Joints
Articular System (Joints)
ANHB 2212 – 2007
Avinash Bharadwaj
Joints
“Articulation”
Articulatio / Arthron Arthrology
Where two or more bones or parts of bones unite…
How they are joined together… the tissues that unite bones
Joint Classification
Structural
The tissues that unite bones
Functional
Mobility or otherwise
Synovial joints – axes of movements
No perfect system (Explained as we go!)
Arbitrary and confusing terms
Overlapping terminology
Latin terminology and anglicised versions
The choice is yours!
Tissues Uniting Bones
Fibrous tissue
Unossified tissue between membrane bones
(Explained fully next week!)
Ligaments (Dense connective tissue!)
Cartilage
Hyaline cartilage
White fibrocartilage
Fibrous capsule with a cavity
Special features for lubrication, movement and stability
Movable Joints
“Movability” (mobility…?) is a relative term!
Movement is always associated with restrictions
Active movements – by muscles
Movements due to other factors
Shapes of bony surfaces
Tensions in ligaments
Other external factors (pelvic joints in childbirth)
Passive movements in clinical examination
Fibrous Joints
Sutures (“stitches”)
Between flat bones of the skull
Surface view
Section (Magnified!)
Bone
Periosteum
Fibrous Joints
Syndesmoses
Inferior tibiofibular joint
(Not shown here)
Interosseous membranes
Separation of compartments
Additional areas for muscle attachments
Some other ligaments…
Gomphoses
Tooth and bone
“Peg-and-socket”
R
U
Cartilaginous Joints
Synchondrosis – Hyaline cartilage
Growth mechanism synostosis
Between primary and secondary centres
Between named bones (e.g. sphenoid + occipital)
(Week 12 Histology!)
Symphysis – White fibrocartilage
WFC is deformable
Partially movable joints
Occasional cavities – ? Evolution of synovial joints
Primary and secondary cartilaginous joints : terms best avoided.
Functionally two distinct entities.
Cartilaginous Joints
Synovial Joints
“Freely movable”…?
Freedom is relative!
More movable than any other type…!
Fibrous tissue bond, with a cavity
Synovial Joints – Basic Features
The bones – articular surfaces
Smooth… but not quite!
Articular cartilage
Fibrous capsule
Ligaments
Capsular thickening
External
Synovial membrane
Synovial Joints – Articular Cartilage
Hyaline (WFC in membrane bones)
No perichondrium
Variable thickness
Depends on the type of joint
In curved surfaces
Convex – thick in the centre
Concave – thin in the centre
Synovial Joints – Capsule Etc
Capsular attachment
Thickening of capsule : “Intrinsic” ligaments
Areas of strength / weakness
Capsule may be loose in places
Other ligaments (“extracapsular”)
Synovial membrane and fluid
Intra-articular discs
White Fibrocartilage
Reduce incongruity
Modify movements
Spread of synovial fluid – reduce “drag”
Incomplete discs / menisci
Other Intra-articular Structures
Ligaments
Cruciate ligaments – knee joint
Tendons
Long head of biceps – shoulder joint
Popliteus – knee joint
Fat pads
Such structures are covered by synovial membrane.
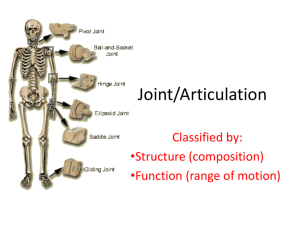
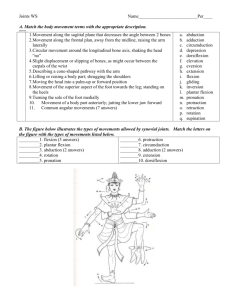
Synovial Joints – Subtypes
Functional
Degrees of freedom
Uniaxial, biaxial, multiaxial
Structural
Shapes of bony surfaces
Synovial Joints – Subtypes
Plane : Sliding movements
(“Non-axial joint”)
Hinge : Uniaxial (e.g. elbow)
Ball-and-socket : Multiaxial (Shoulder, hip)
Saddle : Two planes of movement + combinations
Bicondylar : Two pairs of surfaces
Pivot : Osseofibrous ring + rotating bone
Nothing is perfect – do not expect geometrical shapes!
Two Types Illustrated
Pivot joint –
Osseofibrous ring and head of radius.
Bicondylar joint – Knee
Two pairs of articular surfaces
Bursae
Muscles / tendons in close proximity – friction
Bursa (Latin for purse!)
Thin walled connective tissue bag
Lining of synovial membrane
Between joint capsule and tendon / muscle, bone and tendon / muscle, or between muscles / tendons.
Bursitis – painful
Some bursae communicate with joint cavity
Joint Stability
Movement and stability – a compromise
Factors in stability
Bony configuration
Capsule and ligaments
Tendons and muscles
Sometimes blend with capsule – rotator cuff
Nerves
Rich sensory innervation
Capsule, ligaments, periosteum
Same nerves as those that supply muscles
Joint pain
Bony injuries
Capsular / ligamentous injuries
Synovial membrane
And more…
Blood Vessels
Rich blood supply
All parts except cartilages
Articular cartilage
By diffusion through synovial fluid
Blood vessels of surrounding areas (capsule, bone)
Last Slide