Diabetes Mellitus
advertisement

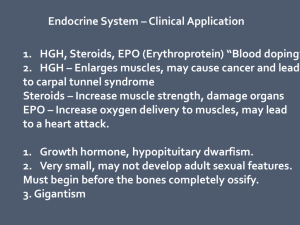
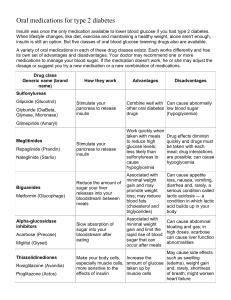
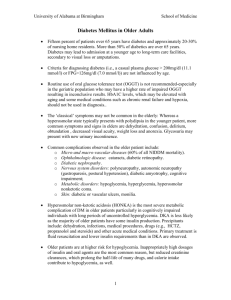
Diabetes Mellitus (Part II) Treatment Acute Complications Chronic Complications Patient Teaching Drug Therapy: Insulin Oral Agents Nutritional Therapy Exercise Pancreas Transplant Treatment • The goal of any treatment for Diabetes: Reduce symptoms Promote well-being Prevent acute complications Prevent or delay the onset and progression of long-term complications • Above goals can only be met by patient maintaining blood glucose levels at or near normal! Insulin Therapy (Exogenous Insulin) • Patients with Type 1 Diabetes always require Exogenous insulin (insulin from a source outside the body) • Type 2 Diabetics may not need any insulin Blood Glucose Levels can be controlled by diet & exercise alone May need insulin eventually due to chronic and progressive nature of the disease Types of Insulin • • • • No longer made from beef or pork pancreas Only human insulin is used today Human insulin made from bacteria or yeast cells Insulins differ in regard to: Onset Peak action Duration • Characterized according to the amount of time they need to take effect • Read the label carefully See Insulin Comparison Chart Insulin Therapy • Specific properties of each type of insulin are matched with the patient’s diet and activity • Can range from one injection per day to several injections of various types of insulin • Most closely resembles endogenous insulin production: Basal-bolus regimen • The regimen chosen should be mutually selected by the patient and the HCP • Criteria for selection are based on the desired and feasible levels of glycemic control and the patient’s lifestyle Fast/Rapid Acting Insulin Rapid-acting • Mealtime Insulin – Bolus • Used to control post-meal blood glucose levels • Rapid Acting Insulin: Onset = 15 minutes • Should be given 15 minutes before a meal Humalog Novolog Short acting Regular Insulin: Onset = 30-60 minutes “Regular” • Should be injected 20-30 minutes before a meal Intermediate Acting Insulin • NPH Insulin Onset 2-4 hours Peaks 4-12 hours Duration - 16-24 hours Generally given twice a day before meals Long Acting (Basal) Background Insulin • Long-acting/basal (background) insulin to control blood glucose levels between meals and overnight • Provides 24 hour steady and continual background insulin to keep blood glucose levels at a constant or controlled level Lantus Levemir • No Peak Risk for hypoglycemia greatly reduced Long Acting Insulin (cont’d) • Lantus and/or Levemir: Given once in the morning or at bedtime Cannot be mixed (in syringe) with other insulins Cannot be pre-filled Combination Insulin • Insulins can generally be mixed in the same syringe • Some Insulins Come Pre-mixed Novolin 70/30 mix 70% NPH – 30% Novolin Regular Novolog 70/30 mix 70% NPH – 30% Novolog Regular Humulin 50/50 mix Humalog 75/25 Administration of Insulin • Insulin is inactivated by gastric juices – cannot be taken orally Injection Insulin Pen Insulin Pump Inhaled Insulin Administration of Insulin: Subcutaneous Injection • Injection • Gently rotate insulin in hands to warm • Mixing Insulins for Injection Lantus/Levemir cannot be mixed Don’t mix insulins from different manufacturers • Regular/NPH Insulin mix: Draw up Regular insulin first, then add NPH Subcutaneous Insulin Injection (cont’d) • Absorption of Insulin varies according to the injection site used Slower Fastest Insulin Administration (cont’d) The Insulin Pen Compact & Portable Looks less like a syringe Handy, Calibrated Pre-filled with Insulin * Change needle for each use Insulin Pump Can be worn on belt or clothing Tubing inserted into subcutaneous tissue in abdomen Site must be changed every 3 days Can deliver basal rate, short and long acting insulin User programs according to exercise, diet, etc. ) Insulin Pump The MiniMed Paradigm insulin pump (A) delivers insulin into a cannula (B) that sits under the skin. Continuous glucose monitoring occurs through a tiny sensor (C) inserted under the skin. Sensor data are sent continuously to the insulin pump through wireless technology. Courtesy of Medtronic Diabetes. Inhaled Insulin (Exubera) • Alternative to injectable insulin • Rapid Acting; replaces short-acting ‘coverage’ insulins • Inhaled before meals • Usually added to longer acting insulins for type 1 diabetics •Type 2 diabetics: Alone or with any combination of prescribed insulins •Contraindications: Smoker Quit smoking within last 6 months Asthma PFTs before prescribed Problems with Insulin Therapy • Allergic Reactions Local; itching, burning usually due to additives True insulin allergy is rare, but can be anaphylactic • Lipodystrophy: Atrophy of subcutaneous tissue Prevented by rotation of sites May result in poor absorption of insulin • Somogyi Effect • Dawn Phenomenon Somogyi Effect • Somogyi Effect is a ‘rebound’ effect Overdose of insulin induces hypoglycemia Usually occurs during hours of sleep • Normal/elevated blood glucose at bedtime, a decrease at 2-3 am hypoglycemic levels, and increase caused by the production of counterregulatory hormones released, producing rebound hyperglycemia • The danger the morning BGL can be high in response to the counterregulatory hormones and the MD may increase the insulin dose Dawn Phenomenon • Similar to Somogyi • Relatively normal glucose until about 3am then the glucose level begins to rise. • Hyperglycemia is present on awakening in the morning due to the release of counterregulatory hormones in the pre-dawn hours. Possibly caused by growth hormone Affects all diabetics at one time or another, more severe when growth hormone is at it’s peak o Adolescence and young adulthood Careful monitoring of insulin, snacks and BGLs Oral Drug Therapy Oral Agents are NOT oral forms of insulin • Oral agents work to improve the mechanisms by which insulin and glucose are produced and used by the body – they work on the 3 defects of type 2 diabetes: 1. Insulin resistance 2. Decreased insulin production 3. Increased hepatic glucose production • May be taken in combination with each other or with insulin to achieve BGL targets Oral Hypoglycemic Agents • Sulfonylureas: increases insulin production from the pancreas • Drug of choice in Type 2 Diabetes because of decreased chance of hypoglycemia o glipizide (Glucotrol, Glucatrol XL) o glyburide (Micronase, DiaBeta, Glynase) o glimiperide (Amaryl) Interacts with oral anticoagulants Oral Hypoglycemics (cont’d) • Biguanides: Primary action is to reduce glucose production by the liver o Metformin (Glucophage) • Can be used alone or with other oral agents or insulin to treat Type 2 Diabetes • Also used in prediabetics to prevent type 2 diabetes • Does not promote weight gain Cannot be taken with contrast dye! Oral Hypoglycemic Agents (cont’d) • a -Glucosidase Inhibitors: (starch blockers) work by slowing down absorption of carbohydrates in the small intestine o Acarbose (Precose) o Miglitol (Glyset) • Taken with first bite of each meal • Most effective in lowering post-prandial BGLs Oral Hypoglycemic Agents (cont’d) • Thiazolidinediones: a/k/a Insulin Sensitizers, work by improving insulin sensitivity, transport and utilization at target tissues o Pioglitazone (Actos) o Rosiglitazone (Avandia) • Most effective for people with insulin resistance Do not cause hypoglycemia because they don’t increase insulin production Can cause edema – do not use in patients with heart failure Diabetes Treatment The Priority Nursing Considerations for any diabetic patient on Insulin or oral Hypoglycemic agents is Monitor/prevent Hypoglycemia Hypoglycemia is an emergency and needs to be treated immediately Nutritional Therapy Type 1 Diabetes Mellitus Type 2 Diabetes Mellitus • Meal planning based on patient’s usual food intake • Balance with insulin and exercise programs • Plan is developed with the person’s eating habits and activity pattern in mind • Emphasis is based on achieving glucose, lipid and blood pressure goals • Reduce total fat, simple sugars, carbohydrates • Space Meals • Weight loss of even 5 – 7% can improve glycemic control Diabetes: Nutritional Therapy • The Cornerstone of Care for the patient with Diabetes The Goal (according to the ADA) is to assist people with diabetes to make good food choices and maintain healthy exercise habits that lead to: 1. 2. 3. 4. 5. Good Metabolic Control Maintain blood glucose levels at or near normal Achieve lipid profiles and BP levels Modify Lifestyle changes as appropriate Improve health through healthy food choices and physical activity Must address individual nutritional needs, personal and cultural preferences and respect the individual’s willingness to change Patient Teaching (Nutritional Tx) • Nurses often assume responsibilities of teaching • Ideally: Diabetic teacher or interdisciplinary diabetes care team • Include Patient’s family and significant others Culture Teach the person who does the cooking Caloric intake Patient Teaching: Exercise Therapy • Regular, consistent exercise is an essential part of diabetes and prediabetes management Exercise increases insulin receptor sites in the tissue and has a direct effect on lowering blood glucose levels Can also decrease triglycerides, LDL cholesterol Can increase HDL Can reduce blood pressure Can improve circulation Exercise Therapy (cont’d) • Exercise can lower BGLs to dangerously low levels Small carbohydrate snacks can be taken 1 hour before, 1 hour after exercise Patient should exercise and carry a fast acting carbohydrate • Exercise can also raise BGLs The body sometimes perceives the exercise as a stress Counterregulatory hormones released, raising BGLs • BGLs should be monitored before, during & after when beginning an exercise regimen, especially if the patient formerly led a sedentary lifestyle Monitoring Blood Glucose Levels • Self-Monitoring of Blood Glucose (SMBG) = a cornerstone of diabetes management • SMBG enables the patient to make selfmanagement decisions regarding Diet Exercise Medications • Important for detecting episodes of hyperglycemia and hypoglycemia • Teaching SMBG is an important nursing responsibility Pancreatic Transplant • Treatment option for Type 1 Diabetics with poorly controlled BGLs Rare, usually not done alone Can be done following kidney transplant to protect the new kidney from further damage from high BGLs Pancreas transplant only partially successful in reversing long-term damage Patient must take life-long immunosuppressants Hypoglycemia Diabetic Ketoacidosis (DKA) Hyperosmolar Hyperglycemic Syndrome (HHS) Hypoglycemia • Hypoglycemia occurs when there is too much insulin in proportion to available glucose in the blood . BGL drops to <70 Common Manifestations of hypoglycemia: Confusion Irritabililty Diaphoresis Tremors Hunger Weakness Visual Disturbances Hypoglycemia • The brain requires a constant supply of glucose in sufficient quantities to function properly, hypoglycemia can affect mental function • Manifestations of hypoglycemia can mimic alcohol intoxication • Untreated hypoglycemia can progress to loss of consciousness, seizures, coma, death Low Blood Glucose Levels • Hypoglycemia may also result if high glucose levels are treated too aggressively and brought down too quickly • It is important to ascertain why the BGL dropped Treatment of Hypoglycemia Conscious Patient Unconscious Patient Hypoglycemia is an emergency and needs to be treated immediately • Give the patient 15-20 grams of quick acting carbohydrate 4-6 oz Regular soda 8-10 Candies 4-6 oz Orange Juice • Repeat in 15 minutes if no improvement • Longer acting carbohydrate Crackers with peanut butter or cheese Immediate notification of health care provider especially if symptoms do not subside • Subcutaneous or IM injection of 1 mg Glucagon • IV administration of 50 mls of 50% Glucose Diabetic Ketoacidosis (DKA) • Also known as Diabetic Coma • Caused by: A profound deficiency of insulin and characterized by: hyperglycemia ketosis acidosis dehydration • Most likely to occur in Type 1 Diabetics, but sometimes occurs in Type 2 Diabetics during conditions of severe illness and/or stress Diabetic Ketoacidosis (cont’d) • Ketones are the acidic by-products of fat metabolism • Ketosis (presence of ketones in the blood) alters the Ph balance causing metabolic acidosis • Ketonuria begins – ketone bodies are excreted in the urine • The kidneys use more water to eliminate the ketones – causes dehydration • The existing insulin deficiency causes proteins to break down and stimulates production of glucose (in the liver) leading to worsening hyperglycemia Diabetic Ketoacidosis (cont’d) • The rise in glucose levels and lack of insulin make the blood glucose levels rise even further • With cell death, potassium is released from cell into the bloodstream -> hyperkalemia • Kidneys continue to excrete ketones – leading to a severe depletion of Potassium & other electrolytes Diabetic Ketoacidosis • Acidosis causes nausea & vomiting which results in severe hypovolemia, possibly shock • Renal failure results from hypovolemic shock (which causes retention of ketones & glucose and the acidosis progresses) Diabetes Ketoacidosis (cont’d) • Result: Patient becomes comatose as the result of dehydration, electrolyte imbalance and acidosis Coma Cardiac irregularities (due to hyperkalemia) Renal insufficiency Eventual death DKA: Clinical Manifestations • Dehydration- Early signs include: Poor Skin Turgor Dry mucous membranes Tachycardia Orthostatic Hypotension Lethargy, weakness • Severe Dehydration: Skin dry & loose Eyeballs soft, sunken DKA: Clinical Manifestations (cont’d) • Abdominal Pain accompanied by anorexia & vomiting • Kussmaul respirations (rapid, deep breathing associated with dyspnea) The body is attempting to reverse the metabolic acidosis through exhalation of excess Co2. Acetone noted on the breath Sweet, fruity breath odor Ketonuria Management • Correct dehydration • Correct electrolyte loss • Acidosis Hyperosmolar Hyperglycemic Syndrome • Formerly known as Hyperosmolar Hyperglycemic Non-Ketoacidosis (HHNK) • HHS is a life-threatening syndrome that can occur when the person is able to produce enough insulin to prevent DKA (and ketoacidosis) but not enough to prevent severe hyperglycemia, osmotic diuresis and extracellular fluid depletion. DKA vs. HHS (HHNK) • DKA usually Type 1 Diabetics • HHNK usually Type 2 Diabetics Seen more often in elderly with pre-existing cardiac or renal problems Usually patient can produce enough insulin to avoid ketoacidosis but not enough to prevent profound hyperglycemia, dehydration and hyperosmolality • Risk factors • Clinical picture Treatment DKA/HHS • IV Fluids • IV Insulin Rapid Acting Insulin Continual drip • Electrolyte Replacement • Assessment of Mental Status Safety • • • • • I & O’s Central Venous Pressure Monitoring (if indicated) Blood Glucose Levels ECG Monitoring Cardiovascular and Respiratory Status Macrovascular/Microvascular Complications Diabetic Retinopathy Nephropathy Neuropathy Complications of Feet & Lower Extremities Integumentary Complications Complications: Diabetes Mellitus Macrovascular Microvascular • Diseases of the large & medium size blood vessels • Exact cause unknown – related to the altered lipid metabolism -> atherosclerotic plaque formation Cerebrovascular Coronary Artery Peripheral Vascular • Diseases resulting from the thickening of the vessel membranes in the capillaries and arterioles in response to conditions of chronic hyperglycemia (Microangiopathy) Diabetic Retinopathy Diabetic Nephropathy Dermopathy o Diabetic Foot Ulcers Macrovascular Complications • Adults with Diabetes have 2-4 x increased risk of cerebrovascular and cardiovascular disease Genetic risk not modifiable Other risk factors can be modified (obesity, smoking, HTN, high fat intake, sedentary lifestyle) Blood Pressure Control significantly reduces the risk of microvascular complications Eye Kidney Nerves Diabetic Retinopathy • The process of microvascular damage to the retina as the result of chronic hyperglycemia in patients with diabetes • Subject to many visual complications • Assessment /Dx • Treatment: Photocoagulation (Laser) destroys the ischemic area producing the growth factors Vitrectomy: aspiration of fluid & fibers from the inside of the eye Diabetic Nephropathy • Definition: A microvascular complication associated with damage to the small blood vessels that supply the glomeruli of the kidney. • Leading cause of End Stage Renal Disease (ESRD) in the U.S. • Same risk, type 1 or type 2 Diabetics Diabetic Nephropathy (cont’d) • The risk for kidney disease in diabetics can be significantly reduced when blood glucose levels are closely controlled to near-normal levels Tight blood glucose control critical • ACE inhibitor (Angiotensin Converting Enzyme) medications sometimes prescribed for diabetics because of the protective effect they have on the kidneys Diabetic Neuropathy • 60-70% of diabetics have some form of neuropathy Occurs with equal frequency in Type 1 & Type 2 • Can lead to loss of (protective) sensation in lower extremities Increases risk of complications that result in amputation of lower limbs o More than 60% of non-traumatic amputations are diabetics Diabetic Neuropathy (cont’d) Sensory Neuropathy • Distal symmetric neuropathy Affects hands and/or feet bilaterally Loss of Sensation: Can be complete or partial loss of sensation Pain: burning, crushing Abnormal sensations Paresthesias Tingling, burning or itching Autonomic Neuropathy • Autonomic Neuropathy: Can affect all body systems and lead to hypoglycemic unawareness, constipation or diarrhea or urinary retention Gastroparesis Cardiovascular abnormalities • Sexual dysfunction often the first manifestation Decreased libido Erectile dysfunction Vaginal infection • Neurogenic Bladder Urinary retention Diabetic Neuropathy Management • diet high in sodium • avoid agents that stimulate ANS • wear elastic garments • frequent monitoring blood glucose • low-fat diet • increase gastric motility • anti-diarrhea medications • high fiber diet/hydration Diabetic Neuropathy Complications of the Feet & Lower Extremities • Foot complications = the most common cause of hospitalization of the person with diabetes • “Diabetic Foot” is the result of both microvascular and macrovascular disease processes which frequently leads to: Injury Serious Infection (Cellulitis) Amputation Feet & Lower Extremities (cont’d) • Multifactoral Process: The Two Major Causes of Diabetic Foot Ulcers are: 1. Sensory neuropathy causes Loss of Protective Sensation (LOPS) Patient is unaware of injury o o o Repetitive injury Stepping on foreign objects when barefoot Ill-fitting footwear 2. Peripheral Arterial Disease Causes a reduction in blood flow to lower extremities Wounds take longer to heal o Increases the risk for infection Diabetic Foot Ulcers Integumentary • Diabetic Dermatopathy Red-brown, flat-topped papules • Necrobiosis lipoidica diabeticorum May appear before other clinical signs & symptoms Foot /Leg Problems Risk factors • Diabetes for more than 10 years • Older than 40 years • History of smoking • Decreased peripheral pulses • Decreased sensation • History of previous foot ulcers Foot /Leg Problems • • • • • • Daily assessment of the feet Examine feet at least once a year Assess for neuropathy Proper bathing/drying/lubricating Closed - toed shoes/socks Protect feet from hot/cold