Gonorrhea
advertisement

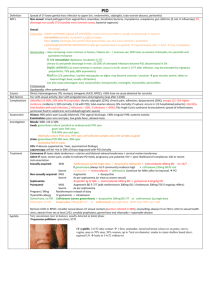
Infections in OB/GYN: Vaginitis, STIs Lisa Rahangdale, MD, MPH Dept. of OB/GYN Objectives Diagnose and treat a patient with vaginitis Interpret a wet prep Differentiate the signs and symptoms, PE findings, diagnostic evaluation of the following STI’s: Gonnorhea Chlamydia Herpes Syphillis HPV Describe pathogenesis, signs and symptoms and management of PID Vaginal Discharge DDXS Candidiasis Bacterial Vaginosis Trichomonas Atrophic Physiologic (Leukorrhea) Mucopurulent Cervicitis Uncommon Foreign Body Desquamative Vaginitis/Vaginosis Characteristics of the discharge pH Amine odor Wet mount Cultures? Vaginal Candidiasis Part of normal flora Majority Candida albicans Predisposing factors: Diabetes Antibiotics Increased estrogen levels (preg, OCP, HRT) Immunosuppression ?Contraceptive devices, behaviors Vaginal Candidiasis S/Sx Pruritis White, clumpy discharge pH 4-4.5 Dxs: KOH prep Treatment Fluconazole 150 mg PO x1 Topical azoles (OTC) Bacterial Vaginosis Disruption of healthy vaginal flora Gardnerella, mycoplasmas, anaerobic overgrowth Dxs criteria: Gram stain OR 3 out of 4 Homogenous, thin, white d/c “CLUE CELLS” Whiff test: “amine odor” when d/c mixed w/ KOH pH >4.5 Bacterial Vaginosis BV Treatment Metronidazole 500 mg BID x 7 days OR Metronidazole gel, 0.75%, one full applicator (5g) PV QD x 5 days OR Clindamycin cream, 2%, one full applicator (5g) PV QHS x 7 days **Avoid alcohol during metronidazole use** Trichomonas Flagellate parasite “Strawberry”Cervix pruritis, frothy green discharge Vag pH >4, neg KOH whiff test NaCl Microscopy: +WBCs, Trichomonads Rx: Metronidazole 2 gm po X 1 Tinidazole 2 gm PO x 1 Partner tx Same doses in pregnancy SEXUALLY TRANSMITTED DISEASES Causative Agent Method of Transmission Symptoms Physical Signs Diagnostic Methods Treatment Screening Neisseria gonnorhea: Symptoms A single encounter with an infected partner 80-90% transmission rate Arise 3-5 days after exposure Initially so mild as to be overlooked Malodorous, purulent vaginal discharge 15% develop acute PID Physical Diagnosis Mucopurulent discharge flowing from cervix To be distinguished from normal thick yellow white cervical mucous(adherent to ectropion) Cervical Motion Tenderness Gonorrhea: DXS Elisa or DNA specific test Cervical swab Combined with Chlamydia Urine tests Culture for legal purposes Gram Stain for WBCs with intracellular gram negative diplococci Physical Diagnosis Mucopurulent discharge flowing from cervix To be distinguished from normal thick yellow white cervical mucous(adherent to ectropion) Cervical Motion Tenderness Disseminated GC Gonococcal bacteremia (rare) Pustular or petechial skin lesions Asymetrical arthralgia Tenosynovitis Septic arthritis Rarely Endocarditis Meningitis Gonorrhea Rx Ceftriaxone 125 mg IM in a single dose OR Cefixime400 mg orally in a single dose PLUS Tx FOR CHLAMYDIA IF NOT RULED OUT Do NOT use Quinolones in U.S. - resistant GC common Chlamydia trachomatis C. trachomatis Obligate intracellular pathogen No cell wall, not susceptible to penicillins Difficult to culture Chlamydia Diagnosis Usually asymptomatic Best to screen susceptible young women Mucopurulent cervicitis Intermenstrual bleeding Friable cervix Postcoital bleeding Elisa or DNA probe Chlamydia Rx Uncomplicated cervicitis (no PID) Azithromycin 1 gm po OR Doxycycline 100 mg BID for 7 days Repeat testing in 3 mons Annual screen in age < 25 Chlamydia in Pregnancy Azithromycin 1 g orally in a single dose OR Amoxicillin 500 mg orally three times a day for 7 days (2006 - Poor efficacy of erythromycin – now alternative regimen) Test of cure in 3 weeks Pelvic Inflammatory Disease Polymicrobial Initiated by GC, Chlamydia, Mycoplasmas Overgrowth by anaerobic bacteria, GNRs and other vaginal flora (Strep, Peptostrep) Bacterial Vaginosis - associated with PID PID Symptoms Acute or chronic abdominal/pelvic pain Deep Dyspareunia Fever and Chills Nausea and Vomiting Epigastric or RUQ pain (perihepatitis) PID Physical Diagnosis Minimum criteria: one or more of the following Uterine Tenderness Cervical Motion Tenderness Adnexal Tenderness Additional support: Fever > 101/38.4 Mucopurulent Discharge Abdominal tenderness +/- rebound Adnexal fullness or mass Hydrosalpinx or TOA PID Diagnostic Tests WBC may be elevated, *often WNL ESR >40, Elevated CRP-neither reliable Ultrasound Hydrosalpinx or a TuboOvarian Complex due to Adhesions are to be distinguished from TuboOvarian Abcess Fluid in Culdesac nonspecific Fluid in Morrison’s Pouch is suggestive if associated with epigastric/RUQ pain PID Treatment Needs to incorporate Rx of GC and Chlamydia (tests pending) Outpatient Ceftriaxone 250mg IM + Doxycycline x 14 d w/ or w/out Metronidazole 500mg bid x 14 d Levofloxacin 500 mg QD or Ofloxacin 400 mg BID + Metronidazole x14 days (No Quinolone unless allergy) Regimens:http://www.cdc.gov/std/treatment/ 2006/pid.htm PID Inpatient Rx Criteria (2006 CDC STD guidelines) Peritoneal signs Surgical emergencies not excluded (appy) Unable to tolerate/comply with oral Rx Failed OP tx Nausea, Vomiting, High Fever TuboOvarian Abcess Pregnancy PID Inpatient Rx Cefoxitin 2 gm IV q 6 hr OR Cefotetan 2 gm q 12 hr Plus Doxycycline 100mg IV or po q 12 hr For maximal anaerobic coverage/penetration of TOA: Clindamycin 900mg q 8 hr and Gentamycin 2 mg/kg then 1.5mg/kg q 8 hr PID Sequelae Pelvic Adhesions chronic pelvic pain, dyspareunia infertility ectopic pregnancy Empiric Treatment Suspected Chlamydia, GC or PID Deemed valuable in preventing sequelae Recommended Screening GC/Chlamydia: women < 25 (**remember urine testing!) Pregnancy Syphilis Pregnancy HIV age 13-64, (? Screening time interval) One STD, consider screening for others PE, Wet mounts, PAP, GC/CT, VDRL, HIV 24 yo G 0 lesion on vulva HPI Pertinent review of systems Focused exam Laboratory Treatment Counseling re partner Genital Ulcers Syphilis Herpes Chanchroid Lymphogranuloma Venereum Granuloma Inguinale Herpes Herpes Simplex Virus I and II Spread by direct contact “mucous membrane to mucous membrane” Painful ulcers Irregular border on erythematous base Exquisitely tender to Qtip exam Culture, PCR low sensitivity after Day 2 Herpes Primary Systemic symptoms Multiple lesions Urinary retention Nonprimary First Episode Few lesions No systemic symptoms preexisting Ab Herpes Rx First Episode Acyclovir, famciclovir, valcyclovir x 7–10 days Recurrent Episodic Rx: In prodrome or w/in 1 day of lesion) 1-5 day regimens Suppressive therapy Important for last 4 weeks of pregnancy Syphilis Treponema Pallidum- spirochete Direct contact with chancre: cervix, vagina, vulva, any mucous membrane Painless ulceration Reddish brown surface, depressed center Raised indurated edges Dx: smear for DFA, Serologic Testing Syphilis Stages Clinically Manifest vs. Latent Primary- painless ulcer chancre must be present for at least 7 days for VDRL to be positive Secondary Rash (diffuse asymptomatic maculopapular) lymphadenopathy, low grade fever, HA, malaise, 30% have mucocutaneous lesions Tertiary gummas develop in CNS, aorta Primary & Secondary Syph Latent Syphilis Definition: Asx, found on screen Early 1 year duration Late >1 year or unknown duration Testing Screening: VDRL, RPR- nontreponemal Confirmatory: FTA, MHATP- treponemal Syphilis Treatment Primary, Secondary and Early Latent Benzathine Penicillin 2.4 mU IM Tertiary, Late Latent Benzathine Penicillin 2.4 mU IM q week X 3 Organisms are dividing more slowly later on NeuroSyphilis IV Pen G for 10-14 days Chancroid Endemic to some areas of US, outbreaks Hemophilus Ducreyi Painful ulcers, tender LNs Can aspirate a suppurative LN for Dx Coexists with HIV, HSV, Syphilis Culture is < 80% sensitive, PCR ? Rx: Azithro, Rocephin, Cipro Lymphogranuloma Venereum Chlamydia trachomatis Different serovars Rare in US Brief ulcer, inflammation of perirectal lymphatic tissues, strictures, fistulas Lymph nodes may require drainage Dx: Serologic Testing CT serovars L1-3 Rx: Doxycycline, Erythromycin Granuloma Inguinale Outside US, Tropics Calymmatobacterium granulomatis Highly Vascular, Painless progressive ulcers without LAD Dx: Histologic ID of Donovan bodies Coexists with other STDs or get secondarily infected with genital flora Rx: Septra, Doxycycline, Cipro, Erythro Vulvar Lesions Human Papilloma Virus Molluscum Contagiosum Pediculosis Pubis Scabies HPV – genital warts Most common STD HPV 6 and 11 – low risk types Verruccous, pink/skin colored, papillaform DDxs: condyloma lata, squamous cell ca, other Treatment: Chemical/physical destruction (cryo, podophyllin, 5% podofilox, TCA) Immune modulation (imiquimod) Excision Laser Other: 5-FU, interferon-alpha, sinecatchins High rate of RECURRENCE