End of Life Care Education
MODULE 1
Case Scenario 1
End of Life Care Webinar
Case: A
78-year old male; good prior health; admitted with acute SDH; GCS 7
Started on mechanical ventilation peri-op. with expected wean by 2-4 days
Poor response to Rx, no GCS ; VAP; respiratory failure worsens; BP
drops; kidney fails; antibiotic resistant infection; still very sick on day 12
F Doctor feels ongoing treatment is unlikely to help
F Family friend who knows you requests cessation of all Rx
What is your outlook?
A Case for Limiting Treatment
•
Death from serious illness is not inevitable;
technology can save lives (!)
•
Medical intervention is given to all patients, in
order to save a few lives
•
In situations where support is unlikely to benefit
the patient:
•
•
Offering ongoing treatment is deceit
May strain limited societal resources
Decision Making:
The Ethical Basis
•
Autonomy
–
–
The patient’s decisions are supreme
The family as surrogate decision makers
•
Beneficence
•
Non-malficence
–
•
Do no harm; “Primum non nocere”
Justice
–
Individual vs. distributive
Ideal Approach to the Case:
• Agree to stop treatment after family
(appropriate surrogates) consensus is
established because you
• are professionally obliged not to
• continue non-beneficial treatments
Ideal
Ethically correct
Physician takes responsibility
Effective palliative measures
can be administered
Misguided
Alternative Approach 1:
• Refuse to stop treatment because you
do
• believe that “euthanasia” is morally
• unacceptable
Naïve justification
Limiting therapy is ethical:
Honest approach
to failing Rx
Minimizes patient discomfort
Guarantees distributive justice
Death is not an intended goal
The morality of euthanasia?:
Its goal is to end life
Euthanasia
Opinions of Indian Doctors
•
There is some confusion about the “intent” of treatment
limitation:
–
–
•
54% equated withholding therapy with “mercy killing”
64% equated withdrawal with it
Is euthanasia immoral?
–
–
42% considered it a valid option in an advanced cancer
scenario
We are unaware if these doctors would assist patients’
suicide
Self-Centered
Approach 2:
• Refuse to limit life-support
measures
• because you are concerned about
the
• legal ramifications of withdrawal /
• withholding
Self interest (fear of litigation) primary
Cost of continued care may be high
? False promise
Scope for abuse………
Approach 2:
Does not help
the
“Public Image”
of the
Profession ,
does it?
Approach 3:
• Refuse to stop treatment; but
‘suggest’
• the family “take the patient home”
• “against medical advice”
The Ethics(?) of LAMA
(Leaving “Against Medical Advice”):
It is treatment withdrawal in an
atmosphere of uncertainty (legal / social)
Coercive (patient takes the ‘blame’)
Paternalistic
Provokes distrust of the profession
Huge scope for abuse
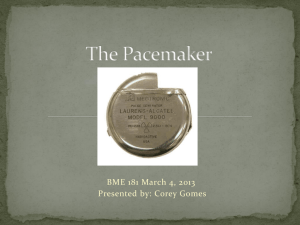
Case B
Mr. A, 65 yr old came with a pacemaker inserted 8 weeks ago in
another hospital. He had fever and was found to have an infected
pacemaker and lead.
Started antibiotics and took out pacemaker and reinserted external
pacemaker by Cardiologist
Developed an RV puncture, took for surgery and an epicardial lead was
inserted
Could not wean off ventilator post op
Transferred to MICU. During the next few days, found diaphragmatic
paralysis (? External pacing) – removed and internal lead placed
medial wall of RV
No improvement in weaning – EMG / NCV – Critical Illness
Polyneuropathy
Tracheostomy done – prognosis explained to family; they want to go
home; no more money for Rx; patients wants therapy discontinued.
Case B - contd
Clinical Ethics Committee decision : Continue all Rx, no
additional cost
Family went home as they could not stay on
Psychiatric evaluation – Patient depressed, started
antidepressants and psychotherapy, visits by layperson
Continued Rx – next 6 weeks, gradually improved both
physically and emotionally
Weaned off at 8 weeks
Transferred back to Cardiology
THANK YOU
This education program is a joint initiative of Indian Society of Critical Care
Medicine and Indian Association of Palliative Care. 2014
© All rights reserved