Integrating basic sciences and patient care in Western
advertisement

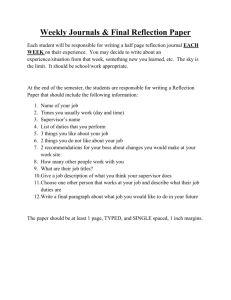
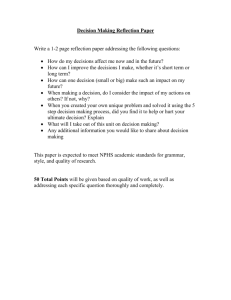
Integrating Basic and Clinical Sciences Presentation by: Amy L. Wilson-Delfosse, Ph.D. James Bruzik, Ph.D. Case Western Reserve University School of Medicine Why Did Case Change? The Western Reserve curriculum designed in the 1950s continued with only minor revisions despite enhancements in computer technology and unprecedented changes in the health care system Classrooms with ~30% of students attending Watching lectures online double time Paper syllabus boundaries Students not preparing for class Teacher-centered Why Did Case Change? Course silos “I don’t know if you’ve had this yet but” Multiple choice tests –nothing else counted, binge and purge approach to learning Difficult to get faculty to teach – clinical and research productivity Dean’s Vision – research and scholarship block and MD thesis Principles of Western Reserve2: Building on Western Reserve1 Integration of health and disease (normal and abnormal) – systems biology Experiential learning, scholarship, critical thinking, lifelong learning Active interchange of ideas between students and faculty Graduate school environment – independent study and selfdirected learning Weave scientific foundations and clinical medicine throughout the 4 year curriculum Principles of Western Reserve2: Building on Western Reserve1 Integration of health and disease (normal and abnormal) – systems biology Experiential learning, scholarship, critical thinking, lifelong learning Active interchange of ideas between students and faculty Graduate school environment – independent study and selfdirected learning Weave scientific foundations and clinical medicine throughout the 4 year curriculum Western Reserve2 Curriculum Year I Year II Year III Year IV Core Clinical Rotations IQ+ Program Foundations of Medicine and Health (20 months, including vacation) (48 weeks, flexible scheduling) Research & Scholarship (16 week block + electives, flexible scheduling) Advanced Clinical and Scientific Studies Areas of Concentration Electives (10 months, flexible scheduling) WR2 Foundations of Medicine and Health Structure (Anat., Histo-Path, Radiology) Foundations of Clinical Medicine (GI, Nutrition, Energy, Metabolism, Biochemistry) 1 Week Clinical Immersion (CV, Pulm, Renal, Cell Regulation, Pharmacology, Cell physiology) 1 Week Clinical Immersion (Host Defense, Microbiology, Blood, Skin, Auto-immune) Cognition, Sensation, and Movement 1 Week Clinical Immersion (Neuro, Mind Musculoskeletal, Cellular Neurophysiology Reflection, Integration & Assessment (Endo, Repro, Development, Genetics, Mol Biol, Cancer Biology) 1 Week Clinical Immersion Host Defense and Host Response Reflection, Integration & Assessment 1 Week Clinical Immersion Reflection, Integration & Assessment (Medical Error, Public Health, Inequities, Bioethics, Professionali sm Epi/Biostats) Homeostasis Food to Fuel Reflection, Integration & Assessment (5 wk) The Human Blueprint Reflection, Integration & Assessment Becoming a Doctor March Year 2 Reflection, Integration & Assessment July Year 1 B O A R D R E V I E W B L O C K Case Inquiry Group (IQ) Student-centered small groups with a faculty facilitator Case-based Self-directed learning Team work Quality improvement – “check out” WR2: Eary Patient Experiences August to December January (Year 1) to January Year 1 December (Year 2) Year 2 Introduction to clinical Advanced Clinical Skills skills RAMP (Rotating Clinical Preceptorships Apprenticeships in Medical Practice) FCM Seminars Health Policy, Leadership and Advocacy, Professionalism, Ethics Web Resources Integration and Assessment Core and Advanced Clinical Experiences: Core Clinical Rotations Core 1 (16 weeks): Internal Medicine and Surgery + Peri-Op and Acute Pain Core 2 (16 weeks): Pediatrics, OB-Gyn, Family Medicine (Prevention/Wellness) Core 3 (8 weeks): Neuroscience and Psychiatry + Chronic pain Advanced Cores (4 weeks each): Undifferentiated and Emergent Care Aging and Society: Geriatrics, Chronic Disease, Palliative Care, Health Systems 4 hours Friday afternoon in group of 10-12 students Reinforce importance of basic science and emerging basic science knowledge in the practice of clinical medicine Continue to use a team-based, learner-centered small group to enhance professional growth and development Practice advanced skills in communication, physical exam, clinical reasoning, evidence based medicine Reflection Case discussion – DDX and learning objectives Research and discussion with experts (basic science and clinical faculty) Skills practice Checkout Example Case: HLHS Check-in: Debrief, possible directed reflections on dealing with a sick child or the parent of a sick child. Go through the case in step by step – starting with a “blue baby”– generate a differential diagnosis, discuss the perinatal changes in the circulation Come up with a list of learning objectives and questions for the experts. HLHS continued … Expert session - paired basic scientist & neonatologist meet with larger group. Mini-didactics + Q+A – focusing on emerging science on the heritable nature of this problem + clinical insights. HLHS continued … Skills practice – Students interview the standardized parent of this baby – script calls for integration of recently learned information + focus on delivering bad news and communicating with families. Check out Assessment Attendance Facilitator assessment Case development/presentation (teams) Students write cases and run the IQ+ afternoon Opportunities for scholarship Opportunities for peer teaching Acknowledgements The faculty, staff and students of CWRU School of Medicine