ACC * D week
advertisement
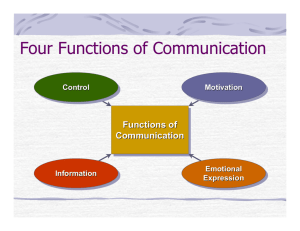
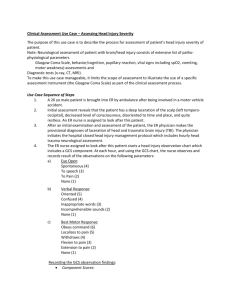
ACC – D week Aaqid Akram MBChB (2013) Clinical Education Fellow Objectives • Be able to calculate GCS in adults/children • Be able to assess and manage a patient with head/neck injury • Be able to recognise and manage problems with alcohol use • Be able to recognise and manage drug overdoses • Be able to recognise and manage meningitis • Be able to recognise and manage seizures Case 1 • • • • • • • 50 year old male Intoxicated with alcohol Brought in by ambulance 2 hours ago Tripped over and fell 8 steps on the way back home haematoma noticed on the left temporal area of head Disorientated in time an place Unaware of the falling episode or why he is here, but aware he was going home • Following the nurses around the department, but sits down in cubicle when you call him over. • Making inappropriate sexual remarks Glasgow Coma Score Score Response 4 Spontaneous 3 Sound 2 Pain 1 Unresponsive 5 Orientated 4 Confused 3 Words 2 Sounds 1 Unresponsive 6 Obeys commands 5 Localising pain 4 Normal flexion 3 Abnormal flexion 2 Extension 1 Unresponsive Eyes (E) Verbal (V) Motor (M) Case 2 • • • • • • • • • • 11 month old infant Brought in by mother Slipped out of arms and into the bath half an hour ago Hit occiput on bath floor Has since been crying intermittently There was immediate crying On examination there is a 4cm swelling Not other abnormalities on inspection Fontanelle still palpable and soft Infant is looking for mother and reaching out to her Case 2 continued • The infant was taken to the paediatric ward for observation • Two hours later • Supraorbital pressure induced flexion, moaning and opening of eyes Child’s Glasgow Coma Score Score >5 years old <5 years old 4 Spontaneous 3 Sound 2 Pain 1 Unresponsive Eyes (E) Verbal (V) 5 Orientated Alert, babbling, coos, words for normal ability 4 Confused Less than usual ability, irritable cry 3 Words Cries to pain 2 Sounds Moans to pain 1 6 Unresponsive Obeys commands Normal spontaneous movements 5 Localising to supraorbital pain (>9 months) / (<9 months) withdraws to touch 4 Withdraws form nail bed pain 3 Flexion to supraorbital pain (decorticate) 2 Extension to supraorbital pain (decerebrate) 1 Unresponsive (flaccid) Motor (M) Case 3 • 45 year old female • Had recently decided she was going to turn a new leaf • Tachycardia • Anxiety / Sweating • No chest pain • Tremulous • Disorientated in time an place • No injuries on inspection • No enlarged organs on examination Alcohol withdrawal Alcohol GABAa receptor stimulation Sudden alcohol withdrawal Uncontrolled synapse firing CNS depression Unopposed sympathetic stimulation Continued alcohol Down-regulation (No + Sensitivity) of GABAa Autonomic hyperactivity Agitation Confusion Anxiety N +V Hallucinations Impaired GCS Acute Alcohol Withdrawal Delerium Tremens Disorientation Seizures Tremor Tachycardia Delerium Sweating Scoring Systems • CAGE Questionnaire: – Have you thought about cutting down ? – Are you annoyed by others criticism of your drinking? – Do you feel guilty about your drinking? – Do you need an eye opener • AUDIT Questionnaire: – Alcohol Use Disorders Identification Test • CIWA Ar Scoring: – (Alcohol withdrawal assessment scoring guidelines) – Ten item scale for assessment and management of alcohol withdrawal – Helps to prevent over sedation /under-treatment of in-patients – Mild <16, Severe >20, Max = 67 CIWA Ar • • • • • Chlordiazepoxide (Librium) 40-50mg po Repeat every 2 hours prn Score>35 or unrelenting symptoms – ICU input • Day 1 total usage – Baseline • Day 2-6 reducing doses Further Management • Pabrinex – 2 pairs (I+II + I+II) TDS for 2 days – 1 pair (I+II) OD for the next 3 days • • • • • • Vitamin B1 – Thiamine Vitamin B2 – Riboflavin Vitamin B3 – Nicotinamide Vitmain B6 – Pyridoxine Vitamin C – Ascorbic Acid Anhydrous Glucose • Oral Thiamine + Vit B Co-Strong Case 3 continued • • • • • • • • Same female comes in 3 months later Back on alcohol 80 units a day No appetite Does not take prescribed supplements Very unsteady on feet with wide gait Confused On examination, nystagmus seen and unable to look laterally Wernicke’s Encephalopathy • Triad – Opthalmoplegia – Ataxia – Confusion • Low levels of thiamine – GI malabsorption / diet – Impaired utilisation by cells • Oxidative damage – Pro-apoptotic mechanism – Mitochondrial damage – Neurons/astrocytes • Korsakoff’s Syndrome Effects of alcohol Neuro: CVS: Hypertension / AF / Cardiomyopathies / Heart Failure Wernike’s / Korsakoff’s / Psychosis / Confusion / panic disorder / depression / seizures / neuropathies Pancreas: Alcohol Ketoacidosis Acute / Chronic Pancreatitis Gastrointestinal: Liver: Bleeds / Cancers Fatty / hepatitis / cirrhosis Endocrine/Hormone: Bone: Osteoporosis Gonadal Atrophy Case 4 • • • • • • • • • 20 year old male Brought into emergency department by Ambulance Generalised tonic-clonic seizure in Tesco car park Appx 3 mins No head injury noted Now in post ictal state – drowsy but interacting No temperature No previous history of seizures Not aware of seizure – remembers walking out of Tesco and then in the ambulance Case 4 continued • On seeing your next patient the wall alarm has been pulled by the mother of the patient • He is having a tonic clonic seizure Case5 • • • • • • • • 26 month old child Unwell for 3 days Grunting last night Not feeding today Very sleepy – opening eyes to voice Pyrexial Irritable crying Floppy hands and feet, but moves hand if attempting nailbed pain • Notice a non blanching rash behind right knee Moved to Resus A. No additional Airway noises B. RR 50 / SpO2 unrecordable C. CRT 5 seconds / HR 180 / Nappy dry since last night D. GCS: 11 IV Access Fluid Resuscitation Raised ICP • X2 large bore • Use one to immediately commence Ceftriaxone 80mg/kg • FBC / U+E / CRP / Blood gas / blood cultures / Bone profile / Mg / lactate / clotting / cross match • Bolus 20ml/kg 0.9% NaCl + Reassess • Second bolus 20ml/kg 0.9% NaCl + Reassess • If still signs of shock urgent elective intubation and ventilation • Once no signs of shock only – DO NOT PERFORM LP • GCS < 9 / fluctuating GCS • Bradycardia + hypertension • abnormal posture / seizures / unequal pupils / papilloedema / dolls eyes Meningitis • Contact public health / ID consultant on call • Kissing contacts / household / room mates – Prophylaxis/immunisation – Ciprofloxacin / ceftriaxone • Causes – – – – – – Viral (enterovirus / mumps / measles / influenza) Bacterial Fungal (cryptococcus / blastomyces / histoplasma) TB Parasitic Other (iatrogenic / cancer / drugs / head injury) Bacterial Meningitis Age Group Pathogens Newborn Group B strep / E Coli / Listeria Infants / Children S Pneumoniae / N Meningitidis / HIb Young Adults S Pneumonaie / N Meningitidis Older Adults S Pneumonaie / N Meningitidis / Listeria CSF Pathogen Glucose Protein WCC Appearance Normal 60-80% plasma 0.2-0.4 g/L <5/mm3 Clear / no colour Bacterial Low (<50%) High (>1.5) Neutrophils >1000/mm3 Cloudy / turbid Viral Normal Normal / High lymphocytes Clear TB Low (<50%) Very High (> bacterial) Mix Clear / slightly cloudy Case 6 • • • • • • Variable Value O RA 24 year old female SpO 94% Deliberate overdose RR 9 HR 75 Co-codamol + Aspirin Temp 37.1 Staggered BP 110/60 Orientated in time, place and person Wants to be left asleep and only opens eyes and tries to move hand away, when applying supraorbital pressure 2 2 Further History • • • • • • • • • Quantity and strength of each Time take if possible Anything else taken? Alcohol Any other regular medication Previous attempts at self harm/suicide Current reasons/motives Mental health contact Patient’s weight Paracetamol OD Codeine (opiate) OD • Asymptomatic • Nausea / vomiting • RUQ tenderness • Jaundice (Late) • Hepatic Encephalopathy • Reduced GCS • Pinpoint pupils • Reduced RR • Bradycardia • Coma NSAID OD • Asymptomatic • Epigastric pain • Nausea / Vomiting • GI bleeding • Renal failure Salicylate OD • Mild Pyrexia • Tinnitus • Nausea / Vomiting • Hypotension • Tachycardia Parvolex (N-Acetylcysteine) • Total dose given in 3 consecutive IV infusions over 21 hours. 1. 150mg/kg in 200ml of 5% glucose over 1 hour 2. 50mg/kg in 500ml of 5% glucose over 4 hours 3. 100mg/kg in 1000ml of 5% glucose over 16 hrs • In very obese patients (>110kg) the dose should be calculated using a body weight of 110kg rather than their actual weight. Objectives were: • Be able to calculate GCS in adults/children • Be able to assess and manage a patient with head/neck injury • Be able to identify and manage problems with alcohol use • Be able to identify and manage drug overdoses • Be able to identify and manage meningitis • Be able to identify and manage seizures