warm fluid to prevent pain
No heparin
Evaluate VS, weight, labs
Monitor for respiratory distress, pain, discomfort
C/I: hemodynamic instability, lack of access, inability to anticoagulate
Planning:
Meds
Meals – no meals right before
Activities – no heavy lifting, no BP on side with line
No invasive procedures or blood draws
Weight, BP, labs
Assess for hypotension, HA,
N/V, malaise, dizziness, muscle cramps, bleeding
Nursing Management
Motor function, ADLs
Symptom mgmt.
Self-care and safety
Energy, ability to perform
ADLs
Ability to void normally
Meds for paresthesias, pain, bowel dysfunction
Amyotrophic Lateral
Sclerosis (ALS)
Guillain Barre
Syndrome
Genetic/family hx
Men in their 30s
Previous viral infection
Myasthenia Gravis
FACE – cranial nerves
Thymoma
Myasthenic crisis: increased droopy eye
Cholinergic crisis: abdominal cramps,
Younger women, older men
Blurred vision, diplopia, nystagmus
Tinnitus, vertigo
Hypalgesia – decreased feeling
Numbness, tingling, burning
Bowel/bladder dysfunction
Late cognitive changes in memory, concentration, judgment, depression
Slurred speech - dysarthria
Falling
No cognitive defects, always motor
Upper and lower motor weakness
Muscle atrophy
Dysphagia, fasciculations
Spasticity, cramping, fatigue
Twitching of limb, tongue
Dyspnea
Motor weakness
Areflexia
Flaccid paralysis
Ascending (sometimes descending) symmetrical weakness progression
Paresthesia and pain
Autonomic changes
No pupillary/cerebral S/S
Changes in cardinal vision, diplopia
Specific muscle weakness
Voluntary muscle fatigue
Ptosis (droopy eyelids)
Diplopia
Dysarthria (speech)
Dysphagia (swallowing)
Snarling look
NO COGNITIVE metal poisoning, stroke, brain tumor
EMG: fibrillations
CBC outside normal
Genetic markers
R/O syphilis, HIV, heavy metal poisoning, stroke, brain tumor
CBC outside normal
Tensilon testing –increase
Ach if improved, myasthenic crisis
EMG: fibrillations
CBC outside normal
R/O syphilis, HIV, heavy metal poisoning, stroke, brain tumor
Steroids for exacerbations
Biological modifiers
Antidepressants
NO CURE
Education:
Avoid stress, extreme temps, infections
Exercise & mobility program
ADLs and muscle function
Antispasticity meds
Exercise & mobility program
Periods of rest
Manage swallowing, resp
Support groups
Comprehensive baseline assessment
Ongoing monitoring
Assess pain
Provide support for fearful patients
Antivirals – reversible
Pain management
NO CORTICOSTEROIDS
IV immunoglobulin
Plasmapheresis
Ineffective Breathing Pattern
Cardiac Dysfunction
Periods of rest around mealtimes
Cholinergic crisis – overmedication; withhold meds; atropine, airway
Myasthenic crisis – undermedication; maintain respiratory fxn; reintroduce meds little by little
diarrhea, bronchospasm, increased secretions
Both muscle weakness
Parkinson’s
Alzheimer’s
Meningitis
Bacterial is most dangerous
Viral: self-limiting, more common, less fatal
Encephalitis
Usually viral
Bacterial:
Immunocompromised
Malnutrition
Alcoholism
DM
Recent dental tx
Bacterial sinus infections
Mosquito bites
Warmer climate
Postviral from measles, mumps, chickenpox
Meningismus (irritation)
Photophobial
Nuchal rigidity
Kernig’s sign (bend hip)
Brudzinski’s sign (bend neck)
Severe headache
High fever
Seizures at onset
Altered LOC late sign
+ Kernig’s & Brudzinski’s
Brain hemorrhage/necrosis
Severe headache
Fever
CPK levels: elevated
Abnormal EEG
Genetic markers
R/O syphilis, HIV, heavy metal poisoning, stroke, brain tumor
R/O hypo/hyperthyroid
CPK levels: elevated
MRI: brain atrophy
CRP levels: elevated
Genetic markers
R/O syphilis, HIV, heavy metal poisoning, stroke, brain tumor
R/O hypo/hyperthyroid
Hx of illnesses, dental tx, trauma
Lumbar puncture
Counterimmunoelectrophoresis
PCR
Lumbar puncture
Low glucose
High protein
High WBCs
Cholinesterase-inhibitors
Immunosuppressants
Plasmapheresis in crisis
IV immunoglobulins in crisis
Thymectomy
Administer meds w/ food to prevent aspiration
Monitor airway, swallowing
Promote self-care
Assist w/ communication
Nutritional support
Eye protection
Avoid infection, stress, overheating
Prophylactic ABx, broadspectrum
Mannitol
Anticonvulsants
Steroids
Pain management
Antipyretics
Support respirations
Manage ICP
Nutritional support
I&O
Seizures
Status Epilepticus
30 minutes of seizure activity
2+ w/o full consciousness in between
Respiratory/CV failure
SPINAL CORD
INJURIES
CONDITION
Hyperflexion injuries
Hyperextension injuries
Who is at risk?
MVA (sudden deceleration)
Rotational injuries
Age – degenerative changes
MVA
Sudden impact from high-energy trauma MVA both sides
Compression
Injuries
Fall from a height
Diving into shallow pond
Age – degenerative changes
Penetrating injuries Projectile injury
N/V
Confusion
ALOC
Focal deficits – motor weakness
Seizures
Bizzarre behavior
Cerebral edema – seizures, loss of sensation, speech, hearing, consciousness
Death if untreated
Uncontrolled motor activity
Drooling
Airway problems
Aura
Pupillary constriction or dilation
Loss of consciousness
Cyanosis
Urinary incontinence
Signs/Symptoms
MRI
CT scan
Blood/urine/throat CX
EEG
Brain biopsy
CT scan for structural problems
EEGs – what seizure looks like
ISAP – location of seizure
Lab/Diagnostics
Where is the level of injury – how much function can a pt have
Umbilicus at T10
Clavicle C3-C4
Finger movement if injury is lower than C7
C6 and above – no hand movement, may be able to drive a chair
T6 – lower extremities affected
Antivirals
Dexamethasone to reduce cerebral edema
Antiepileptics
Pain management
Antipyretics
Airway – lie on side
Safety precautions
Anti-epileptics – S/E, toxicity
Sx resection
Anxiety
Knowledge deficit
Fear
Risk for Injury
Time the seizure
Nursing Management
Airway and respirations
Shock, CV problems
Hemorrhage
LOC – use GCS
Stabilize spine at level of injury
High dose glucocorticoid – anti-inflammatory
SX management – unstable fracture, cord compression
(laminectomy, fusion)
Skin breakdown prevention
Bowel/bladder/sexual fxn
Assess for autonomic dysreflexia, manage
Psychosocial changes
Rehab:
Motor function
Communication
Then:
Cervical spine injuries
Thoracic &
Lumbosacral injuries
Spinal shock
Secondary injury
Chronic SCI
Autonomic
Hyperreflexia
(autonomic dysreflexia)
C1-C3 – breathing muscles paralyzed
C4-8 – impaired breathing
Risk for PNA, atelectasis
Risk for PE
T1-T11 – impaired cough
T12 and below – breathing and coughing normal
Immediately after a spinal injury
Flaccid paralysis
Loss of reflexes below lesion
Bradycardia
Paralytic ileus
Hypotension (SBP<90 - treat)
After a spinal injury
Neurogenic shock
Hypovolemic shock
Spinal shock
Decreased ANS response
Bradycardia
Hypotension
Hypotension
Bradycardia
Edema of LE
Weak cough
Response to noxious stimulus
Distended bladder
Pressure ulcer
Tight clothing
High BP - severe
Bradycardia
Severe HA
Nasal stuffiness
Flushing
Spasticity May occur weeks to months after SCI
Skin Breakdown
GU/Bowel
Impaired tissue perfusion
Tissue hypoxia
Spinal tracts disrupted
Pain
Stretching
Infection
Skin breakdown
Loss of fxn S1-S4
Bowel/bladder
Adaptation
Fixed skeletal traction
Pin site care, monitor traction rope
Halo fixation, cervical tongs
Stryker frame
Assisted coughing, IS
Body cast
Braces or corset
Meds to increase BP
CV assessment
Manage temperature (hypothermia)
Stabilize cord
Rounded abdomen
Spasticity
Temperature intolerance
Pain
Muscle spasms
Raise HOB to 90, lower legs
Loosen tight clothing
Check urine
Check bowels
Check for painful things
Remove cause
BP reduction - meds
Perform daily ROM exercise
Monitor for skin breakdown
Meds (Baclofen, Valium)
Weight shifts q15min
Turn q2-3h
Skin checks
Foley
Sexual
Psychosocial
SCI
Long-term catheterization Loss of urge to urinate, control of sphincter
Inability to sense fullness
UTI
Hydronephrosis
Decline in renal fxn
Renal calculi
Constipation
Incontinence
Hemorrhoids
Ileus
Loss of psychogenic erection
Reflex (physical stimulation) may still be present
Loss of body image, independence, control, economic security
Lifestyle changes
Stress, strain on relationships
Withdrawal from social
Avoid eye contact
Refuse to participate
Suprapubic catheter
Intermittent cath
Mitrofanoff (sx – use appendix between bladder and stoma)
Meds for BM
Scheduled BM
Viagra
Injection therapy
Vacuum pump
Surgical implant
Monitor for inadequate coping
Encourage to discuss feelings
Allow to participate in decision-making