Respiratory system
advertisement
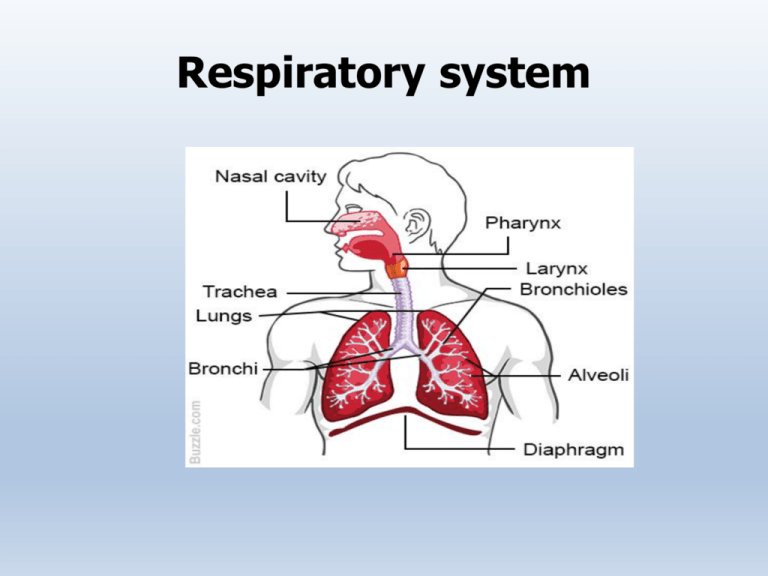
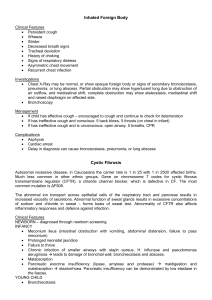
Respiratory system Symptoms / Chief complaint • Cough • Sputum • Hemoptysis • Dyspnea • Chest pain (chest tightness / discomfort) • Wheezing Symptoms / Chief complaint • Cough • Sputum • Hemoptysis • Dyspnea • Chest pain (chest tightness / discomfort) • Wheezing Cough • Type – Dry, Productive , Short, Brassy, Bovine ,Barking , whooping, Cough syncope, Nocturnal, Drug induced • Onset & Duration • Pattern : activities, time of day, weather • Severity • Timing and associated features Causes of cough: Normal chest X-ray Abnormal chest X-ray Acute cough Viral respiratory tract infection, (<3 weeks) Bacterial infection (acute bronchitis), Inhaled foreign body, Inhalation of irritant, dusts/fumes Pneumonia, Inhaled foreign body, Acute hypersensitivity Pneumonitis Chronic cough (>8 weeks) Lung tumor, TB, Interstitial lung disease, Bronchiectasis GERD, Asthma, Post viral bronchial hyper reactivity, Rhinitis/sinusitis, Cigarette smoking Drugs (ACE inhibitors, Irritant dusts/fumes) Macleod’s Clinical examination 13th edition ‘Reg Flag’ symptoms Macleod’s Clinical examination 13th edition Sputum • Sputum is mucus produced from the respiratory tract. The normal lung produces about 100 ml of clear sputum each day, which is transported to the oropharynx and swallowed • Amount • Color • Presence of blood (hemoptysis) • Odor • Consistency Color & Consistency: Type Appearance Cause Serous Clear, watery, Frothy, pink Alveolar cell cancer, Acute pulmonary oedema Mucoid Clear, grey Chronic bronchitis/COPD White, viscid Asthma Yellow Acute bronchopulmonary infection Asthma (eosinophils) Purulent Rusty Green Longer-standing infection, Pneumonia Bronchiectasis, Cystic fibrosis, Lung abscess Rusty red Pneumococcal pneumonia Macleod’s Clinical examination 13th edition Macleod’s Clinical examination 13th edition Haemoptysis • coughing up blood from the respiratory tract Macleod’s Clinical examination 13th edition Causes Malignant • Lung cancer • Endobronchial metastases Benign • Bronchial carcinoid Vascular • Pulmonary infarction • Vasculitis • Iatrogenic • Transthoracic lung biopsy • Acute left ventricular failure • Polyangiitis • Inhaled foreign body • Mitral valve disease • Blood dyscrasias Infection • Bronchiectasis • Lung abscess • Mycetoma • Cystic fibrosis • Tuberculosis • Arteriovenous malformation • Goodpasture’s syndrome • Bronchoscopic biopsy • Bronchoscopic diathermy • Anticoagulation • Trauma • Chest trauma • Haematological Dyspnoea • Dyspnoea (breathlessness) is undue awareness of breathing and is normal with strenuous physical exercise. • Patients use terms such as ‘shortness of breath’,‘difficulty getting enough air in’, or ‘tiredness Grades: M R C classification: – Grade I: Breathless when hurrying on the level or walking up a slight hill – Grade II: Breathlessness when walking with people of own age or on level ground – Grade III: Walks slower than peers, or stops when walking on the flat at own pace – Grade IV: Stops after walking 100 metres, or a few minutes, on the level – Grade V: Too breathless to leave the house (Too breathless to wash or dress ) Macleod’s Clinical examination 13th edition Modes of onset, duration and progression Minutes • Pulmonary thromboembolism • Pneumothorax, Asthma, Inhaled foreign body • Acute left ventricular failure Hours to days • Pneumonia, Asthma , Exacerbation of COPD, LHF Weeks to months • Anaemia, Pleural effusion, Respiratory neuromuscular disorders Months to years • COPD, Pulmonary fibrosis, TB, Muscle weakness Macleod’s Clinical examination 13th edition Variability • Orthopnoea :Breathlessness when lying flat (LVF) • Platypnoea: Breathlessness on sitting up with relief on lying down right-to-left shunting • Trepopnoea : Breathlessness when lying on one side is due to unilateral lung disease dilated Cardiomyopathy • Paroxysmal nocturnal dyspnoea : wakes the patient from sleep • Breathlessness improving at weekends or holidays occupational asthma. Causes of Breathlessness • Cardiorespiratory – – – – – Anaemia Metabolic acidosis Obesity Psychogenic Neurogenic • Cardiac – – – – – Left ventricular failure Mitral valve disease Cardiomyopathy Constrictive pericarditis Pericardial effusion Macleod’s Clinical examination 13th edition Respiratory Airways • Laryngeal tumour • Foreign body • Asthma • COPD • Bronchiectasis • Lung cancer • Bronchiolitis • Cystic fibrosis Pulmonary circulation • Pulmonary thromboembolism • Pulmonary vasculitis • Primary pulmonary hypertension Parenchyma • Pulmonary fibrosis • Alveolitis • Sarcoidosis • Tuberculosis • Pneumonia • Diffuse infections, e.g. Pneumocystis jiroveci pneumonia • Tumour (metastatic, lymphangitis) Pleural • Pneumothorax • Effusion • Diffuse pleural fibrosis Chest wall • Kyphoscoliosis • Ankylosing spondylitis Neuromuscular • Myasthenia gravis • Neuropathies • Muscular dystrophies • Guillain–Barré syndrome Macleod’s Clinical examination 13th edition Chest pain • Chest pain can originate from the parietal pleura, the chest wall and mediastinal structures . • Pleural pain • Chest wall pain • Mediastinal pain • Retrosternal pain – Upper – Lower Causes of Chest pain Non- Central Pleural • Infection: pneumonia, bronchiectasis, tuberculosis • Malignancy: lung cancer, mesothelioma, metastatic • Pneumothorax • Pulmonary infarction • Connective tissue disease: rheumatoid arthritis, SLE Chest wall • Malignancy: lung cancer, mesothelioma, bony metastases • Persistent cough/breathlessness • Muscle sprains/tears • Bornholm’s disease (Coxsackie B infection) • Tietze’s syndrome (costochondritis) • Rib fracture, • Intercostal nerve compression, • Thoracic shingles (herpes zoster) Central Central Tracheal • Infection • Irritant dusts Cardiac • Massive pulmonary thromboembolism • Acute MI/ ischaemia Oesophageal • Oesophagitis • Rupture Great vessels • Aortic dissection Mediastinal • Lung cancer • Thymoma • Lymphadenopathy • Metastases • Mediastinitis • Past History – Similar illness – TB, Asthma, IHD, DM – Childhood illness- measles, inflenza, whooping cough – Recent travel • Family history – Similar illness – DM,TB, HT, IHD, – Parents marriage: consanguineous – Asthma, Eczema • Personal history – – – – – Appetite Veg/non-veg Bowel & bladder Alcohol- amount & duration Smoking-No., duration (smoking index) • Menstrual history – Menarche, LMP – Regular, amount – Associated pain • Treatment History General examination • • • • • • • • • • Built Nourishment Dyspnoea Cyanosis Anemias Jaundice Clubbing Lymphadenopathy Eye Pedal edema Cyanosis Grades and Examination of Clubbing Causes of clubbing A. Bronchopulmonary diseases • Bronchiectasis • Lung abscess • Bronchogenic carcinoma • Emphysema B. Cardiac diseases • Congenital cyanotic heart disease • Subacute bacterial endocarditis Lymphatic and Veins • Lymph node: – Parietal pleura axillary lymph node – Whole right lung& left lower lobe right supraclavicular lymph node – Left upper lobe left supraclavicular lymph node • Veins: – Superior vena caval syndrome Examination of the neck • Scalene Lymph Node – Large and fixed : Primary lung malignancy – Hard, craggy, matted, with/out sinus formation: calicified TB lymphadenopathy • Other significant nodes: – Supraclavicular – Cervical – Axillary External manifestations • • • • • • • Asterixis Halitosis Gynaecomastia Horner’s syndrome Small muscle wasting External markers of TB External markers of cor pulmonale Examination What is the most important start to any exam ?? Introduce yourself to the patient and let them know what you are about to do … Take consent before examination! Systemic Examination of Respiratory system Inspection/Observation • Upper Respiratory Tract – Oral – Nosecavity – Pharynx - Tonsils -Throat • Lower Respiratory Tract – Supraclavicular area – Infraclavicular area – Mammary region – Axillary region – Infra axillary region - Suparscapular region -Interscapular region - Infrascapular region • Shape • Bilateral movement • Subcoastal angle • Dyspnea • Accessory muscles • Trachea position • Apex beat • Shoulder drooping • Spine position • Visible scars/ dilated veins/ sinuses • Position of Trachea: – Trail’s sign • Position of the apex beat Chest Deformities • Flat chest • Barrel chest • Pectus Carinatum • Pectus excavatum: It’s the exaggeration of the normal hollowness over the lower end of the sternem. • Harrison’s sulcus: • Rickety rosary: • Scorbutic rosary: Spine Abmormalites • Kyphosis: Causes the patient to be bent forward. • Ankylosing spondylitis: Diminished volume of lung & capacity of the chest • Scoliosis: spine is curved to either the left or right. Movement of the chest • Rate • Rhythm • Equality • Type of breathing Rate • • • • Normal: 14-18 breaths/min Type of breathing Pulse : Respiratory rate (4:1) Tachyponea: – Nervousness, fever, hypoxia, exertion – APE, Pneumonia, Pul. Emobolism, ARDS, Metabolic acidosis • Bradypnoea: – Alkalosis, Hypothyroidism, raised ICT • Hyperpnoea: – Acidosis, brainstem lesion, Hysteria Rhythm Inspiration: by the contraction Of the external intercostal muscles and the diaphragm Expiration: Depends upon the elastic recoil of the lungs Abnormal breathing patterns • Cheyne-Stokes respirations – Hyperpnoea followed by apnoea – periods of respirations during which the tidal volume starts shallow and gets progressively deeper, and then gets progressively shallower. – Causes: strokes, traumatic brain injuries, brain tumors, CO poisoning, and metabolic encephalopathy, normal side-effect of morphine administration. • Kussmaul's Breathing: – Labored hyperventilation characterized by a deep and rapid respiratory pattern. – Causes: late stages of a severe metabolic acidosis (DKA). • Apneustic Breathing: – prolonged inspiratory phases with each breathe, followed by a prolonged expiratory phase – causes: lesion to the upper part of the pons • Ataxic Breathing: – A completely irregular breathing pattern with irregular pauses and unpredictable periods of apnea. – Cause: lesion to the medulla oblongata secondary to trauma or stroke. – very poor prognosis. • Biot's Breathing • Apnoea between several shallow or few deep inspirations • It is very similar to Cheyen-Stokes except the spontaneous tidal volume is equal throughout the period of respiration. • Causes: Lesions to the medulla oblongata by CVA or trauma, or pressure on the medulla due to uncal or tenorial herniation, prolonged opioid abuse. Palpation • • • • • Position of the trachea Apex position Rib crowding Bony tenderness Lymphnode – Axillary – Cervical – Supraclavicular • Measurement of chest expansion Assessment of chest expansion • Anterior Thoracic Movement: • Posterior Thoracic Movement: Tactile Fremitus Location: Assessing Fremitus: Percussion Percussion Areas: Anterior & Lateral Posterior Methods of Percussion Auscultation Vesicular Inspiratory sounds lasts longer than expiratory sounds Soft Over most of lungs Bronchovesicul ar Inspiration and expiration sounds are equal. Intermediate Angle of louis/between scapulae. Bronchial Expiratory sounds last longer than expiratory ones. Loud Over manubrium sternum. Tracheal Inspiratory and expiratory are about equal Very loud Over trachea in neck. Listen with intent for Breath sounds to the bases Equal breath sounds Inspiration Expiration Abnormal breath sounds Absent or diminished breath sounds Displaced bronchial breath sounds Adventitious breath sounds Crackles Most common cause air passing through fluid (other?) Fine = Smaller airways Coarse = Larger airways Predominantly heard on inspiration Can be equal both lungs Can be isolated to one area Wheezes Produced by air forcing its way through narrowed airways (bronchoconstricted) High pitched musical sounds heard on expiration Can be heard on inspiration Smooth Muscles Irritation = Bronchoconstriction Stridor High pitched continuous crowing sound that is heard over the trachea and larynx Stethoscope not normally needed Best heard over neck Partial airway obstruction from: foreign objects, swelling Pleural Rub Constant grating sound that is heard on inspiration and expiration Caused from parietal and visceral pleura rubbing together Pleura inflamed (loss of serous fluid) Usually localized Proper Auscultation Procedure Attempt to place patient in sitting position Attempt to minimize as much outside noise as possible Encourage patient not to make any moaning and groaning noises Where should I listen? Anterior Chest Posterior Chest