Introduction
Aetiology and Epidemiology:
•
Pelvic Inflammatory Disease
•
•
•
•
•
•
Pelvic Inflammatory Disease (PID) is the term used to describe upper genital
tract infection in women
Infection may involve the endometrium with or without involvement of the
fallopian tubes and peritoneal space
PID is usually initiated by a sexually transmitted organism.
The organisms most commonly implicated are Neisseria gonorrhoeae and
Chlamydia trachomatis.
Regardless of the initiating event, the microbiology of PID usually includes
a mixture of bacteria from vaginal flora e.g. anaerobes, streptococci,
Haemophilus and enteric gram-negative bacteria.
True incidence unknown.
Pelvic infections may also occur after IUCD insertion, TOP, spontaneous
abortion, instrumentation of upper genital tract, during pregnancy or postpartum.
Symptoms and signs:
• Estimated up to 60% are sub-clinical - no or minimal symptoms
• Pelvic pain, deep dyspareunia, abnormal vaginal bleeding, fever
• On examination may have cervical motion tenderness, uterine and adnexal
tenderness, cervicitis, fever
Complications:
• Perihepatitis (Fitz-Hugh-Curtis syndrome) occurs in ~10-20%
• Tubo-ovarian abscess
• Chronic pelvic pain
• Ectopic pregnancy and tubal factor infertility
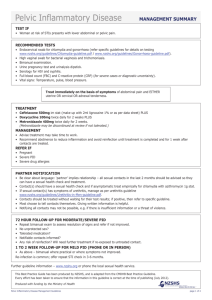
Tests
•
•
Pelvic examination
Sexual health screen, including testing for Neisseria gonorrhoeae, Chlamydia
trachomatis, high vaginal swab for yeasts, bacterial vaginosis and
Trichomonas vaginalis. Screening for HIV, syphilis and HBV infection and
immunity.
CMDHB Primary Care Sexual Health Workstream February 2007
•
•
Urine pregnancy test
Consider urine dipstick, FBC, ESR and CRP
Diagnosis
•
•
Pelvic Inflammatory Disease
No single laboratory test is diagnostic of PID
Diagnosis is clinical, taking into account the history, clinical findings and
results of sexual health screen and supplementary tests
A low threshold for treatment is appropriate in view of important sequelae and
unreliability of diagnostic features
•
Minimum criteria are:
• Pelvic pain AND
• Bilateral adnexal tenderness OR uterine tenderness OR cervical motion
tenderness
Additional suggestive features:
• Abnormal cervical or vaginal mucopurulent discharge
• Fever >38ºC
• Elevated ESR, FBC or CRP
• Confirmed infection with Neisseria gonorrhoeae or Chlamydia trachomatis
Differential diagnosis
The main differential diagnoses to consider are:
• Appendicitis
• Pregnancy complications e.g. ectopic, spontaneous abortion
• Torsion of an ovarian cyst
• UTI
Management
•
•
•
Treatment should cover infection with Neisseria gonorrhoeae, Chlamydia
trachomatis and anaerobes (particularly in moderate to severe infection)
Patients with severe infection requiring hospitalisation should be referred to
Gynaecology for initial inpatient management.
Assessment by the local O&G service is also recommended if the patient is
pregnant.
Outpatient regimens for PID
of mild to moderate severity:
Preferred:
•
•
Ceftriaxone 500mg im stat. AND
Doxycycline 100mg bd po 14 days
•
+Metronidazole 400mg bd for 14 days IF moderately severe PID and extra
anaerobic cover required
Alternative regimen e.g. for patients with a history of penicillin or cephalosporin
anaphylaxis:
CMDHB Primary Care Sexual Health Workstream February 2007
•
Substitute the stat dose of ceftriaxone for Ciprofloxacin 500mg po stat.
Pelvic Inflammatory Disease
IUCD Users:
• There is recent evidence suggesting that treatment of PID is not hindered by
the presence of an IUCD
• The decision as to whether or not an IUCD should be left in situ should be
made on a case by case basis in consultation with the patient
• If the IUCD is removed, recommend delaying this until approx 24 hours into
antibiotic therapy and consider ECP
• If there is inadequate clinical response within 24-48 hours, removal of the IUCD
should be considered
Pregnancy:
• PID in pregnancy is very uncommon, especially after the 12th week as the
gestational sac occludes the uterine cavity. However, chorioamnionitis may also
result from haematogenously spread infection
• Pregnant woman who have suspected PID should be assessed by the local
O&G service and treated with parenteral antibiotics
Partner notification and management of sexual
partners
Partner notification:
• Patient should be encouraged to notify all sexual partners from the
preceding 2 months (or most recent partner if over 2 months since last
contact) and advise them to attend for testing and treatment
Management of sexual partners:
• Perform a sexual health screen and treat empirically with a regimen suitable for
Chlamydia.
• If the index case is diagnosed with N. gonorrhoeae and/or Trichomonas
vaginalis infection, treat partner empirically for these also.
• If the sexual partner is positive for Chlamydia trachomatis or Neisseria
gonorrhoeae – further partner notification as above
Follow-up
•
•
•
In mild infection patients should be reviewed in 1 week and pelvic
examination repeated to confirm resolution of signs
In moderate infection patients should be reviewed in 48 hrs and if not
improving consider Gynaecology referral.
Repeat a sexual health screen approx 3 months after treatment.
Referral guidelines
Referral to a Specialist Sexual Health Service is recommended for:
• Management of sexual partners if clinician wishes
CMDHB Primary Care Sexual Health Workstream February 2007