Female Reproduction PPT - Northern Highlands Regional HS
advertisement

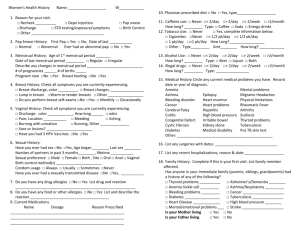
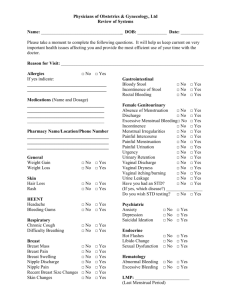
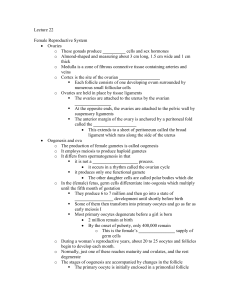
Human Sexuality and Family Life Unit 2 – Anatomy of the Female Reproductive System Puberty in Females •Pituitary gland release gonadotropic hormones – LH & FSH •Activate the female gonads which begins producing the female sex hormones estrogen & progesterone •Secondary sex characteristics begin – this can include budding of breasts, auxillary hair development, leading to menarche around age 13 – usually anovulatory (not ovulating) •Other changes as well KEY TERMS – Female Reproductive System External terms • Vulva – describes all external parts • Labia Majora –outer folds of skin • Labia Minora – inner folds - Both become sensitive • • • • • • during stimulation Clitoris – located in front of urethra – many blood vessels & nerve endings Urethra - connects to urethra -eliminates urine Vagina – opening to uterus – birth canal Perineum – field of tissue between vagina & anus Mons Pubis – pad of tissue covering pubic bone – some sensitivity – covered w/ pubic hair Hymen – membrane that sometimes covers vaginal opening Internal structures • Vagina –birth canal – about 3-4 inches deep – • • • nerve endings concentrated near opening Cervix – lower end of the uterus – located at top of canal Uterus – reproductive organ, located top of vagina between bladder & rectum – about size of a fist – sheds lining monthly as a part of the menstrual cycle Endometrium –lining of uterus – shed during cycle or supports fertilized egg during pregnancy Internal structures – cont. • Bartholin glands – located on sides of canal – release lubricant into canal • Fallopian tubes – egg travels down tube toward uterus – fertilization can take place in lower 1/3 of tube if sperm present • Fimbriae – fingers of f. tube – move toward gonads as ovulation takes place – scoops up ova • Ovaries – female gonads – house sex cell until mature in structure called “follicle”– females born with approx 1 million eggs – ovaries produce sex hormones Hormones • Estrogen- causes reproductive organs to mature into adult shape & size – growth of auxillary hair & strengthens bones • w/ progesterone – regulates the menstrual cycle a & preparing uterus for pregnancy • Ova – female sex cells – begin to mature around age 15 – released monthly during ovulation - Menstrual Cycle • Complex combination of hormonal & physical changes • Involves FSH & LH • Based on a 28 day cycle – can vary • Factors that can affect MC include stress, diet, travel, exercise, WT gain/loss, illness • Refer to MC chart for cycle Problems of Female Repo. System Problem What it is? Symptoms Treatment Cystitis Bladder infection Inflammation of bladder; usually due to bacterial infection Burning during urination; strong smell; fever or blood in urine Antibiotics Vaginitis Vaginal infection by fungus, bacteria, or protozoa; may be from STI Irritation or itchin around vagina; secretions of unusual color &/or unpleasant odor Over-the – counter vaginal cream or antibiotic Problem What it is? Symptoms Treatment Amenorrhea Late puberty due to anorexia, endocrine (Delayed problems, excessive puberty) wt. loss, &/or Over exercise No breast development, &/or no Menstrual periods Determined by doctor Menstrual Cramps Prostaglandins (hormone like substance) produced during menstruation causes cramps Contractions of uterine muscle, abdominal pain, some nausea/vomit Over-thecounter meds, warm baths, doctor Premenstrual Syndrome Mental & physical changes related to MC; not completely understood Irritability, mood swings, depression, abdominal bloating, breast tenderness doctor PMS Problem What it is? Symptoms Treatment Ovarian Cyst Failure of follicle to rupture & release an ova; may also be growths from cancer Pain in lower abdomen or pelvis for a month or so Mx by doctor; cysts often go away on own but may need surgery Cervical Cancer Abnormal division of cells in cervix; can be from STI Vaginal bleeding, discharge, pelvic pain, may be no symptoms Surgery, radiation, chemo Problem What it is? Symptoms Treatment Toxic Shock Syndrome (TSS) Poisoning of the body from bacterial toxins; usually related to tampon use Fever, chills, weakness, rash on palms of hands Antibiotics & immediate Mx treatment Endometriosis Growth of tissue from uterine lining outside the uterus Severe cramping and pain in lower abdomin or pelvis region MX – hormone therapy or surgery HEALTHY FRS •Women should practice good-hygiene, self- exams, regular MX visits •Balanced diet & exercise •Prevent STI’s – •Prevent vaginal irritation=reddenss, itching, mild pain around vaginal opening; prevent by reg. bathing, loose cotton underclothes, not wearing wet clothes for long periods of time, etc •Relieving menstrual cramps •Preventing infertility ---Annual pelvic exam • 7 Ways to Stay Healthy 1. Exercise regularly & maintain balanced diet 2. Gently wash genital area w/ warm water & 3. 4. 5. 6. 7. soap daily- do not use hygiene sprays/powders Wipe front to back after urination Change sanitary napkins every 4-6 hours Avoid wearing tight clothing that can cause discomfort Have annual pelvic exam Do monthly SBE Breast Cancer • • • • Mainly older women but can occur at any age At risk if it runs in the family but not the only factor Can be treated effectively if detected early WAYS TO CHECK – Mammogram – Self-breast exam - Perform BSE during/after warm bath/shower; & at least 1 week after period - Stand in front of mirror, place 1 hand over head & use other to examine each breast separately - Use your thumb/index finger to gently squeeze each nipple looking for unusual discharge - Check each nipple for swelling, dimpling, scaliness - Use 3 fingers to feel each breast for unusual lumps or thickening under skin. Check under armpits & breast as well EATING DISORDERS • American Psychological Association uses following diagnostic criteria to identify: Anorexia – – – – 15% or more below desirable weight Fear of weight gain Altered body image 3 or more missed menstrual periods; in young adolescents, no onset on menstruation Bulimia – Binge eating 2 or more times a week for 3 months – A lack of control over eating – Purging – Concern about body image Characteristic Symptoms • Anorexia – – – – – – Looks thin & keeps getting thinner Skips meals, cuts food into small pieces, moves food around plate Loss of menstrual period Wears layered clothing – loss of hair from head Growth of fine hair on face, arm Sensitive to cold Bulimia – Bathroom use immediately after eating – Inconspicuous eating – Excessive time/money spent food shopping – Menstrual irregularities – Excessive constipation – Swollen/infected glands, sore throat , bursting blood vessels in eyes, damaged teeth & gums – Dehydration EATING DISORDER TREATMENTS • • • • • • Anorexia Can be complex & demanding May include hospitalization to stabilize physical issues Intravenous feedings Drug treatments to treat depression, OCD, anxiety Counseling – individual & family • Bulimia includes family & nutritional counseling – hospitalization is not usually required • Where to get help – Guidance – Bergen County Dept. of Health – Health Professionals