Vaginitis And PID
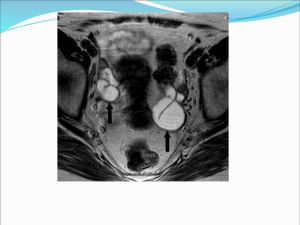
advertisement

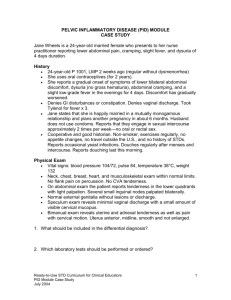
Vaginitis and PID – The Basics Wanda Ronner, M.D. Vaginitis • • • • Disruption in the normal vaginal ecosystem Alteration of vaginal pH A decrease in lactobacilli Growth of other bacteria Normal physiologic discharge • • • • • Cervical mucus Endometrial fluid Fluid from Skene’s and Bartholin’s glands Exfoliated squamous cells Normal pH: 3.5 – 4.5 during reproductive years; 6 – 8 after menopause Common Causes of Vaginitis • Bacterial Vaginosis: 15 - 50% of cases; all ages; anaerobic bacteria and Gardnerella vaginalis • Trichomonas: 15 - 20% of cases; 2045years; protozoan Trichomonas vaginalis • Candida: 33% of cases; premenopausal women: 90% caused by Candida albicans Common Treatments • Yeast: oral fluconazole 150mg single dose, or clotrimazole, miconazole, or terconazole. • Trichomonas: oral metronidazole 2 grams in a single dose or 500mg bid for 7 days. • Bacterial Vaginosis: oral metronidazole 500mg bid for 7 days, or vaginal clindamycin cream or metronidazole gel. Atrophic Vaginitis • 40% of postmenopausal women • Caused by estrogen deficiency • Symptoms: dryness, itching, burning, dyspareunia, pelvic pressure, yellowishgreen malodorous discharge • Findings: pH > 5, decreased superficial cells, WBCs • Treatment: vaginal or oral estrogen 67 yr. old with vulvar/vaginal atrophy Pelvic Inflammatory Disease • Inflammatory disorders of the upper female genital tract – endometritis, salpingitis, tubo-ovarian abscess, pelvic peritonitis • Organisms responsible: mainly Gonorrhea and Chlamydia; anaerobes, G. vaginalis, Haemophilus, enteric Gram-negative rods, Streptococcus agalactiae. PID – a public health concern • Most common gyn reason for ER visits: 350,000/year. • 70,000 hospitalizations/year. • Most common serious infection of women age 16 – 25. • One in four women have significant medical or reproductive complications. Diagnosis of PID • • • • • • • • Cervical motion tenderness Uterine tenderness Adnexal tenderness Temp > 101º F Mucopurulent discharge Abundant WBCs on wet mount Elevated ESR, elevated C-reactive protein GC or Chlamydia Differential Diagnosis • • • • • • • Ectopic pregnancy Acute appendicitis Functional pain (e.g. pain with ovulation) Dysmenorrhea Endometriosis UTI/Pyelonephritis Bowel disorders Treatment of PID • Need to provide empiric, broad spectrum coverage of likely pathogens • Must include treatment for GC and Chlamydia • See handout for April 2007 CDC treatment regimens CDC Recommended Regimens • Parenteral: Cefotetan (2g IV every 6 hrs) OR Cefoxitin (2g IV every 6 hrs) PLUS Doxycycline (100 mg orally or or IV) every 12 hrs. • Oral: Ceftriaxone (250mg IM in a single dose) PLUS Doxycycline 100mg orally twice a day for 14 days with or without Metronidazole 500mg orally twice a day for 14 days Why do we treat aggressively? • Even mild cases may result in severe damage: infertility, ectopic pregnancy, and chronic pelvic pain. Follow Up • Improvement should be seen within 3 days on oral meds – defervescence, reduction in abdominal tenderness, uterine, adnexal and cervical motion tenderness – if not – HOSPITALIZE • In no improvement after 3 days on parenteral meds consider laparoscopy