Fluid and Electrolytes
advertisement

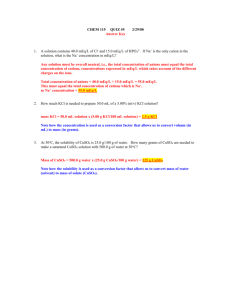
Serum Electrolytes & Arterial blood gases Dr. Mohammed K. El-Habil MSC. Pharmacology 2014 Electrolytes Solutes that form ions (electrical charge) Cation (+) Anion (-) Major body electrolytes: Na+, K+, Ca++, Mg++ Cl-, HCO3-, HPO4--, SO4- Electrolyte Distribution Major ICF ions K+ HPO4-- Major ECF ions NA+ CL-, HCO3- Electrolyte Normal Values Sodium Potassium Phosphrus Chloride Calcium Urea Creatinine Magnesium: CO2 Bicarbonate 135 – 145 mEq/L 3.5 – 5 mEq/L 1.8-2.3 mEq/L 98 – 106 mEq/L 9 – 11 mEq/L 20 – 40 mEq/L 0.7 – 1.2 mEq/L 1.5 – 3 mEq/L 22 – 26 mEq/L 24-30 mEq/L Hypernatremia Na+ is more than 135 – 145 mEq/L Manifestations Thirst, lethargy, agitation, seizures, and coma, shrinking of brain. Similar to : Central or nephrogenic diabetes insipidus (DI). In treatment, reduce Na+ levels gradually to avoid cerebral edema Hyponatremia Results from loss of sodium-containing fluids Sweat, diarrhea, emesis,..etc. Or from water excess Inefficient kidneys Drowning, excessive intake Manifestations Confusion, nausea, vomiting, seizures, Brain edema and coma Hyperkalemia Serum Potassium greater than 5.5 mEq/L - More dangerous than hypokalemia because cardiac arrest is frequently associated with high serum K+ levels Hyperkalemia Manifestations Weak or paralyzed skeletal muscles Ventricular fibrillation or cardiac block Abdominal cramping or diarrhea Hypokalemia Low serum potassium caused by Abnormal losses of K+ via the kidneys or gastrointestinal tract Drugs: Diuretics Magnesium deficiency Metabolic alkalosis enhance H-K pumping & entrance of K intracellular . Hypokalemia Manifestations Most serious are cardiac arrhythemias Skeletal muscle weakness Weakness of respiratory muscles Decreased gastrointestinal motility Calcium Obtained from ingested foods More than 99% combined with phosphorus and concentrated in skeletal system Inverse relationship with phosphorus Otherwise… Calcium Balance controlled by Parathyroid hormone Calcitonin Vitamin D/Intake Bone used as reservoir Hypercalcemia High serum calcium levels more than 9 – 11 mEq/L caused by Hyperparathyroidism (two thirds of cases) Malignancy (parathyroid tumor) Vitamin D overdose Prolonged mobilization Hypercalcemia Manifestations Decreased memory Confusion Disorientation Fatigue Constipation Treatment Excretion of Ca with loop diuretic Hydration with isotonic saline infusion Synthetic calcitonin Hypocalcemia Low serum Ca levels caused by Decreased production of PTH Acute pancreatitis Multiple blood transfusions Alkalosis Decreased intake Hypocalcemia Manifestations Weakness/Tetany Positive Trousseau’s or Chvostek’s sign Laryngeal stridor Dysphagia Tingling around the mouth or in the extremities Treatment Treat cause Oral or IV calcium supplements Not IM to avoid local reactions Treat pain and anxiety to prevent hyperventilation-induced respiratory alkalosis Phosphate Primary anion in ICF Essential to function of muscle, red blood cells, and nervous system Deposited with calcium for bone and tooth structure Hyperphosphatemia High serum PO43 (more than1.8-2.3 mEq/L) caused by: Acute or chronic renal failure Chemotherapy Excessive ingestion of phosphate or vitamin D Manifestations Calcified deposition: joints, arteries, skin, kidneys, and corneas Neuromuscular irritability and tetany Hypophosphatemia Low serum PO43 caused by Malnourishment/malabsorption Alcohol withdrawal Use of phosphate-binding antacids During parenteral nutrition with inadequate replacement Hypophosphatemia Manifestations CNS depression Confusion Muscle weakness and pain Dysrhythmias Cardiomyopathy Magnesium 50% to 60% contained in bone Coenzyme in metabolism of protein and carbohydrates Factors that regulate calcium balance appear to influence magnesium balance. Acts directly on myoneural junction Important for normal cardiac function Hypermagnesemia High serum Mg more than 1.5 – 3 mEq/L caused by When renal insufficiency or failure is present Manifestations Lethargy or drowsiness Nausea/vomiting Impaired reflexes*** Respiratory and cardiac arrest Hypomagnesemia Manifestations Confusion Hyperactive deep tendon reflexes Tremors Seizures Cardiac dysrhythmias Electrolytes Electrolytes Renal Function Arterial blood gases Interpretation of ABGs Diagnosis in six steps Evaluate pH Analyze PaCO2 Analyze HCO3 Determine if Balanced or Unbalanced Determine if CO2 or HCO3 matches the alteration Decide if the body is attempting to compensate Interpretation of ABG 1. 2. 3. 4. 5. pH over balance PaCO2 = “respiratory” balance HC03- = “metabolic” balance If all three normal = balanced Match direction. e.g., if pH and PaCO2 are both acidotic, then primary respiratory acidosis 6. Together, CO2 & HCO3 act as metabolic & respiratory buffer like: 7. H2O + CO2 ˭ ˭ ˭ H2CO3 ˭ ˭ ˭ HCO3 + H Metabolic Acid-base Disorders: Some Clinical Causes METABOLIC ACIDOSIS ↓HCO3- & ↓ pH - lactic acidosis; ketoacidosis; drug poisonings (e.g., aspirin, ethylene glycol, methanol) diarrhea; some kidney problems (e.g., renal tubular acidosis, interstitial nephritis) METABOLIC ALKALOSIS ↑ HCO3- & ↑ pH contraction alkalosis, diuretics, corticosteroids, gastric suctioning, vomiting hyperaldosterone state (e.g., Cushing’s syndrome, Bartter’s syndrome, severe K+ depletion) Respiratory Acid-base Disorders: Some Clinical Causes RESPIRATORY ACIDOSIS ↑PaCO2 & ↓ pH Central nervous system depression (e.g., drug overdose) Chest bellows dysfunction (e.g., Guillain-Barré syndrome, myasthenia gravis) Disease of lungs and/or upper airway (e.g., chronic obstructive lung disease, severe asthma attack, severe pulmonary edema) RESPIRATORY ALKALOSIS ↓PaCO2 & ↑ pH Hypoxemia (includes altitude) Anxiety Sepsis Any acute pulmonary insult (e.g., pneumonia, mild asthma attack, early pulmonary edema, pulmonary embolism) Acid-Base Disorders Acid-Base Disorders Interpretation of ABGs pH 7.26 Normal (7.35-7.45) PaCO2 67 mm Hg (35-45) PaO2 47 mm Hg (80-100) HCO3 26 mEq/L (22-26) What is this? Respiratory acidosis Interpretation of ABGs pH 7.18 PaCO2 38 mm Hg PaO2 70 mm Hg HCO3 15 mEq/L What is this? Metabolic acidosi