NOTE:
This is Handout #1 of 2
Be sure to also print out Handout #2
January 10, 2011
Nursing 330
Human Reproductive Health
Office Hours
Turnitin
Mondays, 5:30pm – 6pm
Room TBA
Course ID: 3734705
Password: NURS330
Course packets
Course Website
Syllabus
Reading Assignments
Quarter Schedule
Evaluation Methods
Lecture Notes
Print out or download on to laptop
May be taken down at anytime so it is your
responsibility to print or download before each
lecture
Important Dates
Mid-term:
February 7, 2011
Essay Due: February 14, 2011
Electronically [Turnitin]
Hard Copy + Article [In Class]
Extra Credit Due: February 21, 2011
Final Exam: March 7, 2011
Puberty
Puberty
Not a synonym for adolescence
Defined as the biological state when
reproduction becomes possible
Refers to physical changes that occur during
adolescence
Puberty (cont)
Pubertal changes in girls begin between
ages 9 and 14.
Pubertal changes in boys generally begin
about 2 years later than in girls.
Physical occurrences from puberty
Growth Spurt
The primary sex characteristics develop
The secondary sex characteristics develop
Growth Spurt
1. Limbs
2. Body’s trunk
3. Shoulders and chest
Bones become harder and more dense
Muscle and fat contribute to an adolescent
increase in weight
Body Composition
Girls
Develop Breast
Acquire Hips
Higher fat to muscle
ratio
Boys
Wider shoulders
More muscular neck
Lose fat during
adolescence
Primary Sex Characteristics
Differences in male and female anatomy which
are present at birth
–ovaries and testes
Defined as the change necessary to prepare girls’
and boys’ bodies to produce children
Marker events
Girls
Boys
Menarche
Spermarche
As the primary sex organs mature, the secondary
sex characteristics distinguish males from females
Secondary Sex Characteristics
Defined as changes that make boys and
girls look like mature men and women
Girls
-Breast Development
-Body fat
-Body Odor
-Body Hair
Boys
-Voice Deepens
-Shoulders broaden
-Body Odor
-Body Hair
Tanner Classification of Sexual
Maturity
Puberty is divided into five stages, called
Tanner Stages (numbered 1-5). Each stage
represents the extent of breast, pubic and
genital hair growth.
Phases of Development - girls
Usual Age Range
Earliest Age
Latest Age
1. Beginning of
breast
development
8 – ¾ years
13 – ¼ years
11 years
2. Appearance of
pubic hair
9 years
13 ½ years
11 years
3. Beginning of
most rapid
growth
10 ½ years
14 ½ years
12 years
4. Menarche
10 ¾ years
15 ½ years
12 ½ years
2-3 years after
signs of puberty
1st
Approximate
Average Age
Phases of Development
- boys
Usual Age Range
Earliest Age
Latest Age
Approximate
Average Age
1. Beginning of
enlargement
of testes
9 ½ years
13 ½ years
12 years
2. Growth of the
penis
10 years
14 years
12 ¼ years
3. Appearance of
pubic hair
9 ½ years
14 years
12 ½ years
4. Beginning of
most rapid
growth in
height
11 ½ years
16 years
14 years
Nocturnal Emissions
Aka
Wet Dreams
Involuntary Orgasm
An ejaculation of semen experienced
during sleep
DISCUSSION QUESTION
Hormones
Estrogen
Responsible for many changes that occur during
puberty.
Cause the breasts, uterus, and vagina to mature and
the body to take feminine proportions
Contribute to regulation of the menstrual cycle
Testosterone
Responsible for changes of male puberty
Leads to muscle growth, body and facial hair, and
other male sex characteristics
Contributes to gains in body size
Sexual Anatomy &
Physiology
Female Sex Organs:
All embryos appear as female at first.
Genetic and hormonal signals trigger the
development of male organs in those
embryos destined to be male.
Sex organs serve a reproductive purpose,
but they perform other functions also:
giving pleasure, attracting sex partners, and
bonding in relationships.
Vulva
The external female genitals are known
collectively as the vulva. It includes:
Mons pubis
Clitoris
Clitoral Hood (or Prepuce)
Labia Majora
Labia Minora
Urethral Opening
Anus
Vulva (cont)
mons pubis is a pad of fatty tissue that covers the
area of the pubic bone.
clitoris is the center of sexual arousal in the female.
labia majora (outer lips) are two folds of spongy flesh
extending from the mons pubis and enclosing the
other external genitals.
labia minora (inner lips) are smooth, hairless folds
within the labia majora that meet above the clitoris.
Diagram of the Female Reproductive
System (external view)
Female Genital Mutilation (FGM)
aka Female Circumcision
What is it?
Types
Areas where it is practiced
What is FGM?
Types of FGM
Type I
excision of the prepuce, with or without
excision of part or all of the clitoris
Type II
excision of the clitoris with partial or total
excision of the labia minora
Types of FGM (cont)
Type III
Aka infibulation; the most extreme
excision of part or all of the external genitalia and
stitching/narrowing of the vaginal opening
Type IV
pricking, piercing or incising of the clitoris and/or
labia; stretching of the clitoris and/or labia;
cauterization by burning of the clitoris and
surrounding tissue
Where is FGM practiced?
Why is FGM practiced?
Internal Organs
The internal female sexual structures and
reproductive organs include:
Vagina
Uterus
Cervix
Ovaries
Fallopian tubes
The Vagina
A flexible muscular organ, approximately 3-4
inches long (in unaroused state) that has the
vaginal opening at one end and the cervix at the
other.
Purpose of the vagina:
Menstruation
Childbirth
Intercourse
The Vagina (cont)
Introitus or Vaginal Os
The opening of the vagina
Hymen
a thin, perforated membrane, that covers the introitus
prior to first intercourse or other intrusion.
a Greek word meaning "virginal membrane" or "thin
skin".
Cervix
Located between the vagina and the uterus
Cervical Os
Opening to the vagina
Allows menstrual blood to flow out of the
uterus into the vagina
Uterus
Also known as the womb
A pear-shaped organ located between the bladder and the
lower intestine
Consists of three parts
Body of the uterus (about the size of a fist in a non-pregnant
female)
Cervix
Fundus
Endometrium
Lining of the uterus
is built up and then shed and expelled through the cervical os
(opening) during menstruation.
Ovaries
Egg-producing organs
Hold between 200,000 and 400,000
follicles (sacks)
Found on each side of the uterus
Fallopian Tube
Also known as the Uterine Tube or Oviduct
Two leading off each side of the uterus
Site of fertilization
Diagram of the Female Reproductive
System (internal view)
Female Reproductive System
Use handout from course pack to identify:
Page 13
Anus
Bladder
Cervix
Fallopian tube
Ovary
Rectum
Urethra
Uterus
Vagina/Vaginal
Opening
G-Spot
Controversial
research has posited
the existence of an
erotically sensitive
area, the
Grafenberg spot
(G-spot), on the
front wall of the
vagina midway
between the
introitus and the
cervix.
Female Sexual Physiology
At birth, the human female’s ovaries contain
400,000-700,000 female gametes (sex cells).
During puberty hormones trigger the
completion of oogenesis, the production of
oocytes, commonly called eggs or ova.
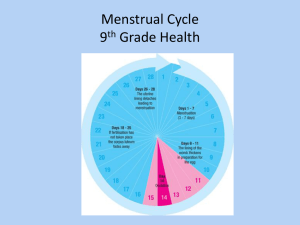
The Menstrual Cycle
Follicular (Proliferative) phase
Luteal (Secretory) phase
aka premenstrual phase
Days 1 through 6
Beginning of menstrual flow to end of blood flow
Days 7 – 13 endometrium thickens
Days 15 to 28
The endometrium thickens to prepare the egg for
implantation
These two phases are separated by:
Ovulation
Day 14
Ovulation
The process in the menstrual cycle by which a
mature ovarian follicle ruptures and releases an
ovum (also known as an egg or an oocyte)
The released egg, unless fertilized, only lasts 12
to 24 hours.
Menstrual Cycle
Order of the Menstrual Cycle:
Menstrual → Proliferative → Secretory
The menstrual cycle is divided into 3 phases.
1. Menstruation
2. Proliferative Phase: Endometrial tissue builds up
during this phase
3. Secretory Phase: Produces nutrients to sustain an
embryo
Menstrual Phases
Typical No. of Days
Hormonal Actions
Follicular (Proliferative)
Phase
Also known as
Pre-ovulatory phase
Cycle Days 1 through 6
Beginning of menstruation to end
of blood flow
Estrogen and progesterone start
out at their lowest levels
FSH levels rise to stimulate
maturity of follicles. Ovaries start
producing estrogen and levels
rise, while progesterone levels
remain low.
Cycle Days 7 -13: The
endometrium (the inner lining of
the uterus) thickens to prepare for
the egg implantation
Ovulation
Cycle Day 14
Surge in LH. Largest follicle
bursts and releases egg into
fallopian
Luteal (Secretory)
Phase
Also known as
Premenstrual phase
Cycle Days 15 – 28
Depends on whether fertilization
occurs or not.
Corpus Luteum
A mound of yellow tissue
Develops as a result of the ruptured follicle
During pregnancy, it serves to produce
estrogen and progesterone
If fertilization occurs,
Fertilized egg attaches to blanket of blood
vessels which supplies nutrients for the
developing placenta. Corpus luteum
continues to produce estrogen and
progesterone.
If fertilization does NOT occur:
Corpus luteum deteriorates. Estrogen and
progesterone levels drop. The blood vessel
lining sloughs off and menstruation begins.
Hormones
Hormones are chemical substances that
serve as messengers, traveling through the
bloodstream.
Hormones
Pituitary Hormones
Luteinizing Hormone (LH)
Follicle Stimulating Hormone (FSH)
Ovarian Hormomes
Estrogen
Progesterone
The Path of the Egg
Reaches uterus about 2-4 days after ovulation
Moves slowly toward uterus
Swept into fallopian tube
Released from follicle
The egg, unless fertilized, only survives 12-24 hours.
The Menstrual Cycle
PMS
Premenstrual syndrome (PMS) is a group
of symptoms related to the menstrual cycle
PMS
Physical and emotional disorder
Caused by hormonal changes
Widely recognized as a medical condition
85% of menstruating women have at least
one symptom
5-10% debilitating symptoms
Symptoms present two weeks before
menstruation
Remedies:
Dietary Recommendations
Low fat
High fiber
3 meals a day and 3 snacks containing starchy
foods
Drink plenty of water
Avoid caffeine
Low salt
High calcium
Menstrual Conditions
Two types
Amenorrhea
Dysmenorrhea
Amenorrhea
Primary
failure to start having a period by the age of 16
Secondary
temporary or permanent ending of periods in a woman who
has menstruated normally in the past
Menstrual Disorders (Cont)
Dysmenorrhea - Painful menstrual periods (aka
cramps)
Primary
no physical abnormality and usually begins within
three years after you begin menstruating
Secondary
involves an underlying physical cause, such as
endometriosis or uterine fibroids
Discussion Question: