Inhaled Foreign Body
Inhaled Foreign Body
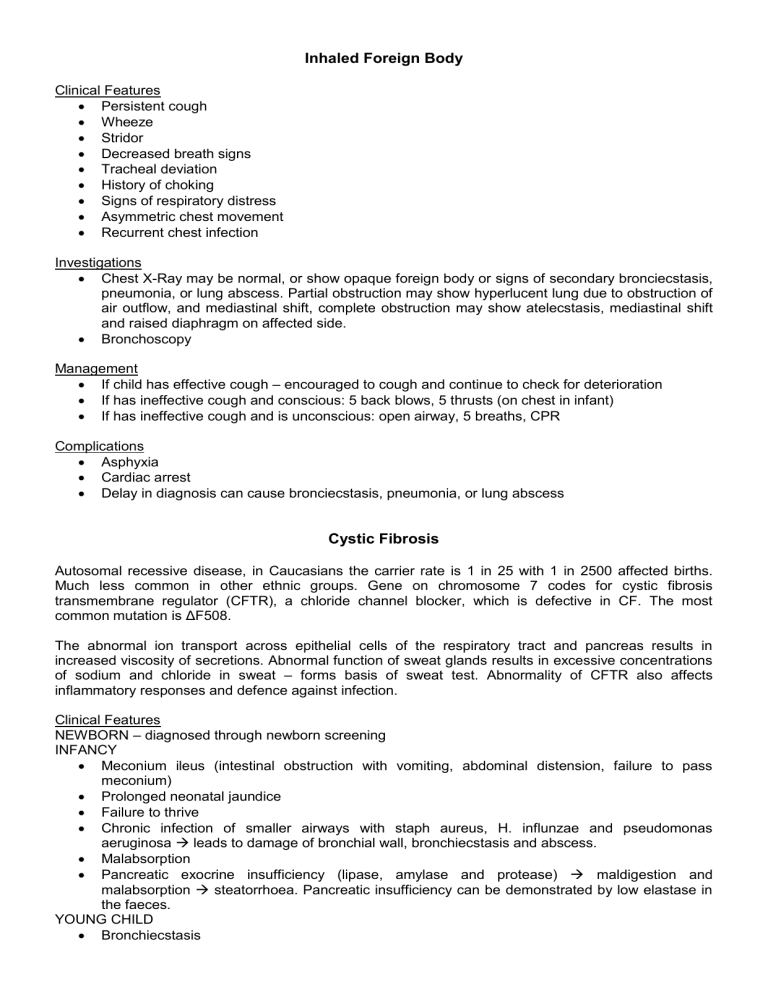
Clinical Features
Persistent cough
Wheeze
Stridor
Decreased breath signs
Tracheal deviation
History of choking
Signs of respiratory distress
Asymmetric chest movement
Recurrent chest infection
Investigations
Chest X-Ray may be normal, or show opaque foreign body or signs of secondary bronciecstasis, pneumonia, or lung abscess. Partial obstruction may show hyperlucent lung due to obstruction of air outflow, and mediastinal shift, complete obstruction may show atelecstasis, mediastinal shift and raised diaphragm on affected side.
Bronchoscopy
Management
If child has effective cough – encouraged to cough and continue to check for deterioration
If has ineffective cough and conscious: 5 back blows, 5 thrusts (on chest in infant)
If has ineffective cough and is unconscious: open airway, 5 breaths, CPR
Complications
Asphyxia
Cardiac arrest
Delay in diagnosis can cause bronciecstasis, pneumonia, or lung abscess
Cystic Fibrosis
Autosomal recessive disease, in Caucasians the carrier rate is 1 in 25 with 1 in 2500 affected births.
Much less common in other ethnic groups. Gene on chromosome 7 codes for cystic fibrosis transmembrane regulator (CFTR), a chloride channel blocker, which is defective in CF. The most common mutation is ΔF508.
The abnormal ion transport across epithelial cells of the respiratory tract and pancreas results in increased viscosity of secretions. Abnormal function of sweat glands results in excessive concentrations of sodium and chloride in sweat – forms basis of sweat test. Abnormality of CFTR also affects inflammatory responses and defence against infection.
Clinical Features
NEWBORN – diagnosed through newborn screening
INFANCY
Meconium ileus (intestinal obstruction with vomiting, abdominal distension, failure to pass meconium)
Prolonged neonatal jaundice
Failure to thrive
Chronic infection of smaller airways with staph aureus, H. influnzae and pseudomonas aeruginosa leads to damage of bronchial wall, bronchiecstasis and abscess.
Malabsorption
Pancreatic exocrine insufficiency (lipase, amylase and protease) maldigestion and malabsorption steatorrhoea. Pancreatic insufficiency can be demonstrated by low elastase in the faeces.
YOUNG CHILD
Bronchiecstasis
Rectal Prolapse
Nasal Polyp
Sinusitis
OLDER CHILD AND ADOLESCENT
Allergic bronchopulmonary aspergillosis (ABPA)
Diabetes mellitus (often Type 2)
Cirrhosis and portal hypertension
Distal intestinal obstruction
Pneumothorax or recurrent haemoptysis
Sterility in males
Increasing psychological problems
Persistent loose cough with over-production of sputum
Hyperinflation of the chest due to air trapping.
Coarse inspiratory crepitations or expiratory wheeze.
Finger clubbing in established disease
Investigations
Chest X-Ray – hyperinflation, marked peribronchial shadowing, bronchial wall thickening and ring shadows.
Management
Annual review in specialist centre
Therapy aims to prevent progression of lung disease and to maintain adequate nutrition and growth
RESPIRATORY MANAGEMENT
Young children respiratory status monitored on symptoms, older children have lung function measured regularly by spirometry
With regular treatment should have no respiratory signs
Physiotherapy twice a day – clear airways of secretions (chest percussion, postural drainage, controlled deep breathing)
Physical exercise encouraged
Continuous prophylactic oral antibiotics, plus additional rescue antibiotics for n increase in respiratory symptoms or decline in lung function
Persistent symptoms require prompt IV antibiotics, usually for 14days
Chronic pseudomonas infection is associated with more rapid decline – slowed by daily nebulised antipseudomonal antibiotics
Nebulised DNase can decrease viscosity of sputum