Infections in OB/GYN: Vaginitis, STIs
advertisement

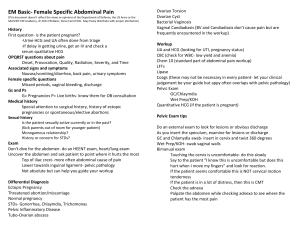
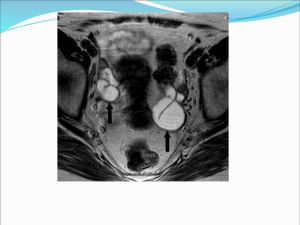
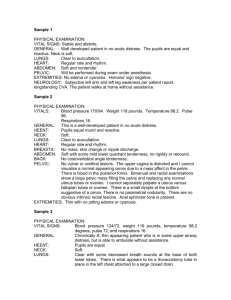
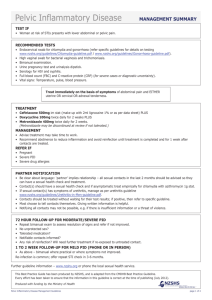
Infections in OB/GYN: Vaginitis, STIs Lisa Rahangdale, MD, MPH Dept. of OB/GYN Objectives • Diagnose and treat a patient with vaginitis • Interpret a wet prep • Differentiate the signs and symptoms, PE findings, diagnostic evaluation of the following STI’s: – – – – – Gonnorhea Chlamydia Herpes Syphillis HPV • Describe pathogenesis, signs and symptoms and management of PID 26 yo 2 wk hx vag DC • • • • • • • Differential Diagnosis HPI Pertinent PMH Pelvic Exam MicroscopyLaboratory Treatment Counseling Vaginal Discharge DDXS • • • • • • • Candidiasis Bacterial Vaginosis Trichomonas Atrophic Physiologic (Leukorrhea) Mucopurulent Cervicitis Uncommon – Foreign Body – Desquamative HPI • Age • Characteristics of discharge – color, odor, consistency • Symptoms – Itching, burning – erythema, bumps – Bleeding, pain • Prior occurences, treatments • Risk factors – Sexual activity, medications, PMH PMH • Pregnancy • Menopause • Immunosuppression – Diabetes, HIV, medications Pelvic exam Microscopy Pelvic Exam Microscopy Treatment & Counseling • Rx: Metronidazole 2 gm po X 1 Tinidazole 2 gm PO x 1 • Counseling – Partner treatment – Safe sex Pelvic exam Microscopy Pelvic exam Neisseria gonnorhea • Symptoms – Arise 3-5 days after exposure – Initially so mild as to be overlooked – Malodorous, purulent vaginal discharge • Physical Exam – Mucopurulent discharge flowing from cervix – Cervical Motion Tenderness Gonorrhea Rx Ceftriaxone 125 mg IM in a single dose OR Cefixime400 mg orally in a single dose PLUS Tx FOR CHLAMYDIA IF NOT RULED OUT Do NOT use Quinolones in U.S. - resistant GC common Chlamydia S/Sx/Dxs • • • • • • Usually asymptomatic Best to screen susceptible young women Mucopurulent cervicitis Intermenstrual bleeding Friable cervix Postcoital bleeding • Elisa or DNA probe (difficult to culture) Chlamydia Rx • Uncomplicated cervicitis (no PID) – Azithromycin 1 gm po OR – Doxycycline 100 mg BID for 7 days • Repeat testing in 3 mons • Annual screen in age < 25 Chlamydia in Pregnancy • Azithromycin 1 g orally in a single dose OR Amoxicillin 500 mg orally three times a day for 7 days (2006 - Poor efficacy of erythromycin – now alternative regimen) • Test of cure in 3 weeks 21 YO presents with RLQ pain • Differential diagnosis – GYN – OB – GI – Urologic – MSK • She has CMT on pelvic examination. Does this rule anything out? HPI • • • • LMP = 5 days ago Pelvic pain, vaginal discharge x 2 days New sexual partner in last 3 months Uses condoms “all of the time except sometimes when we forget.” Pelvic Inflammatory Disease • Polymicrobial – Initiated by GC, Chlamydia, Mycoplasmas – Overgrowth by anaerobic bacteria, GNRs and other vaginal flora (Strep, Peptostrep) – Bacterial Vaginosis - associated with PID PID Symptoms • Acute or chronic abdominal/pelvic pain • Deep Dyspareunia • Fever and Chills • Nausea and Vomiting • Epigastric or RUQ pain (perihepatitis) PID Physical Diagnosis • Minimum criteria: one or more of the following– Uterine Tenderness – Cervical Motion Tenderness – Adnexal Tenderness • Additional support: – – – – Fever > 101/38.4 Mucopurulent Discharge Abdominal tenderness +/- rebound Adnexal fullness or mass • Hydrosalpinx or TOA PID Diagnostic Tests • WBC may be elevated, *often WNL • ESR >40, Elevated CRP-neither reliable • Ultrasound – Hydrosalpinx or a TuboOvarian Complex/Abcess – Fluid in Culdesac nonspecific – Fluid in Morrison’s Pouch is suggestive if associated with epigastric/RUQ pain “Am I going to have to go the hospital?” • Inpatient tx Criteria – – – – – – – Peritoneal signs Surgical emergencies not excluded (appy) Unable to tolerate/comply with oral Rx Failed OP tx Nausea, Vomiting, High Fever TuboOvarian Abcess Pregnancy 2006 CDC STD guidelines PID Treatment • Needs to incorporate Rx of GC and Chlamydia (tests pending) • Outpatient – Ceftriaxone 250mg IM + Doxycycline x 14 d w/ or w/out Metronidazole 500mg bid x 14 d – Levofloxacin 500 mg QD or Ofloxacin 400 mg BID + Metronidazole x14 days (No Quinolone unless allergy) Regimens:http://www.cdc.gov/std/treatment/2006/pi d.htm PID Inpatient Rx • Cefoxitin 2 gm IV q 6 hr • OR Cefotetan 2 gm q 12 hr – Plus • Doxycycline 100mg IV or po q 12 hr • For maximal anaerobic coverage/penetration of TOA: – Clindamycin 900mg q 8 hr and – Gentamycin 2 mg/kg then 1.5mg/kg q 8 hr “Am I going to be OK after I take these antibiotics?” PID SEQUELAE • Pelvic Adhesions – chronic pelvic pain, dyspareunia – infertility – ectopic pregnancy • Empiric Treatment – Suspected Chlamydia, GC or PID – Deemed valuable in preventing sequelae Recommended Screening • GC/Chlamydia: – women < 25 (**remember urine testing!) – Pregnancy • Syphilis – Pregnancy • HIV – age 13-64, (? Screening time interval) • One STD, consider screening for others – PE, Wet mounts, PAP, GC/CT, VDRL, HIV 24 yo G 0 lesion on vulva • • • • • • HPI Pertinent review of systems Focused exam Laboratory Treatment Counseling re partner Vulvar lesions: DDxs • Genital Ulcers – – – – Herpes Syphilis Chanchroid Lymphogranuloma Venereum – Granuloma Inguinale • Vulvar lesions – HPV – Molluscum Contagiosum – Pediculosis Pubis – Scabies Herpes • Herpes Simplex Virus I and II • Spread by direct contact – “mucous membrane to mucous membrane” • • • • Painful ulcers Irregular border on erythematous base Exquisitely tender to Qtip exam Culture, PCR low sensitivity after Day 2 Herpes • Primary – Systemic symptoms – Multiple lesions – Urinary retention • Nonprimary First Episode – Few lesions – No systemic symptoms – preexisting Ab Herpes Rx • First Episode – Acyclovir, famciclovir, valcyclovir x 7–10 days • Recurrent Episodic Rx: – In prodrome or w/in 1 day of lesion) – 1-5 day regimens • Suppressive therapy – Important for last 4 weeks of pregnancy Syphilis • Treponema Pallidum- spirochete • Direct contact with chancre: cervix, vagina, vulva, any mucous membrane • Painless ulceration • Reddish brown surface, depressed center • Raised indurated edges • Dx: smear for DFA, Serologic Testing Syphilis Stages • Clinically Manifest vs. Latent • Primary- painless ulcer – chancre must be present for at least 7 days for VDRL to be positive • Secondary– Rash (diffuse asymptomatic maculopapular) lymphadenopathy, low grade fever, HA, malaise, 30% have mucocutaneous lesions • Tertiary gummas develop in CNS, aorta Primary & Secondary Syph Latent Syphilis • Definition: Asx, found on screen – Early 1 year duration – Late >1 year or unknown duration • Testing – Screening: VDRL, RPR- nontreponemal – Confirmatory: FTA, MHATP- treponemal Syphilis Treatment • Primary, Secondary and Early Latent – Benzathine Penicillin 2.4 mU IM • Tertiary, Late Latent • Benzathine Penicillin 2.4 mU IM q week X 3 • Organisms are dividing more slowly later on • NeuroSyphilis • IV Pen G for 10-14 days Vulvar Lesions • • • • Human Papilloma Virus Molluscum Contagiosum Pediculosis Pubis Scabies HPV – genital warts • • • • • Most common STD HPV 6 and 11 – low risk types Verruccous, pink/skin colored, papillaform DDxs: condyloma lata, squamous cell ca, other Treatment: – – – – – Chemical/physical destruction (cryo, podophyllin, 5% podofilox, TCA) Immune modulation (imiquimod) Excision Laser Other: 5-FU, interferon-alpha, sinecatchins • High rate of RECURRENCE