Diabetes in older adults
advertisement

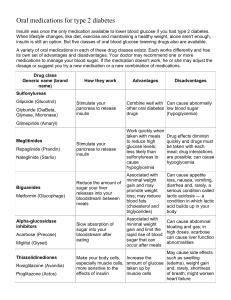
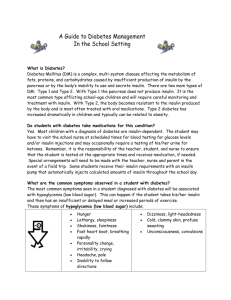
University of Alabama at Birmingham School of Medicine Diabetes Mellitus in Older Adults Fifteen percent of patients over 65 years have diabetes and approximately 20-30% of nursing home residents. More than 50% of diabetics are over 65 years. Diabetes may lead to admission at a younger age to long-term care facilities, secondary to visual loss or amputations. Criteria for diagnosing diabetes (i.e., a casual plasma glucose > 200mg/dl (11.1 mmol/l) or FPG>126mg/dl (7.0 mmol/l)) are not influenced by age. Routine use of oral glucose tolerance test (OGGT) is not recommended-especially in the geriatric population who may have a higher rate of impaired OGGT resulting in inconclusive results. HbA1C levels, which may be elevated with aging and some medical conditions such as chronic renal failure and hypoxia, should not be used in diagnosis.. The ‘classical’ symptoms may not be common in the elderly: Whereas a hyperosmolar state typically presents with polydipsia in the younger patient, more common symptoms and signs in elders are dehydration, confusion, delirium, obtundation , decreased visual acuity, weight loss and anorexia. Glycosuria may present with new urinary incontinence. Common complications observed in the older patient include: o Micro-and macro-vascular diseases (60% of all NIDDM mortality). o Ophthalmologic disease: cataracts, diabetic retinopathy. o Diabetic nephropathy. o Nervous system disorders: polyneuropathy, autonomic neuropathy (gastroparesis, postural hypotension), diabetic amyotrophy, cognitive impairment; o Metabolic disorders: hypoglycemia, hyperglycemia, hyperosmolar nonketotic coma. o Skin: diabetic or vascular ulcers, monilia. Hyperosmolar non-ketotic acidosis (HONKA) is the most severe metabolic complication of DM in older patients particularly in cognitively impaired individuals with long periods of uncontrolled hyperglycemia. DKA is less likely as the majority of older patients have some insulin production. Precipitants include: dehydration, infections, medical procedures, drugs (e.g., HCTZ, propranolol and steroids) and other acute medical conditions. Primary treatment is fluid resuscitation and lower insulin requirements than in DKA are observed. Older patients are at higher risk for hypoglycemia. Inappropriately high dosages of insulin and oral agents are the most common reason, but reduced creatinine clearances, which prolong the half-life of many drugs, and calorie intake contribute to hypoglycemia, as well. 1 University of Alabama at Birmingham School of Medicine Take visual acuity, cognitive status, functional condition and support systems into account when designing treatment regimens for older adults. Prevention of complications and functional preservation are important treatment goals. Caloric/protein restriction may not be appropriate for the older patient-50% of nursing home diabetics are underweight. Second-generation sulfonylureas are less likely to interfere with other medications and have fewer side effects. Glipizide is preferred over glyburide due to the latter’s tendency to cause serious hypoglycemia in older persons. Do not use metformin in patients over age 80 years and those with renal or liver disease; use caution in patients with heart failure. Calculate creatinine clearances using the Cockcroft-Gault equation and avoid metformin if it is <60-70ml/min. Thiazolidinediones (Avandia, Actos) should be avoided in patients with NYHA stage III or IV CHF and in seniors with liver disease. These agents usually do not cause hypoglycemia, but require bimonthly LFTs and are expensive. Not recommended as first line therapy. Alphaglucosidases (Acarbose, Migitol) can cause a lot of GI disturbance (e.g., flatus and diarrhoea) for a modest drop in glucose. Insulin: 1. Reserved for patients who fail to achieve glycemic control with an oral agent and diet. 2. Frequently a single daily dose can be used because insulin secretory capacity remains in most type II DM patients. 3. The starting dose should be individualized but usually 10units NPH in normal or low-weight individuals and 15 units in obese patients. Premixed insulin or the addition of regular insulin can be used for tighter control. 4. If blood glucose>300mg/dl and dehydration, hospitalization for control recommended. 5. Risk of hypoglycemia is present and must consider visual & motor skills & cognitive ability of patient and /or caregiver. 6. Although combination regimens (insulin+sulfonylureas/metformin) have been used in the middle-aged population there is no evidence for there use in the older patient and should in fact be avoided because of the additive risk of hypoglycemia. References 1. Endocrine and metabolic problems in Ouslander JG, Osterweil D, Morley J, eds. Medical Care in the Nursing Home: McGraw-Hill, NY, NY, 1997. 2. Halter JB. Diabetes mellitus in Hazzard WR, Blass JP, Ettinger WH, et al, eds. Principles of Geriatric Medicine and Gerontology, 4th ed: McGraw Hill, NY, NY, 1999. 2 University of Alabama at Birmingham School of Medicine 3. Mao CA. Diabetes mellitus in Forceia MA, Lavisso-Mourey R. Geriatric Secrets: Hanley and Belfus, Philadelphia, PA, 1996. 4. Reed RL, Mooradian AD. Diabetes mellitus in Ham RJ, Sloane PD, Warshaw GA, eds. Primary Care Geriatrics, 4th ed: Mosby, St. Louis, MO, 2002. 5. American Diabetes Association website. Supported by a grant from the Association of American Medical Colleges and the John A. Hartford Foundation. 3