Chapter 3
advertisement
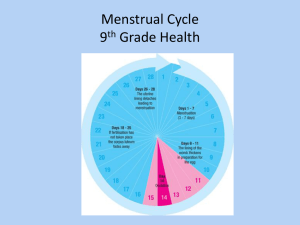
NOTE: This is Handout #1 of 2 Be sure to also print out Handout #2 April 9, 2012 Nursing 330 Human Reproductive Health Office Hours Turnitin Mondays, 5:30pm – 6pm Room TBA Class ID: 5011311 Password: NURS330 Course Packets Course Website Syllabus Reading Assignments Essay Extra Credit Quarter Schedule Lecture Notes Print out or download on to laptop May be taken down at anytime so it is your responsibility to print or download before each lecture Essay Reproductive Health issue in a current mainstream newspaper or magazine article (journal articles are not acceptable) 50 points Due 5/147/12 ( Turnitin –AND- In Class) Article Should be dated between March 1, 2012 – May 14, 2012 Bring articles to class for approval (4/9/12 – 5/7/12) Essay (cont) Sample topics: Puberty, Menopause, Male Climacteric Syndrome, Cancer – breast, cervical, testicular, prostate, Rape, Sex Education, Abortion, Female Genital Mutilation, Pregnancy, STDs & HIV, Infertility, Breast Feeding, Contraception, Population Control, Same Sex Marriages, Sexuality. If you have other topics not listed here, submit it to the instructor for review and approval Answer specific questions Refer to course website for detailed assignment instructions Extra Credit (EC) Up to 25 points To be done throughout the quarter May only submit one EC per lecture Last day to submit EC: 5/21/12 Extra Credit (cont) Five Options 5. Reproductive Health Exam/STD screening – 15 points 5K/10K Health Walk/Run/Bike Ride– 15 points Volunteer Work – 10 points Attend a Workshop – 10 points Humor – 5 points May only complete one option once 1. 2. 3. 4. Important Dates Mid-term: April 30, 2012 Essay Due: May 14, 2012 Electronically [Turnitin] Hard Copy + Article [In Class] Extra Credit Due: May 21, 2012 Final Exam: June 11, 2012 Announcements Course syllabus updated Now includes detailed information about in-class assignment Be sure to use/print this updated version As explained during lecture last week, In class assignments are open book assignments, completed in class only. They cannot be taken outside the classroom or after the class time during which they are assigned. Students who miss an in-class assignment may use extra credit work to make up those points. IMPORTANT NURS 330 covers a variety of topics related to the Human Reproductive Health. Students are expected to be sensitive and mature in their discussions, questions and mannerisms. Any personal information disclosed by students in the class is considered confidential and should not be repeated outside the classroom. I reserve the right to eliminate any person, from the class, who I deem disruptive at any time. Puberty Puberty Not a synonym for adolescence Defined as the biological state when reproduction becomes possible Refers to physical changes that occur during adolescence Puberty (cont) Pubertal changes in girls begin between ages 9 and 14. Pubertal changes in boys generally begin about 2 years later than in girls. Physical occurrences from puberty Growth Spurt The primary sex characteristics develop The secondary sex characteristics develop Growth Spurt 1. Limbs 2. Body’s trunk 3. Shoulders and chest Bones become harder and more dense Muscle and fat contribute to an adolescent increase in weight Body Composition Girls Develop Breast Acquire Hips Higher fat to muscle ratio Boys Wider shoulders More muscular neck Lose fat during adolescence Primary Sex Characteristics Differences in male and female anatomy which are present at birth –ovaries and testes Defined as the change necessary to prepare girls’ and boys’ bodies to produce children Marker events Girls Boys Menarche Spermarche As the primary sex organs mature, the secondary sex characteristics distinguish males from females Secondary Sex Characteristics Defined as changes that make boys and girls look like mature men and women Girls -Breast Development -Body fat -Body Odor -Body Hair Boys -Voice Deepens -Shoulders broaden -Body Odor -Body Hair Phases of Development - girls Usual Age Range Earliest Age Latest Age 1. Beginning of breast development 8 – ¾ years 13 – ¼ years 11 years 2. Appearance of pubic hair 9 years 13 ½ years 11 years 3. Beginning of most rapid growth 10 ½ years 14 ½ years 12 years 4. Menarche 10 ¾ years 15 ½ years 12 ½ years 2-3 years after signs of puberty 1st Approximate Average Age Phases of Development - boys Usual Age Range Earliest Age Latest Age Approximate Average Age 1. Beginning of enlargement of testes 9 ½ years 13 ½ years 12 years 2. Growth of the penis 10 years 14 years 12 ¼ years 3. Appearance of pubic hair 9 ½ years 14 years 12 ½ years 4. Beginning of most rapid growth in height 11 ½ years 16 years 14 years Nocturnal Emissions Aka Wet Dreams Involuntary Orgasm An ejaculation of semen experienced during sleep Hormones Estrogen Responsible for many changes that occur during puberty. Cause the breasts, uterus, and vagina to mature and the body to take feminine proportions Contribute to regulation of the menstrual cycle Testosterone Responsible for changes of male puberty Leads to muscle growth, body and facial hair, and other male sex characteristics Contributes to gains in body size Sexual Anatomy & Physiology Female Sex Organs: All embryos appear as female at first. Genetic and hormonal signals trigger the development of male organs in those embryos destined to be male. Sex organs serve a reproductive purpose, but they perform other functions also: giving pleasure, attracting sex partners, and bonding in relationships. Vulva The external female genitals are known collectively as the vulva. It includes: Mons pubis Clitoris Clitoral Hood (or Prepuce) Labia Majora Labia Minora Urethral Opening Anus Vulva (cont) mons pubis is a pad of fatty tissue that covers the area of the pubic bone. clitoris is the center of sexual arousal in the female. labia majora (outer lips) are two folds of spongy flesh extending from the mons pubis and enclosing the other external genitals. labia minora (inner lips) are smooth, hairless folds within the labia majora that meet above the clitoris. Female Genital Mutilation (FGM) aka Female Circumcision What is it? Types Areas where it is practiced What is FGM? Types of FGM Type I excision of the prepuce, with or without excision of part or all of the clitoris Type II excision of the clitoris with partial or total excision of the labia minora Types of FGM (cont) Type III Aka infibulation; the most extreme excision of part or all of the external genitalia and stitching/narrowing of the vaginal opening Type IV pricking, piercing or incising of the clitoris and/or labia; stretching of the clitoris and/or labia; cauterization by burning of the clitoris and surrounding tissue Where is FGM practiced? Over 28 African countries Parts of the Middle East Parts of Asia Internal Organs The internal female sexual structures and reproductive organs include: Vagina Uterus Cervix Ovaries Fallopian tubes The Vagina A flexible muscular organ, approximately 3-4 inches long (in unaroused state) that has the vaginal opening at one end and the cervix at the other. Purpose of the vagina: Menstruation Childbirth Intercourse The Vagina (cont) Introitus or Vaginal Os The opening of the vagina Hymen a thin, perforated membrane, that covers the introitus prior to first intercourse or other intrusion. a Greek word meaning "virginal membrane" or "thin skin". Cervix Located between the vagina and the uterus Cervical Os Opening to the vagina Allows menstrual blood to flow out of the uterus into the vagina Uterus Also known as the womb A pear-shaped organ located between the bladder and the lower intestine Consists of three parts Body of the uterus (about the size of a fist in a non-pregnant female) Cervix Fundus Endometrium Lining of the uterus is built up and then shed and expelled through the cervical os (opening) during menstruation. Ovaries Egg-producing organs Hold between 200,000 and 400,000 follicles (sacks) Found on each side of the uterus Fallopian Tube Also known as the Uterine Tube or Oviduct Two leading off each side of the uterus Site of fertilization G-Spot Controversial research has posited the existence of an erotically sensitive area, the Grafenberg spot (G-spot), on the front wall of the vagina midway between the introitus and the cervix. Female Sexual Physiology At birth, the human female’s ovaries contain 400,000-700,000 female gametes (sex cells). During puberty hormones trigger the completion of oogenesis, the production of oocytes, commonly called eggs or ova. The Menstrual Cycle Follicular (Proliferative) phase Luteal (Secretory) phase aka premenstrual phase Days 1 through 6 Beginning of menstrual flow to end of blood flow Days 7 – 13 endometrium thickens Days 15 to 28 The endometrium thickens to prepare the egg for implantation These two phases are separated by: Ovulation Day 14 Ovulation The process in the menstrual cycle by which a mature ovarian follicle ruptures and releases an ovum (also known as an egg or an oocyte) The released egg, unless fertilized, only lasts 12 to 24 hours. Menstrual Cycle Order of the Menstrual Cycle: Menstrual → Proliferative → Secretory The menstrual cycle is divided into 3 phases. 1. Menstruation 2. Proliferative Phase: Endometrial tissue builds up during this phase 3. Secretory Phase: Produces nutrients to sustain an embryo Menstrual Phases Typical No. of Days Hormonal Actions Follicular (Proliferative) Phase Also known as Pre-ovulatory phase Cycle Days 1 through 6 Beginning of menstruation to end of blood flow Estrogen and progesterone start out at their lowest levels FSH levels rise to stimulate maturity of follicles. Ovaries start producing estrogen and levels rise, while progesterone levels remain low. Cycle Days 7 -13: The endometrium (the inner lining of the uterus) thickens to prepare for the egg implantation Ovulation Cycle Day 14 Surge in LH. Largest follicle bursts and releases egg into fallopian Luteal (Secretory) Phase Also known as Premenstrual phase Cycle Days 15 – 28 Depends on whether fertilization occurs or not. Corpus Luteum A mound of yellow tissue Develops as a result of the ruptured follicle During pregnancy, it serves to produce estrogen and progesterone If fertilization occurs, Fertilized egg attaches to blanket of blood vessels which supplies nutrients for the developing placenta. Corpus luteum continues to produce estrogen and progesterone. If fertilization does NOT occur: Corpus luteum deteriorates. Estrogen and progesterone levels drop. The blood vessel lining sloughs off and menstruation begins. Hormones Hormones are chemical substances that serve as messengers, traveling through the bloodstream. Hormones Pituitary Hormones Luteinizing Hormone (LH) Follicle Stimulating Hormone (FSH) Ovarian Hormomes Estrogen Progesterone The Path of the Egg Reaches uterus about 2-4 days after ovulation Moves slowly toward uterus Swept into fallopian tube Released from follicle The egg, unless fertilized, only survives 12-24 hours. PMS Premenstrual syndrome (PMS) is a group of symptoms related to the menstrual cycle PMS Physical and emotional disorder Caused by hormonal changes Widely recognized as a medical condition 85% of menstruating women have at least one symptom 5-10% debilitating symptoms Symptoms present two weeks before menstruation Remedies: Dietary Recommendations Low fat High fiber 3 meals a day and 3 snacks containing starchy foods Drink plenty of water Avoid caffeine Low salt High calcium Menstrual Conditions Two types Amenorrhea Dysmenorrhea Amenorrhea Primary failure to start having a period by the age of 16 Secondary temporary or permanent ending of periods in a woman who has menstruated normally in the past Menstrual Disorders (Cont) Dysmenorrhea - Painful menstrual periods (aka cramps) Primary no physical abnormality and usually begins within three years after you begin menstruating Secondary involves an underlying physical cause, such as endometriosis or uterine fibroids