symptoms - UNC School of Medicine
advertisement

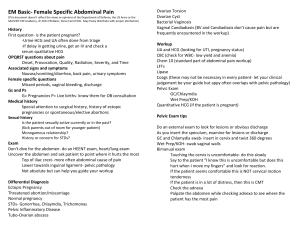
Infections in OB/GYN: Vaginitis, STI’s UNC School of Medicine Obstetrics and Gynecology Clerkship Case Based Seminar Series Lisa Rahangdale, MD, MPH Dept. of OB/GYN Objectives for Vaginitis Formulate a differential diagnosis for vulvovaginitis Interpret a wet mount microscopic examination Describe the variety of dermatologic disorders of the vulva Discuss the steps in the evaluation and management of a patient with vulvovaginal symptoms Objectives for STI’s Describe the guidelines for STI screening and partner notification and treatment Describe STI prevention strategies, including immunization Describe the symptoms and physical exam findings associated with common STI’s Discuss the steps in the evaluation and initial management of common STI’s including appropriate referral Describe the pathophysiology of salpingitis and pelvic inflammatory disease Describe the evaluation, diagnostic criteria and initial management of salpingitis/pelvic inflammatory disease Identify the possible long-term sequelae of salpingitis/pelvic inflammatory disease Case: 2 wkhxh/o vaginal 2626yoyo w/ 2 wk vag DC DC • • • • • • • Differential Diagnosis HPI Pertinent PMH Pelvic Exam MicroscopyLaboratory Treatment Counseling Vaginal Discharge: Ddx Candidiasis Bacterial Vaginosis Trichomonas Atrophic Physiologic (Leukorrhea) Mucopurulent Cervicitis Uncommon Foreign Body HPI Age Characteristics of discharge color, odor, consistency Symptoms Itching, burning erythema, bumps Bleeding, pain Prior occurences, treatments Risk factors Sexual activity, medications, PMH (pregnancy, menopause, immunosuppression) Vaginitis/Vaginosis Characteristics of the discharge pH Amine odor Wet mount Cultures? Vaginal Candidiasis Part of normal flora Majority Candida albicans Predisposing factors: Diabetes Antibiotics Increased estrogen levels (preg, OCP, HRT) Immunosuppression ?Contraceptive devices, behaviors Vaginal Candidiasis S/Sx Pruritis White, clumpy discharge pH 4-4.5 Dxs: KOH prep Treatment Fluconazole 150 mg PO x1 Topical azoles (OTC) Pelvic exam Bacterial Vaginosis Disruption of healthy vaginal flora Gardnerella, mycoplasmas, anaerobic overgrowth Dxs criteria: Gram stain OR 3 out of 4 Homogenous, thin, white d/c “CLUE CELLS” Whiff test: “amine odor” when d/c mixed w/ KOH pH >4.5 Bacterial Vaginosis Bacterial Vaginosis: Treatment Metronidazole 500 mg BID x 7 days OR Metronidazole gel, 0.75%, one full applicator (5g) PV QD x 5 days OR Clindamycin cream, 2%, one full applicator (5g) PV QHS x 7 days **Avoid alcohol during metronidazole use** Trichomonas Flagellate parasite “Strawberry”Cervix Pruritis, frothy green discharge Vaginal pH >4, neg KOH whiff test NaCl Microscopy: +WBCs, Trichomonads Rx: Metronidazole 2 gm po X 1 Tinidazole 2 gm PO x 1 Partner tx Same doses in pregnancy Pelvic Exam Sexually Transmitted Diseases (STI’s) Causative Agent Method of Transmission Symptoms Physical Signs Diagnostic Methods Treatment Screening Prevention: don’t forget the obvious! Counsel your patients about condom use! Neisseria gonorrhea: Symptoms A single encounter with an infected partner 80-90% transmission rate Arise 3-5 days after exposure Initially so mild as to be overlooked Malodorous, purulent vaginal discharge 15% develop acute PID Neisseria gonorrhea: Diagnosis Physical Exam: Mucopurulent discharge flowing from cervix To be distinguished from normal thick yellow white cervical mucous (adherent to ectropion) Cervical Motion Tenderness Neisseria gonorrhea: Diagnosis Elisa or DNA specific test Cervical swab Combined with Chlamydia Urine tests Culture for legal purposes Gram Stain for WBCs with intracellular gram negative diplococci Neisseria gonorrhea: Disseminated Gonococcal bacteremia (rare) Pustular or petechial skin lesions Asymetrical arthralgia Tenosynovitis Septic arthritis Rarely Endocarditis Meningitis Neisseria gonorrhea: Treatment Ceftriaxone 125 mg IM in a single dose OR Cefixime 400 mg orally in a single dose PLUS Tx FOR CHLAMYDIA IF NOT RULED OUT Do NOT use Quinolones in U.S. - resistant GC common Chlamydia trachomatis C. trachomatis Obligate intracellular pathogen No cell wall, not susceptible to penicillins Difficult to culture Chlamydia trachomatis: Diagnosis Usually asymptomatic Best to screen susceptible young women Mucopurulent cervicitis Intermenstrual bleeding Friable cervix Postcoital bleeding Elisa or DNA probe Chlamydia trachomatis: Treatment Uncomplicated cervicitis (no PID) Azithromycin 1 gm po OR Doxycycline 100 mg BID for 7 days Repeat testing in 3 mons Annual screen in age < 25 Chlamydia trachomatis: Pregnancy Azithromycin 1 g orally in a single dose OR Amoxicillin 500 mg orally three times a day for 7 days Test of cure in 3 weeks Case: 2621yoyo presents 2 wk hxwith vagRLQ DCpain • Differential Diagnosis: – – – – – GYN OB GI Urologic MSK Pelvic Inflammatory Disease Pelvic Inflammatory Disease Polymicrobial Initiated by GC, Chlamydia, Mycoplasmas Overgrowth by anaerobic bacteria, GNRs and other vaginal flora (Strep, Peptostrep) Bacterial Vaginosis - associated with PID PID: Symptoms Acute or chronic abdominal/pelvic pain Deep Dyspareunia Fever and Chills Nausea and Vomiting Epigastric or RUQ pain (perihepatitis) PID: Physical Diagnosis Minimum criteria: one or more of the following Uterine Tenderness Cervical Motion Tenderness Adnexal Tenderness Additional support: Fever > 101/38.4 Mucopurulent Discharge Abdominal tenderness +/- rebound Adnexal fullness or mass Hydrosalpinx or TOA PID: Diagnostic Tests WBC may be elevated, often WNL ESR >40, Elevated CRP-neither reliable Ultrasound Hydrosalpinx or a TuboOvarian Complex due to Adhesions are to be distinguished from TuboOvarian Abcess Fluid in Culdesac nonspecific Fluid in Morrison’s Pouch is suggestive if associated with epigastric/RUQ pain PID: Outpatient Treatment http://www.cdc.gov/std/treatment/2010/pid.htm#a2 Outpatient Ceftriaxone 250mg IM + Doxycycline x 14 d w/ or without Metronidazole x 14 d Cefoxitin 2 g IM + Probenecid 1 g PM concurrently + Doxy x 14 d w/ or without Metronidazole x 14 d Other parenteral 3rd generation cephalosporin + Doxy x 14 d w/ or with Metronidazole x 14 d PID: Inpatient Treatment Criteria (2010 CDC STD guidelines) Surgical emergencies not excluded (appy) Unable to tolerate/comply with oral Rx Failed outpatient tx (no improvement 72 hrs) Severe illness, Nausea, Vomiting, High Fever TuboOvarian Abcess (refer for surgical evaluation if patient not improving) Pregnancy *no evidence that adolescents require hospitalization Consider referral to GYN if patient not improving PID: Inpatient Treatment http://www.cdc.gov/std/treatment/2010/pid.htm#a2 A: Cefoxitin 2 gm IV q 6 hr OR Cefotetan 2 gm q 12 hr Plus Doxycycline 100mg IV or po q 12 hr B: Clindamycin 900mg q 8 hr and Gentamycin 2 mg/kg then 1.5mg/kg q 8 hr * Can d/c IV therapy 24 hrs after clinical improvement, complete 14 days PID: Sequelae Pelvic Adhesions chronic pelvic pain, dyspareunia infertility ectopic pregnancy Empiric Treatment Suspected Chlamydia, GC or PID Deemed valuable in preventing sequelae Recommended Screening GC/Chlamydia: women < 25 (**remember urine testing!) Pregnancy Syphilis Pregnancy HIV age 13-64, (? Screening time interval) One STD, consider screening for others PE, Wet mounts, PAP, GC/CT, VDRL, HIV Case: w/hx lesion vulva 26 24 yoyo 2G0wk vagonDC • • • • • • • Differential Diagnosis HPI Pertinent ROS Focused exam Laboratory Treatment Counseling Genital Ulcers Syphilis Herpes Chanchroid Lymphogranuloma Venereum Granuloma Inguinale Herpes Herpes Simplex Virus I and II Spread by direct contact “mucous membrane to mucous membrane” Painful ulcers Irregular border on erythematous base Exquisitely tender to Qtip exam Culture, PCR low sensitivity after Day 2 Herpes Primary Systemic symptoms Multiple lesions Urinary retention Nonprimary First Episode Few lesions No systemic symptoms preexisting Ab Herpes: Treatment First Episode Acyclovir, famciclovir, valcyclovir x 7–10 days Recurrent Episodic Rx: In prodrome or w/in 1 day of lesion) 1-5 day regimens Suppressive therapy Important for last 4 weeks of pregnancy Syphilis Treponema Pallidum- spirochete Direct contact with chancre: cervix, vagina, vulva, any mucous membrane Painless ulceration Reddish brown surface, depressed center Raised indurated edges Dx: smear for DFA, Serologic Testing Syphilis Stages Clinically Manifest vs. Latent Primary- painless ulcer chancre must be present for at least 7 days for VDRL to be positive Secondary Rash (diffuse asymptomatic maculopapular) lymphadenopathy, low grade fever, HA, malaise, 30% have mucocutaneous lesions Tertiary gummas develop in CNS, aorta Primary and Secondary Syphilis Latent Syphilis Definition: Asx, found on screen Early 1 year duration Late >1 year or unknown duration Testing Screening: VDRL, RPR- nontreponemal Confirmatory: FTA, MHATP- treponemal Syphilis: Treatment Primary, Secondary and Early Latent Benzathine Penicillin 2.4 mU IM Tertiary, Late Latent Benzathine Penicillin 2.4 mU IM q week X 3 Organisms are dividing more slowly later on NeuroSyphilis IV Pen G for 10-14 days Chancroid Endemic to some areas of US, outbreaks Hemophilus Ducreyi Painful ulcers, tender LNs Can aspirate a suppurative LN for Dx Coexists with HIV, HSV, Syphilis Culture is < 80% sensitive, PCR ? Rx: Azithro, Rocephin, Cipro Lymphogranuloma Venerum Chlamydia trachomatis Different serovars Rare in US Brief ulcer, inflammation of perirectal lymphatic tissues, strictures, fistulas Lymph nodes may require drainage Dx: Serologic Testing CT serovars L1-3 Rx: Doxycycline, Erythromycin Granuloma Inguinale Outside US, Tropics Calymmatobacterium granulomatis Highly Vascular, Painless progressive ulcers without LAD Dx: Histologic ID of Donovan bodies Coexists with other STDs or get secondarily infected with genital flora Rx: Septra, Doxycycline, Cipro, Erythro Vulvar Lesions Human Papilloma Virus Molluscum Contagiosum Pediculosis Pubis Scabies HPV: Genital Warts Most common STD HPV 6 and 11 – low risk types Verruccous, pink/skin colored, papillaform DDxs: condyloma lata, squamous cell ca, other Treatment: Chemical/physical destruction (cryo, podophyllin, 5% podofilox, TCA) Immune modulation (imiquimod) Excision Laser Other: 5-FU, interferon-alpha, sinecatchins High rate of RECURRENCE Gardasil covers HPV 6, 11 Bottom Line Concepts Appropriate diagnosis of vaginitis will ensure appropriate treatment. The various forms of vulvovaginitis are easily confused by patients. Be familiar with appropriate STI screening guidelines and review them at all preventive care visits. The CDC provides excellent information on treatment of STI’s. The only truly effective preventive measures is abstinence from sexual activity. Condoms and dental dams are the only preventive measure we have for patients who are sexually active. References and Resources APGO Medical Student Educational Objectives, 9th edition, (2009), Educational Topic 35, 36 (p74-77). Beckman & Ling: Obstetrics and Gynecology, 6th edition, (2010), Charles RB Beckmann, Frank W Ling, Barabara M Barzansky, William NP Herbert, Douglas W Laube, Roger P Smith. Chapter 26, 27 (p241258). Hacker & Moore: Hacker and Moore's Essentials of Obstetrics and Gynecology, 5th edition (2009), Neville F Hacker, Joseph C Gambone, Calvin J Hobel. Chapter 22 (p265-275). CDC 2010 STD Treatment guidelines: http://www.cdc.gov/std/treatment/2010/toc.htm