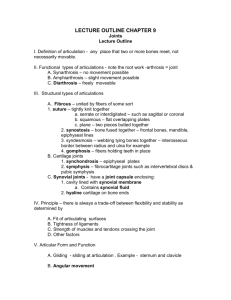
Ch 8. Joints
advertisement

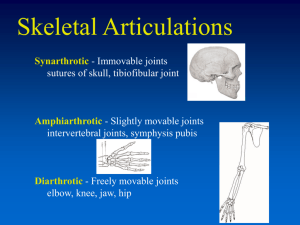
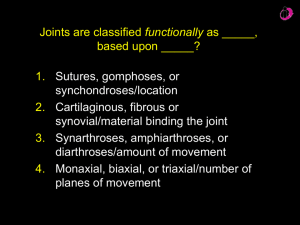
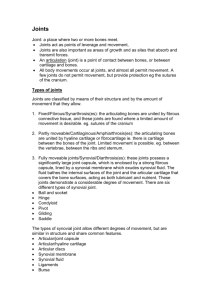
Ch 8. Joints Joints • Or articulations • Sites where two bones meet • 2 fundamental functions 1. Motility 2. Hold skeleton together - Weakest part of skeleton Classification of Joints • Classified by structure and function • Structural – material binding – Fibrous – Cartilaginous – Synovial joints • Function – Amount of movement – Synarthroses – immovable – Amphiarthroses – slightly movable – Diarthroses – freely movable • General – – fibrous = immobile – Synovial – freely movable – Cartilaginous - both Fibrous Joints • • • • • Bones joined by fibrous tissue Dense fibrous connective tissue No joint cavity present Most are immovable 3 types 1. Sutures 2. Syndesmoses 3. gomphoses Fibrous Joints 1. Sutures • “seams” • Only between bones of skull • Rigid slices knit bone together • During middle age – ossifies – closed sutures – synostoses • Immobile = protection (a) Suture Joint held together with very short, interconnecting fibers, and bone edges interlock. Found only in the skull. Suture line Dense fibrous connective tissue Figure 8.1a Fibrous Joints 2. Syndesmoses – • Bones connected by ligaments • Only cords or bands of fibrous tissue • Amount of movement depends on length of connecting fibers (b) Syndesmosis Joint held together by a ligament. Fibrous tissue can vary in length, but is longer than in sutures. Fibula Tibia Ligament Figure 8.1b Fibrous Joints 3. Gomphoses – • Peg in socket fibrous joint • Tooth joint • Teeth embedded in sockets – periodontal ligament (c) Gomphosis “Peg in socket” fibrous joint. Periodontal ligament holds tooth in socket. Socket of alveolar process Root of tooth Periodontal ligament Figure 8.1c Cartilaginous Joints • • • • Unit articulating bones Lack joint cavity Not highly mobile 2 types – 1. Synchondroses 2. Symphyses Cartilaginous Joints 1. Synchondroses – • Bones united by bar or plate of hyaline cartilage • Epiphyseal plates in long bones of children • Costal cartilage of first rib (c) Gomphosis “Peg in socket” fibrous joint. Periodontal ligament holds tooth in socket. Socket of alveolar process Root of tooth Periodontal ligament Figure 8.1c Cartilaginous Joints 2. Symphyses – • “growing together” • Intervening pad or plate of fibrocartilage • Compress able and resilience • Amphiarthrotic joints • Designed for strength and flexibility (b) Symphyses Bones united by fibrocartilage Body of vertebra Fibrocartilaginous intervertebral disc Hyaline cartilage Pubic symphysis Figure 8.2b Synovial Joints • “joint eggs” • Articulating bones are separated by a fluid filled joint cavity • Freedom of movement • Freely moveable diarthroses Synovial Joints General Structure • 6 distinguishing characteristics: 1. Articular Cartilage – glassy smooth hyaline – articular cartilage – Thin, spongy cushions absorb compression 2. Joint (Synovial) Cavity – joint cavity – potential space with a small amount of synovial fluid 3. Articular Capsule – 2 layered articular capsule or joint capsule • Inner synovial membrane – loose CT 4. Synovial Fluid – occupies all free space • Derived by filtration • Viscous, egg white consistency • Slippery weight bearing film – reduces friction Synovial Joints General Structure 5. Reinforcing Ligaments – band like ligaments • Usually – capsular or intrinsic ligaments – thickened parts of fibrous capsule • Outside capsule – distinct – extra- capsular ligaments • Deep to it – intracapsular ligaments 6. Nerves and blood vessels – richly supplied with sensory nerve fibers • Some detect pain • Most monitor joint positions and stretch • Richly supplied with capillary beds – produce filtrate Synovial Joints General Structure • Other Components – – Cushioning fatty pads – Articular discs – menisci – wedges of fibrocartilage Ligament Joint cavity (contains synovial fluid) Articular (hyaline) cartilage Fibrous capsule Synovial membrane Articular capsule Periosteum Figure 8.3 Brusae And Tendon Sheaths • • • • Associated with joints Bags of lubricants Ball bearings – reduce friction Bursae – flattened fibrous sacs – Thin film of synovial fluid – Occur where ligaments, muscles, skin, tendons, or bones rub together • Tendon Sheath – – Elongated bursae wraps completely around tendon subjected to friction – Where several tendons crowded together Coracoacromial ligament Subacromial bursa Cavity in bursa containing synovial fluid Humerus resting Bursa rolls and lessens friction. Humerus head rolls medially as arm abducts. Humerus moving (b) Enlargement of (a), showing how a bursa eliminates friction where a ligament (or other structure) would rub against a bone Figure 8.4b Stability of Synovial Joints • Stabilized – so do not dislocate • Stability depends on – 1. Shape of articular surfaces 2. Number and position of ligaments 3. Muscle tone Stability of Synovial Joints 1. Articular Surfaces – • Shapes determine movements possible • Minor role in stability • Many joints – shallow sockets – noncomplementary articulating surfaces • When large – socket deep – stability vastly improved Stability of Synovial Joints 2. Ligaments – more ligaments – stronger • Brace joints 3. Muscle Tone – muscle tendons cross joints • Tendons taught at all times • Muscle tone – low levels of contractile activity in relaxed muscles keep them muscles healthy and ready to react Movements Allowed by Synovial Joints • Muscle origin – attached to immobile or less movable bone • Insertion – attached to movable bone • Muscle contract – insertion moves towards origin • Nonaxial movement – slipping movements only – no axis • Uniaxial movements – movement in 1 plane • Biaxial movement – movement in 2 planes • Multiaxial movement – movement in or around all 3 planes and axes 3 General Types of Movement 1. Gliding 2. Angular Movements 3. Rotations 1. Gliding • • • • • Simplest One flat bone surface slides over another Back and forth, side to side No angulations or rotation Intercarpal and intercostal joints Gliding (a) Gliding movements at the wrist Figure 8.5a 2. Angular • Increase or decrease angle between 2 bones • Any plane of the body • Include – flexion, extension, hyperextension, abduction, adduction and circumduction Hyperextension Extension Flexion (b) Angular movements: flexion, extension, and hyperextension of the neck Figure 8.5b 2. Angular A. Flexion • Bending movement • Usually along sagittal plane • Decrease angle of joint • Head toward chest Extension Hyperextension Flexion (c) Angular movements: flexion, extension, and hyperextension of the vertebral column Figure 8.5c 2. Angular B. Extension • Reverse of flexion • Occurs at same joints • Movement along sagittal plane • Increase the angle • Straightens a flexed limb or body part • Ex. Straightening the knee • Hyperextension – extension beyond anatomical position Extension Hyperextension Flexion (c) Angular movements: flexion, extension, and hyperextension of the vertebral column Figure 8.5c 2. Angular C . Abduction • “moving away” • Movement of a limb away from the midline • Along frontal plane Abduction Adduction Circumduction (e) Angular movements: abduction, adduction, and circumduction of the upper limb at the shoulder Figure 8.5e 2. Angular D. Adduction – • “moving toward” • Opposite abduction • Movement of a limb toward body midline Abduction Adduction Circumduction (e) Angular movements: abduction, adduction, and circumduction of the upper limb at the shoulder Figure 8.5e 2. Angular E. Circumduction – • Moving limb so it describes a cone in space • Distal end of limb moves in a circle 3. Rotation • • • • Turning of bone around its long axis 1st – 2 cervical vertebrae Hip, shoulder Towards or away from midline Rotation Lateral rotation Medial rotation (f) Rotation of the head, neck, and lower limb Figure 8.5f Special Movements • Do not fit into any of other categories • Supination “turning backwards” – radius around ulna • Pronation – “turning forward” – radius around ulna Pronation (radius rotates over ulna) Supination (radius and ulna are parallel) (a) Pronation (P) and supination (S) Figure 8.6a Special Movements • Dorsiflexion – increase and decrease movement of foot, foot superior – approaches shin • Plantar Flexion – pointing toes Dorsiflexion Dorsiflexion Plantar flexion Plantar flexion (b) Dorsiflexion and plantar flexion Figure 8.6b Special Movements • Inversion – sole of foot turns medially • Eversion – sole face laterally Inversion Eversion (c) Inversion and eversion Figure 8.6c Special Movements • Protraction – anterior movement in transverse plane • Retraction – posterior movement in a transverse plane Protraction of mandible Retraction of mandible (d) Protraction and retraction Figure 8.6d Special Movements • Elevation – lift body part superiorly • Depression – moving elevated part inferiorly Elevation of mandible Depression of mandible (e) Elevation and depression Figure 8.6e Special Movements • Opposition – joint between metacarpal 1 and trapezium • Movement of thumb Opposition (f) Opposition Figure 8.6f Types of Synovial Joints • 6 categories – 1. Plane Joint – – Flat – Allow only short non-axial gliding movement – No rotation – Non-axial plane joints f Nonaxial Uniaxial Biaxial Multiaxial c b a Plane joint (intercarpal joint) a e d Figure 8.7a Types of Synovial Joints 2. Hinge Joints – • Cylindrical end of bone conforms to trough shaped surface • Motion – single plane • Resembles mechanical hinge • Permit flexion and extension only f Nonaxial Uniaxial Biaxial Multiaxial c b Hinge joint (elbow joint) b a e d Figure 8.7b Types of Synovial Joints 3. Pivot Joints – • Rounded end of bone conforms to “sleeve” or ring composed of bone • Uniaxial rotation • Atlas and dens joint • Ex. Head side to side f Nonaxial Uniaxial Biaxial Multiaxial c b c Pivot joint (proximal radioulnar joint) a e d Figure 8.7c Types of Synovial Joints 4. Condyloid Joint – • Also ellipsoidal joint • Fits into complete depressions in another articulating surfaces oval • Angular motion • Ex. Radiocarpal joints f Nonaxial Uniaxial Biaxial Multiaxial c b d Condyloid joint (metacarpophalangeal joint) a e d Figure 8.7d Types of Synovial Joints 5. Saddle Joints – • Like condyloid joint but allow greater motion • Both concave and convex areas • Shaped like a saddle • Carpometacarpal joint of thumb f Nonaxial Uniaxial Biaxial Multiaxial c e Saddle joint (carpometacarpal joint of thumb) b a e d Figure 8.7e Types of Synovial Joints 6. Ball and Sockets – • Spherical or hemispherical head of one bone articulates with cup like socket of another • Multiaxial and most freely moving synovial • Universal movement – shoulder and hip f Nonaxial Uniaxial Biaxial Multiaxial c b f Ball-and-socket joint (shoulder joint) a e d Figure 8.7f Synovial Joints- Knee Joint • Largest, most complex joint of body • Three joints surrounded by a single joint cavity: – Femoropatellar joint: • Plane joint • Allows gliding motion during knee flexion – Lateral and medial tibiofemoral joints between the femoral condyles and the C-shaped lateral and medial menisci (semilunar cartilages) of the tibia • Allow flexion, extension, and some rotation when knee is partly flexed Femur Articular capsule Posterior cruciate ligament Lateral meniscus Anterior cruciate ligament Tibia Tendon of quadriceps femoris Suprapatellar bursa Patella Subcutaneous prepatellar bursa Synovial cavity Lateral meniscus Infrapatellar fat pad Deep infrapatellar bursa Patellar ligament (a) Sagittal section through the right knee joint Figure 8.8a Anterior Anterior cruciate ligament Articular cartilage on lateral tibial condyle Articular cartilage on medial tibial condyle Lateral meniscus Medial meniscus Posterior cruciate ligament (b) Superior view of the right tibia in the knee joint, showing the menisci and cruciate ligaments Figure 8.8b Synovial Joints- Knee Joint • At least 12 associated bursae • Capsule is reinforced by muscle tendons: – E.g., quadriceps and semimembranosus tendons • Joint capsule is thin and absent anteriorly • Anteriorly, the quadriceps tendon gives rise to: – Lateral and medial patellar retinacula – Patellar ligament Quadriceps femoris muscle Tendon of quadriceps femoris muscle Patella Lateral patellar retinaculum Medial patellar retinaculum Tibial collateral ligament Fibular collateral ligament Patellar ligament Fibula Tibia (c) Anterior view of right knee Figure 8.8c Synovial Joints- Knee Joint • Capsular and extracapsular ligaments – Help prevent hyperextension • Intracapsular ligaments: – Anterior and posterior cruciate ligaments – Prevent anterior-posterior displacement – Reside outside the synovial cavity Femur Tendon of adductor magnus Medial head of gastrocnemius muscle Popliteus muscle (cut) Articular capsule Oblique popliteal ligament Lateral head of gastrocnemius muscle Bursa Tibial collateral ligament Fibular collateral ligament Tendon of semimembranosus muscle Arcuate popliteal ligament Tibia (d) Posterior view of the joint capsule, including ligaments Figure 8.8d Synovial Joint – Shoulder Joint • Ball-and-socket joint: head of humerus and glenoid fossa of the scapula • Stability is sacrificed for greater freedom of movement Acromion of scapula Coracoacromial ligament Subacromial bursa Fibrous articular capsule Tendon sheath Synovial cavity of the glenoid cavity containing synovial fluid Hyaline cartilage Synovial membrane Fibrous capsule Tendon of long head of biceps brachii muscle Humerus (a) Frontal section through right shoulder joint PLAY Animation: Rotatable shoulder Figure 8.10a Synovial Joint – Shoulder Joint • Reinforcing ligaments: – Coracohumeral ligament—helps support the weight of the upper limb – Three glenohumeral ligaments—somewhat weak anterior reinforcements Synovial Joint – Shoulder Joint • Reinforcing muscle tendons: – Tendon of the long head of biceps: • Travels through the intertubercular groove • Secures the humerus to the glenoid cavity – Four rotator cuff tendons encircle the shoulder joint: • Subscapularis • Supraspinatus • Infraspinatus • Teres minor Acromion Coracoacromial ligament Subacromial bursa Coracohumeral ligament Coracoid process Articular capsule reinforced by glenohumeral ligaments Subscapular Greater bursa tubercle of humerus Tendon of the Transverse subscapularis humeral muscle ligament Scapula Tendon sheath Tendon of long head of biceps brachii muscle (c) Anterior view of right shoulder joint capsule Figure 8.10c Acromion Coracoid process Articular capsule Glenoid cavity Glenoid labrum Tendon of long head of biceps brachii muscle Glenohumeral ligaments Tendon of the subscapularis muscle Scapula Posterior Anterior (d) Lateral view of socket of right shoulder joint, humerus removed Figure 8.10d Synovial Joint – Elbow Joint • Radius and ulna articulate with the humerus • Hinge joint formed mainly by trochlear notch of ulna and trochlea of humerus • Flexion and extension only Articular capsule Synovial membrane Humerus Synovial cavity Articular cartilage Fat pad Tendon of triceps muscle Bursa Coronoid process Tendon of brachialis muscle Ulna Trochlea Articular cartilage of the trochlear notch (a) Median sagittal section through right elbow (lateral view) Figure 8.11a Synovial Joint – Elbow Joint • Anular ligament—surrounds head of radius • Two capsular ligaments restrict side-to-side movement: – Ulnar collateral ligament – Radial collateral ligament Humerus Anular ligament Radius Lateral epicondyle Articular capsule Radial collateral ligament Olecranon process Ulna (b) Lateral view of right elbow joint Figure 8.11b Articular capsule Anular ligament Humerus Coronoid process Medial epicondyle Ulnar collateral ligament Radius Ulna (d) Medial view of right elbow PLAY Animation: Rotatable elbow Figure 8.11d Synovial Joint - Hip (Coxal) Joint • Ball-and-socket joint • Head of the femur articulates with the acetabulum • Good range of motion, but limited by the deep socket • Acetabular labrum—enhances depth of socket Coxal (hip) bone Articular cartilage Acetabular labrum Femur Ligament of the head of the femur (ligamentum teres) Reinforcing ligaments: Iliofemoral ligament Pubofemoral ligament Ischiofemoral ligament Ligamentum teres Synovial cavity Articular capsule (a) Frontal section through the right hip joint Figure 8.12a Synovial Joint - Hip (Coxal) Joint Reinforcing ligaments: • Iliofemoral ligament • Pubofemoral ligament • Ischiofemoral ligament • Ligamentum teres Iliofemoral ligament Ischium Ischiofemoral ligament Greater trochanter of femur (c) Posterior view of right hip joint, capsule in place PLAY Animation: Rotatable hip Figure 8.12c Anterior inferior iliac spine Iliofemoral ligament Pubofemoral ligament Greater trochanter (d) Anterior view of right hip joint, capsule in place Figure 8.12d Temporomandibular Joint (TMJ) • Mandibular condyle articulates with the temporal bone • Two types of movement – Hinge—depression and elevation of mandible – Gliding—e.g. side-to-side (lateral excursion) grinding of teeth • Most easily dislocated joint in the body Mandibular fossa Articular tubercle Zygomatic process Infratemporal fossa External acoustic meatus Lateral ligament Articular capsule Ramus of mandible (a) Location of the joint in the skull Figure 8.13a Mandibular fossa Articular disc Articular tubercle Superior joint cavity Articular capsule Synovial membranes Mandibular condyle Ramus of Inferior joint mandible cavity (b) Enlargement of a sagittal section through the joint Figure 8.13b Superior view Outline of the mandibular fossa Lateral excursion: lateral (side-to-side) movements of the mandible Figure 8.13c Common Joint Injuries • Sprains – The ligaments are stretched or torn – Partial tears slowly repair themselves – Complete ruptures require prompt surgical repair • Cartilage tears – Due to compression and shear stress – Fragments may cause joint to lock or bind – Cartilage rarely repairs itself – Repaired with arthroscopic surgery Torn meniscus Figure 8.14 Common Joint Injuries • Dislocations (luxations) – Occur when bones are forced out of alignment – Accompanied by sprains, inflammation, and joint immobilization – Caused by serious falls or playing sports • Subluxation—partial dislocation of a joint Homeostatic Imbalances • Bursitis – An inflammation of a bursa, usually caused by a blow or friction – Treated with rest and ice and, if severe, antiinflammatory drugs • Tendonitis – Inflammation of tendon sheaths typically caused by overuse – Symptoms and treatment similar to bursitis Homeostatic Imbalances • Arthritis – • >100 different types of inflammatory or degenerative diseases that damage joints • Most widespread crippling disease in the U.S. • Symptoms; pain, stiffness, and swelling of a joint • Acute forms: caused by bacteria, treated with antibiotics • Chronic forms: osteoarthritis, rheumatoid arthritis, and gouty arthritis Homeostatic Imbalances • Osteoarthritis (OA) • Common, irreversible, degenerative (“wear-and-tear”) arthritis • 85% of all Americans develop OA, more women than men • Probably related to the normal aging process • More cartilage is destroyed than replaced in badly aligned or overworked joints • Exposed bone ends thicken, enlarge, form bone spurs, and restrict movement • Treatment: moderate activity, mild pain relievers, capsaicin creams, glucosamine and chondroitin sulfate Homeostatic Imbalances • Rheumatoid Arthritis (RA) • Chronic, inflammatory, autoimmune disease of unknown cause • Usually arises between age 40 and 50, but may occur at any age; affects 3 times as many women as men • Signs and symptoms include joint pain and swelling (usually bilateral), anemia, osteoporosis, muscle weakness, and cardiovascular problems Homeostatic Imbalances • Rheumatoid Arthritis (RA) cont • RA begins with synovitis of the affected joint • Inflammatory blood cells migrate to the joint, release inflammatory chemicals • Inflamed synovial membrane thickens into a pannus • Pannus erodes cartilage, scar tissue forms, articulating bone ends connect (ankylosis) Figure 8.15 Homeostatic Imbalances • Rheumatoid Arthritis (RA) Treatment • Conservative therapy: aspirin, long-term use of antibiotics, and physical therapy • Progressive treatment: anti-inflammatory drugs or immunosuppressants • New biological response modifier drugs neutralize inflammatory chemicals Homeostatic Imbalances • Gouty Arthritis – • Deposition of uric acid crystals in joints and soft tissues, followed by inflammation • More common in men • Typically affects the joint at the base of the great toe • In untreated gouty arthritis, the bone ends fuse and immobilize the joint • Treatment: drugs, plenty of water, avoidance of alcohol Homeostatic Imbalances • Lyme Disease – • Caused by bacteria transmitted by the bites of ticks • Symptoms: skin rash, flu-like symptoms, and foggy thinking • May lead to joint pain and arthritis • Treatment: antibiotics Developmental Aspects • By embryonic week 8, synovial joints resemble adult joints • A joint’s size, shape, and flexibility are modified by use • Advancing years take their toll on joints: – Ligaments and tendons shorten and weaken – Intervertebral discs become more likely to herniate – Most people in their 70s have some degree of OA • Exercise that coaxes joints through their full range of motion is key to postponing joint problems