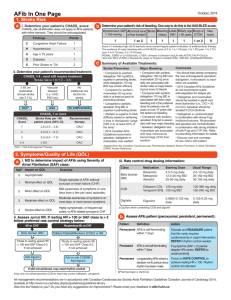
Section II: Clinical Management of AFib
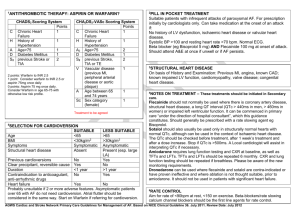
advertisement

Section II: Clinical Management of AFib Section II. Clinical Management of AFib 1. Clinical Evaluation of AFib 2. Treatment Options for AFib • Cardioversion • Drugs to prevent AFib • Drugs to control ventricular rate • Drugs to reduce thromboembolic risk • Non-pharmacological options 1. Clinical Evaluation of AFib Clinical Evaluation • Minimum – History and Physical examination – Electrocardiogram – Trans-thoracic echocardiogram – Blood tests of thyroid, renal and hepatic function • Discretionary – Six-minute walk test – Exercise testing – Holter monitoring or event recording – Trans-oesophageal echocardiography – Electrophysiological study – Chest radiograph ACC/AHA/ESC 2006 Guidelines for the Management of Patients With Atrial Fibrillation J Am Coll Cardiol (2006) 48: 854 Opportunistic Case Finding • In patients presenting with symptoms commonly associated with AFib: – breathlessness/dyspnoea – palpitations – syncope/dizziness – chest discomfort • Manual pulse palpation should be performed to determine the presence of an irregular pulse that may indicate underlying AFib NICE recommendation: Developed by National Collaborating Centre for Chronic Conditions at the Royal College of Physicians; Atrial fibrillation: full guideline DRAFT (January 2006) Primary Therapeutic Aims in AFib • Restore and maintain sinus rhythm whenever possible • Prevent thromboembolic events In order to: – Reduce symptoms and improve QoL – Minimize impact of AFib on cardiac performance – Reduce risk of stroke – Minimize cardiac remodeling ACC/AHA/ESC 2006 Guidelines for the Management of Patients With Atrial Fibrillation J Am Coll Cardiol (2006) 48: 854 2. Treatment Options for AFib Treatment Options for AFib Cardioversion • Pharmacological • Electrical Drugs to prevent AFib • Antiarrhythmic drugs • Non-antiarrhythmic drugs Drugs to control ventricular rate Drugs to reduce thromboembolic risk Non-pharmacological options • Electrical devices (implantable pacemaker and defibrillator) • AV node ablation and pacemaker implantation (ablate & pace) • Catheter ablation • Surgery (Maze, mini-Maze) Treatment Options for AFib Cardioversion Cardioversion of AFib • Pharmacological – Early onset AFib – Long-standing AFib • Electrical – Transthoracic Cardioversion of AFib Prompt treatment essential • Limit duration to minimize cardiac remodelling • Avoid anticoagulation therapy – (necessary for arrhythmias that last >48 hours) • Avoid prolonged hospital recovery • Improve quality of life Pharmacological Cardioversion Pharmacological Cardioversion • More effective in recent-onset AFib – Class IA-IC-III drugs administered IV – Class IC favoured in non-cardiopathic patients – Class III favoured in cardiopathic patients or those with delays in conduction • Oral loading can be performed with class IC drugs – Flecainide (200-300 mg) – Propafenone (450-600 mg) Pharmacological Cardioversion Recent onset AFib Oral Loading with Class IC Drugs for Recent Onset AFib 100 Flecainide 300 mg Propafenone 600 mg p<0.001 vs. placebo SR (%) p<0.001 vs. placebo 78 80 60 Placebo 72 59 51 39 40 18 20 0 3 hours 8 hours Capucci A, et al. Am J Cardiol (1994) 74: 503 Cardioversion of Paroxysmal AFib with Class IC Drugs Paroxysmal AFib (<48h), good LVEF Class IC drugs (propafenone, flecainide) • IV 2 mg/kg + 0.007 mg/kg/min, maintenance • Oral administration • Mean efficacy: flecainide 300 mg propafenone 600 mg 80% • Mean time of efficacy: 3h • Proarrhythmia: FLA 1:1 ECG monitoring necessary (<0.5%) with patients in resting condition Risk with Class IC Drugs: Transformation of AFib into Atrial Flutter with 1:1 AV Conduction Flecainide Treatment Out-of-Hospital with Class IC Drugs • Symptomatic, rare episodes of AFib • Recent onset AFib • No structural heart disease • Prior hospital experience • Good physician-patient relationship • Resting conditions for at least 4 hours Pill-in-the-Pocket • In a selected (no or mild HD), risk-stratified patient population with recurrent AFib not currently taking AADs – 79% developed ≥ 1 episodes of recurrent AFib during 15 ± 5m follow-up – Acute oral flecainide or propafenone successfully terminated 94% of episodes within 113 ± 84 min, with side effects in 7% of patients Alboni P, et al. N Engl J Med (2004) 351: 2384 Pill-in-the-Pocket Prior to enrolment 45.6 50 p<0.001 Number per month Number per month 50 During follow-up 25 25 15 4.9 0 p<0.001 1.6 0 Calls to ER Hospitalisation Alboni P, et al. N Engl J Med (2004) 351: 2384 Conversion to SR with Amiodarone IV (randomized studies) Control drug n Cowan et al Digoxin IV Hou et al Duration of study OR of SR with amiodarone p 34 24 h 1.11 NS Digoxin IV 50 24 h 1.30 0.0048 Cotter et al Placebo 80 24 h 1.34 0.029 Galve et al Placebo 100 24 h 1.13 0.532 Donovan et al Placebo 64 24 h 1.05 NS Donovan et al Flecainide 66 24 h 0.86 NS Nos et al Verapamil 24 3h 77% amiod./ 0% verap <0.001 McAlister et al Quinidine 36 8h 0.64 0.04 Pilati et al Quinidine 75 24 h 1.09 NS Kerin et al Quinidine 32 24 h 1.07 NS Di Biasi et al Propafenone 40 24 h 1.15 NS Larbuisson et al Propafenone 84 24 h 1.22 NS Chapman et al Procainamide 26 12 h 0.99 NS Magnesium sulfate 42 24 h 0.64 <0.05 Moran et al Primary endpoint Conversion to sinus rhythm Connolly SJ Circulation (1999) 100: 2025 Amiodarone for Cardioversion of Recent-Onset AFib: Meta-analysis 100 Bolus only Bolus + infusion 95 • Amiodarone IV (3-7 mg/kg ± infusion 0.9-3.0 g/day) 80 • Amiodarone oral (25-30 mg/kg) Conversion (%) 69 • Time to conversion > 6-8 h 55 60 • Amiodarone > 1.5 g/day IV > 40 placebo 34 • Amiodarone 25-30 mg/kg oral > placebo 20 • Amiodarone not > other AADs 0 2-4 h 8h • Safe in patients with structural cardiopathies and low LVEF Khan IA, et al. Int J Cardiol (2003) 89: 239 Amiodarone Single Oral Administration for Cardioversion of Recent Onset AFib Placebo Amiodarone 100 Patients in AFib (%) 80 60 40 20 0 0 2 4 6 8 10 12 14 16 18 20 22 24 26 Time to conversion (hours) Peuhkurinen K, et al. Am J Cardiol (2000) 85: 462 Flecainide IV vs Amiodarone IV for Cardioversion in Recent-Onset AFib Amiodarone Flecainide Placebo 32 28 Cardioversion (%) p=0.001 p=0.007 24 20 16 12 8 4 0 0 1 2 3 4 5 6 7 8 (hours) Donovan KD, et al. Am J Cardiol (1995) 75: 693 Pharmacological Cardioversion Long-lasting AFib Effect of Duration on Efficacy of Pharmacological Cardioversion 106 patients with AFib <6 months 100 Flecainide Sotalol * p=0.005 80 69* 60 52* 44 40 31 23 17 20 0 0 Total <24 hours <7 days 0 <6 months Reisinger J, et al. Am J Cardiol (1998) 81: 1450 Amiodarone Cardioversion in Persistent AFib 67 patients with AFib >48 hours A 100 B Amiodarone Placebo p<0.001 82 77 Sinus rhythm (%) 80 65 60 48 40 32 31 30 20 0 0 Total LA (mm) >45 <45 LVEF (%) >50 <50 AFib (m) >1 <1 Kochiadakis GE, et al. Am J Cardiol (1999) 83: 61 Conversion of Atrial Flutter or AFib with Ibutilide IV 266 patients 100 100 p<0.0001 80 Sinus rhythm (%) Sinus rhythm (%) 80 p<0.0001 60 40 60 40 20 20 0 0 Ibutilide Placebo AFlutter AFib Adverse effects: 8.3% polymorphic ventricular tachycardia Stambler BS, et al. Circulation (1996) 94: 1613 Conversion of Atrial Flutter or AFib with Ibutilide IV Effect “on top” of long-term amiodarone 70 patients (57 AFib, 13 AFlutter) Ibutilide 2 mg Recovery of SR (%) 80 60 54 39 40 20 0 AFlutter AFib Glatter K, et al. Circulation (2001) 103: 253 Electrical Cardioversion (transthoracic) Technical Aspects The efficacy of electrical cardioversion depends on the density of current delivered to the atrial myocardium, which is dependent on: • Impedence • Position of paddles • Pressure applied to paddles • Waveform • Transthoracic Cardioversion of Atrial Fibrillation Comparison of Rectilinear Biphasic vs Damped Sine Wave Monophasic Shocks Suneet Mittal, Shervin Ayati, Kenneth M. Stein, David Schwartzman, Doris Cavlovich, Patrick J. Tchou, Steven M. Markowitz, David J. Slotwiner, Marc A. Scheiner, Bruce B. Lerman. Circulation 2000; 101: 1282-7 Defibrillation Waves Monophasic wave Biphasic wave 30 Ampere Ampere 10 20 0 10 -10 0 0 4 8 msec 12 0 4 8 12 msec Mittal S, et al. Circulation (2000) 101: 1282 Cumulative Efficacy of Cardioversion Monophasic or biphasic shock p<0.005 p<0.0001 100 Efficacy of cardioversion (%) 85 91 94 79 80 68 68 60 44 40 21 20 0 100 J 200 J 300 J Monophasic 360 J 70 J 120 J 150 J 170 J Biphasic Mittal S, et al. Circulation (2000) 101: 1282 • Biphasic vs Monophasic Shock Waveform for Conversion of Atrial Fibrillation The Results of an International Randomized, Double-Blind Multicenter Trial RL Page, RE Kerber, JK Russel, T Trouton, J Waktare, D Gallik, JE Olgin, P Ricard, GW Dalzell, R Reddy, R Lazzara, K Lee, M Carlson, B Halperin, GH Bardy, for the BiCard Investigators. JACC (2002) 39: 1956-63 Dermal Injury Dependent on Waveform 60 Monophasic Biphasic 50 40 30 20 10 0 None (no erythema) Mild (no tenderness) Moderate (tenderness) Severe (blistering) Page RL, et al. J Am Coll Cardiol (2002) 39: 1956 Success of Monophasic (MP) and Biphasic (BP) Waveforms at Cumulative Energy Levels Adgey AA & Walsh SJ Heart (2004) 90: 1493 Success of Cumulative Shocks for Different Biphasic Devices Adgey AA & Walsh SJ Heart (2004) 90: 1493 Electrical Cardioversion Pharmacological pretreatment and management of recurrence Failure of Electrical Cardioversion 100 No conversion Immediate recurrent AFib Early recurrent AFib Late recurrence AFib 90 Sinus rhythm (%) 80 70 60 50 40 30 20 10 0 2 min 2 weeks 1 year cardioversion Van Gelder IC, et al. Am J Cardiol (1999) 84: 147R Recurrence Following Cardioversion: AFFIRM Study AFFIRM:most recurrences occur within 2 months of cardioversion Patients with AF Recurrence (%) Treatment Arm 100 Rate control Rhythm control 80 60 40 Log rank statistic = 58.62 p<0.0001 20 0 0 1 2 4 5 6 10,481 (92) 73,494 (75) 2,484 (95) 18,503 (79) Time (years) N, Events (%) Rate control: Rhythm control: 3 563,3 (0) 729,2 (0) 167,383 (69) 344,356 (50) 96,440 (80) 250,422 (60) 42,472 (87) 143,470 (69) Raitt MN, et al. Am Heart J (2006) 151: 390 Immediate Recurrence of AFib Following Successful Electrical Cardioversion Immediate/Early Recurrence of AFib After Electrical Cardioversion Authors n ERAF (%) Timing Bertaglia 90 28 7 days Bianconi 96 18 24 hours Botto 156 61 7 days Daoud 337 9 5 min De Simone 107 14 7 days 61 36 5 days 116 7 24 hours 50 26 1 min Tieleman Villani Yu • Effect of Atrial Fibrillation Duration on Probability of Immediate Recurrence after Transthoracic Cardioversion H Oral, M Ozadyn, C Sticherling, H Tada, C Scharf, A Chugh, SWK Lai, F Pelosi, BP Knight, SA Strickeberger, F Morady. JCE 2003; 14: 182-5 Immediate Recurrence of AFib (IRAF) According to the Duration of Arrhythmia 100 Prevalence of IRAF (%) 90 80 70 60 48 50 27 40 30 34 20 45 72 10 0 1 hr 1-24 hrs 1-7 days 7-30 days 31-90 days 36 13 40 91-180 181-365 days days >365 days Duration of AFib Oral H, et al. J Cardiovasc Electrophysiol (2003) 14: 182 Oral Propafenone Before Electrical Cardioversion in Persistent AFib Effect on early recurrence of arrhythmia 100 80 70 60 Propafenone Placebo 0 10 min 24 min 48 min Complex atrial arrhythmia (%) Sinus rhythm (%) 90 50 70 p<0.01 p<0.002 60 52 50 40 30 20 18 10 0 10 minutes Bianconi L, et al. J Am Coll Cardiol (1996) 28: 700 Effect of Pre-treatment with Oral Amiodarone 30 Amiodarone GIK No treatment 100 p<0.005 p<0.05 80 Conversion (%) Conversion (%) 24 Amiodarone GIK No treatment 18 12 60 40 6 20 0 0 SR before ECV SR with cardioversion No differences in energy for cardioversion Capucci A, et al. Eur Heart J (2000) 21: 66 Short- and Long-term Treatment with Amiodarone after Cardioversion Reduces Recurrence Stable anticoagulation for 2 weeks Randomization 172 Protocol violation = 4; Withdrew consent = 7 Placebo 38 30 Short-term Amiodarone 62 32 38 DCCV 100 Placebo 30 Long-term Amiodarone 61 16 Sinus Rhythm Short-term Amiodarone 48 10 Chemical 26 Long-term Amiodarone 48 Sinus Rhythm at 8 weeks Placebo 6 (16%) Short-term Amiodarone 29 (47%) Long-term Amiodarone 34 (56%) Sinus Rhythm at 52 weeks Placebo 2 (5%) Short-term Amiodarone 20 (32%) Long-term Amiodarone 30 (49%) Chenner KS, et al. Eur Heart J (2004) 25: 144 Effect of Pre-treatment with Ibutilide IV SR before ECV SR after ECV AFib • Successful cardioversion 50 in all patients given ibutilide and in 14/50 patients failing cardioversion alone Patients (%) 40 • The mean energy for 30 defibrillation was less with ibutilide 20 • Sustained polymorphic tachycardia in 2/64 (3%) patients treated with ibutilide within 15 min of the infusion 10 0 IBU No IBU Oral H, et al. N Engl J Med (1999) 340: 1849 • Pre-treatment with Verapamil in Patients with Persistent or Chronic Atrial Fibrillation Who Underwent Electrical Cardioversion A De Simone, G Stabile, DF Vitale, P Turco, M Di Stasio, F Petrazzuoli, M Gasparini, C De Matteis, R Rotunno, T Di Napoli. J Am Coll Cardiol (1999) 34: 810-4 Pre-treatment with Verapamil for Reducing Recurrence post-ECV 60 PFN PFN + VER PFN - VER p=0.04 p=0.02 Recurrence (%) 50 p=0.04 39 p=0.01 40 30 30 20 10 0 15 17 10 6 1 week 3 months De Simone A, et al. J Am Coll Cardiol (1999) 34: 810 • Effects of Pre-treatment with Verapamil on Early Recurrences after Electrical Cardioversion of Persistent Atrial Fibrillation A Randomised Study E Bertaglia, D D’Este, A Zanocco, F Zerbo, P Pascotto. Heart (2001) 85: 578-80 Effect of Pre-treatment with Verapamil on Early Recurrence Following ECV A randomised trial (90 patients with amiodarone) 60 Amio + Ver Amio NS 50 Recurrence (%) NS 40 30 NS 20 10 0 6h 7d 30 d Follow-up Bertaglia E, et al. Heart (2001) 85: 578-80 Effect of Verapamil on Immediate and Early Recurrence after Cardioversion of AFib • Effectiveness demonstrated – A De Simone et al (JACC 1999) – E Daoud et al (JCE 2000) – GQ Villani et al (AHJ 2002) – A De Simone et al (AJC 2002) – GL Botto et al (JACC 2002) • Not efficacious – E Bertaglia et al (Heart 2001) – T Van Noord et al (JCE 2001) – H Ramanna et al (JACC 2001) Cardioversion of AFib and Maintenance of SR 100 Serial ECV 1 ECV, no AADs Maintenance of SR (%) 90 80 70 60 50 40 30 20 10 0 1 2 3 4 5 6 7 8 9 10 11 12 Months post-cardioversion Van Gelder IC, et al. Arch Int Med (1996) 156: 2585 • Success of Serial External Electrical Cardioversion of Persistent Atrial Fibrillation in Maintaining Sinus Rhythm E Bertaglia, D D’Este, F Zerbo, F Zoppo, P Delise, P Pascotto. European Heart Journal (2002) 23: 1522-8 Serial Electrical Cardioversion 90 patients with persistent AFib who had previously undergone at least one successful electrical cardioversion Randomization Cardioversion repeated up to 2 times in case of recurrent AFib within 1 month of the preceding electrical cardioversion (Group AGG) or Recurrences were left untreated (Group CTL) Bertaglia E, et al. Eur Heart J (2002) 23: 1522 Persistence of Sinus Rhythm During Long-term Follow-up Aggressive repeated ECV beneficial in highly recurrent persistent AFib Sinus rhythm (%) Group AGG Group CTL 100 90 80 70 60 50 40 30 20 10 0 0 7 30 days 180 365 Bertaglia E, et al. Eur Heart J (2002) 23: 1522 2.Treatment Options for AFib Drugs to Prevent AFib Drugs to Prevent AFib • Antiarrhythmic drugs – Class I-III antiarrhythmics • Non-antiarrhythmic drugs – ACE-I, ARBs – Statins – PUFA Rationale for Drug Treatment to Prevent Recurrence • Suppression of symptoms • Avoidance of tachycardia-induced cardiomyopathy • Reduction of thromboembolism • Prevention of heart failure? • Decrease of mortality? Drugs to Prevent AFib Antiarrhythmics Vaughan Williams Classification Type lA Disopyramide Procainamide Quinidine Type IB Lidocaine Mexiletine Type IC Flecainide Moricizine Propafenone Type II Beta-blockers Type III Amiodarone Bretylium Dofetilide Ibutilide Sotalol Type IV Calcium antagonists Drugs to Maintain SR in Patients with AFib – Recommended Daily Doses • Disopyramide 400-750 mg • Procainamide 1000-4000 mg • Quinidine 600-1500 mg • Flecainide 200-300 mg • Propafenone 450-900 mg • Amiodarone 100-400 mg • Dofetilide 500-1000 mcg • Sotalol 240-320 mg Effectiveness of Current AADs • Even with the most effective AAD, such as amiodarone, long-term efficacy is low ~50% or less at 1 year Prevention of Recurrence with AADs No. of Events/Total Drugs studied Antiarrhythmic vs Control Class IA Disopyramide hydrochloride Quinidine sulfate All class IA Class IB All: aprindine hydrochloride, bidisomide Class IC Flecainide acetate Propafenone hydrochloride All class IC Class II All: metroprolol tartrate No. of Studies Antiarrhythmic Peto OR (95% Cl) Control p value 0.10 1 10 2 40/75 49/71 0.52 (0.27-1.01) 0.05 7 8 741/1106 781/1118 417/518 449/564 0.51 (0.40-0.65) 0.51 (0.40-0.64) <0.001 <0.001 2 639/781 453/540 0.84 (0.63-1.13) 0.26 3 31/71 56/78 0.31 (0.16-0.60) <0.001 5 376/720 276/378 0.37 (0.28-0.48) <0.001 9 443/843 342/466 0.36 (0.28-0.45) <0.001 1 127/197 140/197 0.74 (0.49-1.13) 0.16 Amiodarone 4 200/428 209/245 0.19 (0.14-0.27) <0.001 Dofetilide 2 252/431 274/325 0.28 (0.20-0.38) <0.001 Sotalol hydrochloride 9 916/1391 622/815 0.53 (0.44-0.65) <0.001 Dronedarone 1 116/151 43/48 0.45 (0.20-1.02) 0.06 15 1484/2401 1148/1433 0.37 (0.32-0.43) <0.001 Class III All class III Lafuente-Lafuente C, et al. Arch Intern Med (2006) 166: 719 Prevention of Recurrence with AADs Prevention of recurrence in studies comparing AADs with placebo or no treatment Proportion without Recurrence (%) 70 60 50 40 30 20 10 0 Quinidine Disopyramide Propafenone Flecainide Amiodarone Sotalol Lafuente-Lafuente C, et al. Arch Intern Med (2006) 166: 719 Antiarrhythmic Drugs for Maintenance of Sinus Rhythm Meta-analysis of 18 randomized, controlled trials 7 6 Odds Ratio 5 4 3 2 1 0 Quinidine Disopyramide Propafenone Flecainide Amiodarone Sotalol Amiodarone > risk of non-cardiac adverse effects Tamariz L, et al. J Am Coll Cardiol 2003: 536A Amiodarone to Prevent Recurrence of AFib CTAF Study: mean follow-up 16 months 100 Patients without AFib (%) p<0.001 80 60 40 Sotalol 20 0 0 Propafenone Amiodarone 100 200 300 400 500 600 Follow-up (days) Roy D, et al. N Engl J Med (2000) 342: 913 AFFIRM Substudy of First AntiArrhythmic Drug AFFIRM Study 222 pts 256 pts Percent without recurrence 100 p=0.011 100 62% 60% 80 80 60 60 Amiodarone 40 Amiodarone 40 23% 38% Class I Drugs 20 0 p<0.001 0 1 2 3 Years Sotalol 20 4 5 0 0 1 2 3 4 5 Years AFFIRM Investigators J Am Coll Cardiol (2003) 42: 20 Amiodarone and Solatolol Equivalent in Patients with Ischaemic Heart Disease SAFE-T Investigators All patients Patients with IHD 1.0 0.8 Amiodarone 0.6 Sotalol 0.4 Placebo 0.2 0 0 200 400 600 800 1000 Probability of remaining in SR Probability of remaining in SR 1.0 0.8 0.6 Amiodarone 0.4 Sotalol 0.2 Placebo 0 0 200 400 600 800 1000 Follow-up (days) Singh BN, et al. N Engl J Med (2005) 352: 1861 Major Adverse Experiences Associated with Early Drug Discontinuation • Hypothyroidism 7.0% • Hyperthyroidism 1.4% • Peripheral Neuropathy 0.5% • Lung Infiltrates 1.6% • Liver Dysfunction 1.0% • Bradycardia 2.4% Amiodarone Trials Meta-analysis Investigators Lancet (1997) 350: 1417 Amiodarone Discontinuations Associated with Major Adverse Events • Gastrointestinal events • Pulmonary events 4.0% 2.6% • Ocular events 0.6% • Other 7.1% AFFIRM Investigators J Am Coll Cardiol (2003) 42: 20 Major Adverse Experiences Associated with Early Drug Discontinuation • Amiodarone meta-analysis • CTAF 41% at 2y 18% at 16m • PIAF 25% at 1y • AFFIRM 12.3% at 1y Major Adverse Experiences Associated with AADs Drugs studied No. of Studies Withdrawals Peto OR (95% Cl) Antiarrhythmic vs Control Class IA 0.10 Disopyramide hydrochioride 2 3.85 (1.13-13.20) Quinidine sulfate: higher dose 5 3.58 (2.01-6.40) Quinidine: lower dose 2 0.81 (0.59-1.10) Quinidine: all studies All class IA Class IB All: aprindine hydrochloride Class IC Flecainide acetate Propafenone hydrochloride All class IC Class II All: metoprolol tartrate 7 8 1.90 (0.90-4.02) 2.02 (1.00-4.10) 1 0.66 (0.11-3.95) 3 5 9 9.14 (1.94-42.90) 1.69 (1.09-2.62) 1.93 (1.27-2.93) 1 3.16 (1.43-6.99) Amiodarone 3,4 5.55 (2.24-13.70) Dofetilide 1,2 1.61 (0.41-6.23) 2 0.95 (0.68-1.33) Sotalol: rest of studies 6,7 3.02 (1.65-5.53) Sotalol: all studies 8,9 1.47 (0.84-2.60) 2 2.46 (1.51-4.01) 14,16 1.63 (1.29-2.07) 1 10 Class III Sotalol hydrochloride: PAFAC, SOPAT Azimilide dihydrochloride + Dronedarone All class III Lafuente-Lafuente C, et al. Arch Intern Med (2006) 166: 719 Proarrhythmia Associated with AADs Drugs studied No. of Studies Proarrhythmia Peto OR (95% Cl) Antiarrhythmic vs Control Class IA Disopyramide hydrochloride 2 No Events Quinidine sulfate: higher dose 5 4.56 (1.20-17.30) Quinidine: lower dose 2 1.53 (0.64-3.60) Quinidine: all studies All class IA Class IB All: aprindine hydrochloride Class IC Flecainide acetate Propafenone hydrochloride All class IC Class II All: metoprolol tartrate 7 8 2.10 (1.02-4.33) 2.06 (1.00-4.26) 1 No Events 3 5 9 5.97 (1.67-21.30) 1.52 (0.33-7.02) 3.41 (1.28-9.09) 1 7.96 (2.84-22.30) Amiodarone 3, 4 2.65 (0.88-8.00) Dofetilide 1, 2 3.77 (1.31-10.80) 2 1.42 (0.56-3.60) Sotalol: rest of studies 6, 7 2.67 (1.44-4.98) Sotalol: all studies 8, 9 2.20 (1.31-3.69) 2 3.30 (1.01-10.80) 14, 16 2.20 (1.31-3.69) 0.10 1 10 Class III Sotalol hydrochloride: PAFAC, SOPAT Azimilide dihydrochloride + dronedarone All class III Lafuente-Lafuente C, et al. Arch Intern Med (2006) 166: 719 Proarrhythmic Profile of AADs Torsade de Pointe Dysopiramide Quinidine Procainamide Lidocaina Mexiletine Morizicine Propafenone Flecainide Amiodarone Ibutilide Sotalol 1-2% 2% 1-2% Rare Rare Rare <1% 4-5% 2-5% Atrial Flutter 1:1 Bradyarrhythmia VF VT * ++ ++ ++ Rare Rare + + + + + + + Rare Rare ++ ++ ++ + + + + ++ ++ + Rare ++ +++ +++ + + + + + Rare Rare + ++ ++ +++ Rare +++ * More frequent in pts with structural HD or history of ventricular arrhythmias Friedman P, et al. Am J Cardiol (1998) 82: 50N Overall Mortality Associated with AADs Drugs studied Antiarrhythmic vs Control Class IA Disopyramide phosphate Quinidine sulfate All class IA Class IB All: aprindine hydrochloride, bidisomide Class IC Flecainide acetate Propafenone hydrochloride All class IC Class II All: metroprolol tartrate No. of Studies No. of Events/Total Antiarrhythmic Peto OR (95% Cl) Control p value 0.10 1 10 2 2/75 0/71 7.56 (0.47-1.22) 0.16 7 8 21/1128 23/1203 4/548 4/594 2.26 (0.93-5.45) 2.39 (1.03-5.59) 0.07 0.04 2 9/781 3/540 1.89 (0.59-6.03) 0.28 3 0/71 0/78 Not estimable NA 5 0/720 2/378 0.05 (0.00-1.02) 0.05 9 1/843 2/466 0.14 (0.00-1.88) 0.14 1 3/197 0/197 7.47 (0.77-72.20) 0.08 Amiodarone 4 13/428 3/245 1.96 (0.68-5.67) 0.21 Dofetilide 2 83/431 83/325 0.97 (0.67-1.40) 0.88 Sotalol hydrochloride 9 30/1391 5/815 2.09 (0.97-4.49) 0.06 Azimilide dihydrochloride + dronedarone 2 10/1042 4/537 1.31 (0.43-3.97) 0.63 16 136/3292 95/1922 1.19 (0.88-1.61) 0.27 Class III All class III Lafuente-Lafuente C, et al. Arch Intern Med (2006) 166: 719 Mortality Associated with Class 1A Drugs Prophylaxis of AFib with quinidine: Meta-analysis of 6 randomized trials 100 80 Quinidine Placebo p<0.001 p<0.001 p<0.001 p<0.05 69 58 (%) 60 50 45 40 33 25 20 # of patients 17 3 0 3 month 6 month 12 month Mortality Coplen SE, et al. Circulation (1990) 82: 1106 Physician Visits Associated with AAD Use Over Time 7 Visits on medication (%) 6 Quinidine Class IC Amiodarone Hydrochloride 5 4 3 2 1 0 1991-1992 1993-1994 1995-1996 1997-1998 1999-2000 Visit (years) Fang FC et al. Arch Intern Med 2004; 164: 55-60 Rhythm and Rate Control Studies • PIAF, Lancet 2000 • RACE, NEJM 2002 • AFFIRM, NEJM 2002 • PAF-2, Eur Heart J 2002 • STAF, JACC 2003 • HOT-CAFÉ, Chest 2004 Rhythm vs Rate Trials Trial n Age, y AFFIRM Rate control Rhythm control 2027 2033 70 70 256 266 68 68 100 100 65 66 85 70 6 7.5 21 24 10 39 96-99 86-99 5.5 7.9 17 13 0 NR NR NR 0.6 3.1 5 2.5 10 56 100 100 NR NR 1.6 1.6 NR 63.5 74 NR 1 2.9 1 2.9 12m 125 127 61 60 Hot Cafe Rate control Rhythm control 35 63 22m PIAF Rate control Rhythm control Mortality % 27m STAF Rate control Rhythm control Thromboembolic complications % 42m RACE Rate control Rhythm control Mean Follow-up Sinus rhythm Warfarin (%) (%) 20m 101 104 61 60 Falk, RH. Circulation (2005) 111: 3141 AFib Follow-up Investigation of Rhythm Management (AFFIRM) No survival advantage of rhythm over rate (n=4060) Cumulative mortality (%) 30 p=0.08 25 Rhythm control 20 15 Rate control 10 5 0 No. of deaths 0 1 2 3 4 5 Years Rhythm control 0 80 (4) 175 (9) 357 (13) 314 (18) 352 (24) Rate control 0 78 (4) 148 (7) 210 (11) 275 (16) 306 (21) AFFIRM Investigators N Engl J Med (2002) 347: 1825 Meta-Analysis of Rhythm Control versus Rate Control Studies Odds Ratio for Combined Endpoint (All-cause Death + Thromboembolic Stroke) Study or sub-category Rate control (n/N) Rhythm control (n/N) Weight (%) OR (95% CI Random) Van Den Berg 388/2027 438/2033 89.86 0.86 (0.74, 1.00) SOLVD 1/101 6/104 0.46 0.16 (0.02, 1.38) TRACE 2/125 4/127 0.72 0.50 (0.09, 2.78) Ueng 24/256 32/266 6.72 0.76 (0.43, 1.32) CAPP 97100 9/100 2.24 1.00 (0.38, 2.63) 2609 2630 100.0 0.85 (0.73, 0.98) Total (95% CI) OR (95% CI Random) 0.1 0.2 Total events: 424 (Rate control). 489 (Rhythm control) Test for heterogeneity chi-square=2.97; df=4; p=0.56; I2=0% Test for overall effect z=2.24; p=0.03 0.5 Rate control better 1 2 5 10 Rhythm control better Testa L, et al. Eur Heart J (2005) 26: 2000 AFFIRM On-Treatment Analysis: SR but not AAD Use Associates with Improved Survival Covariate HR: 99% CL Lower Upper p HR Age at enrollment* <0.0001 1.06 1.04 1.08 Coronary artery disease <0.0001 1.65 1.31 2.07 Congestive heart failure <0.0001 1.83 1.45 2.32 Diabetes <0.0001 1.56 1.22 2.00 Stroke or transient ischemic attack <0.0001 1.54 1.17 2.05 Smoking <0.0001 1.75 1.29 2.39 0.0067 1.27 1.01 1.58 Sinus rhythm <0.0001 0.54 0.42 0.70 Warfarin use <0.0001 0.47 0.36 0.61 Digoxin use <0.0001 1.50 1.18 1.89 0.0005 1.41 1.10 1.83 First episode of AFib Rhythm-control drug use * per year of age AFFIRM Investigators Circulation (2004) 109: 1509 AFFIRM On-Treatment Analysis: SR Associates with Survival Implications In patients with AFib such as those enrolled in the AFFIRM study, warfarin improves survival. The presence of SR but not AAD use is associated with a lower risk of death. These results suggest that if an effective method for maintaining SR with fewer side effects were available, it might improve survival AFFIRM Investigators Circulation (2004) 109: 1509 Drugs to Prevent AFib Non-antiarrhythmic drugs Non-antiarrhythmic Drugs to Prevent AFib • ACE Inhibitors and Angiotensin Receptor Blockers • Statins • Polyunsaturated fatty acids (omega-3) Non-antiarrhythmic drugs ACE Inhibitors and Angiotensin Receptor Blockers Characteristics of ARB and ACE-I Studies in AFib Drug No. Randomized Mean Follow-Up Mean LVEF HTN (%) Rate of AF in Control Group (%) AF, CHF Lisinopril 30 84 days n/a n/a 64 AF Enalapril 145 270 days (61-575) 51 32 43 LVD, CHF, NSR Enalapril 374 3.3 yrs 27 20 24 Post-MI, NSR Lisinopril 17,711 42 days n/a 30 8 Post-MI, LVD, NSR Trandolapril 1,577 2-4 yrs 33 22 5 STOP-H2, 1999 HTN Enalapril 10,985 5.0 yrs n/a 100 8 CAPP, 1999 HTN Captopril 6,614 6.1 yrs n/a 100 2 CHF, NSR Candesartan 5,518 3.2 yrs 39 55 8 AF Irbesartan 154 254 days (60-710) 64 42 29 ValHeFT, 2003* CHF, NSR Valsartan 4,409 2 yrs 28 7 8 Wachtell, (LIFE), 2003* HTN, LVH, NSR Losartan 9,193 4.9 yrs n/a 100 6 Author/Study, Date Patient Group ACE-I trials Van Den Burg, 1995 Ueng, 2003 Vermes (SOLVD), 2003 Pizetti (GISSI), 2001 Pedersen (TRACE), 1999 ARB trials CHARM, 2003* Madrid, 2002 *Abstract only. ACEI = angiotensin-converting enzyme inhibitor; AF = atrial fibrillation; ARB = angiotensin receptor blocker; CHF = congestive heart failure; HTN = hypertension; LVD = left ventricular dysfunction; LVEF = left ventricular ejection fraction; LVH = left ventricular hypertrophy; NSR = sinus rhythm; Post-MI = post-myocardial infarction Healey JS, et al. J Am Coll Cardiol (2005) 45: 1832 Effect of Treatment Based on Class of Drug: ACE Inhibitors Treatment (n/N) Control (n/N) 2/7 SOLVD TRACE RR (95% CI Random) Weight (%) RR (95% CI Random) 7/11 1.7 0.45 (0.13, 1.57) 10/186 45/188 4.8 0.22 (0.12, 0.43) 22/790 42/787 6.6 0.52 (0.31, 0.87) Ueng 18/70 32/75 7.0 0.60 (0.37, 0.97) CAPP 117/5492 135/5493 11.4 0.87 (0.68, 1.11) STOP-H2 200/2205 357/4409 13.0 1.12 (0.95, 1.32) GISSI 665/8855 721/8846 14.0 0.92 (0.83, 1.02) 1034/17615 1339/19809 58.7 0.72 (0.56, 0.93) Study ACE inhibitor Van Den Berg Sutotal (95% CI) 28% p=0.01 Test for heterogeneity chi-square=32.58; df=6; p<0.00001 Test for overall effect z=-2.53; p=0.01 1 2 0 5 10 Healey JS, et al. J Am Coll Cardiol (2005) 45: 1832 Effect of Treatment Based on Class of Drug: ARBs Treatment (n/N) Control (n/N) 9/79 22/75 ValHeFT 116/2209 173/2200 Charm 179/2769 216/2749 LIFE 179/4417 252/4387 Sutotal (95% CI) 483/9474 663/9411 Study RR (95% CI Random) Weight (%) RR (95% CI Random) 43 0.39 (0.19, 0.79) 11.8 0.67 (0.53, 0.84) 12.5 0.82 (0.68, 1.00) 12.6 0.71 (0.59, 0.85) 41.3 0.71 (0.60, 0.84) ARB Madrid 29% p=0.00002 Test for heterogeneity chi-square=5.25; df=3; p=0.15 Test for overall effect z=-4.12; p=0.00004 1 2 0 5 10 Healey JS, et al. J Am Coll Cardiol (2005) 45: 1832 Effect of ACE Inhibitors or ARB Based on Indication RR (95% CI Random) Study Treatment (n/N) Control (n/N) Heart Failure Van Den Berg 2/7 7/11 SOLVD 10/186 45/188 ValHeFT 116/2209 173/2300 Charm 179/2769 216/2749 Sutotal (95% CI) 307/5171 441/5148 Test for heterogeneity chi-square=15.01; df=3; p<0.0018 Test for overall effect z=-2.72; p=0.007 Hypertension CAPP 117/5492 135/5493 LIFE 178/4417 252/4387 STOP-H2 200/2205 357/4409 Sutotal (95% CI) 496/12114 744/14/283 Test for heterogeneity chi-square=13.34; df=2; p=0.0013 Test for overall effect z=-0.82; p=0.4 1 2 0 Weight (%) RR (95% CI Random) 44% 1.7 4.8 11.8 12.5 30.9 0.45 0.22 0.67 0.62 0.56 (0.13, (0.12, (0.53, (0.66, (0.37, 1.57) 0.43) 0.84) 1.00) 0.85) 12% 11.4 12.6 13.0 37.1 0.87 0.71 1.12 0.88 (0.69, (0.59, (0.95, (0.65, 1.11) 0.85) 1.32) 1.19) 5 10 Healey JS, et al. J Am Coll Cardiol (2005) 45: 1832 Effect of ACE Inhibitors or ARB Based on Indication Study Treatment (n/N) RR (95% CI Random) Control (n/N) Atrial Fibrillation Madrid 9/79 22/75 Ueng 15/70 32/75 Sutotal (95% CI) 27/149 54/150 Test for heterogeneity chi-square=1.33; df=1; p=0.31 Test for overall effect z=-3.13; p=0.002 Post-Myocardial Infarction TRACE 22/790 42/787 GISSI 665/8865 721/6646 Sutotal (95% CI) 27/149 54/150 Test for heterogeneity chi-square=4.64; df=1; p=0.031 Test for overall effect z=-1.12; p=0.3 1 2 0 Weight (%) RR (95% CI Random) 48% 4.3 7.0 11.4 0.39 (0.19, 0.79) 0.60 (0.37, 0.97) 0.52 (0.35, 0.79) 27% 6.6 14.0 20.7 0.52 (0.31, 0.87) 0.92 (0.83, 1.02) 0.73 (0.43, 1.26) 5 10 Healey JS, et al. J Am Coll Cardiol (2005) 45: 1832 Non-antiarrhythmic drugs Statins Studies of Statins to Prevent AFib Study Design Statin drugs in protecting against AFib Retrospective analysis of prospective study database Medication and subjects OR Comments Statin users vs nonusers in a population of chronic CAD (n=449) 0.48 (CI 0.28-0.83) Effect of statins was independent of changes in serum cholesterol. AFib diagnosed by ECG at routine follow-up visits or with new symptoms onset. Prevention of AFib Retrospective recurrence after analysis of cardioversion patients referred for cardioversion Statin users vs nonusers in a population with persistent lone AFib (n=62) 0.31 (CI 0.10-0.90) Prevastatin to prevent recurrent AFib after electrical cardioversion Pravastatin 1.08 (CI not 40 mg/day vs available) no drug 3 weeks prior and 6 weeks cardioversion (n=114) Prospective, open-label, controlled multicenter study 52% 69% 8% Patients on statins had higher cholesterol and were older than nonusers. AFib diagnosed by ECG at routine follow-up visits. Open-label design, small study, conventional antiarrhythmics also used. Lozano HF, et al. Heart Rhythm (2005) 2: 1000 Effect of Atorvastatin on Reducing AFib Recurrence Post-ECV 48 patients with AFib lasting >48h and followed for 3m Freedom from recurrence 1.0 Atorvastatin 0.9 0.8 p=0.01 0.7 control 0.6 0.5 0 30 60 90 Follow-up (days) Ozaydin M, et al. Am J Cardiol (2006) 297: 1490 Non-antiarrhythmic drugs Polyunsaturated fatty acids (omega-3) Polyunsaturated Fatty Acids in Preventing AFib 100 PUFAs Group Control Group Patients free of AFib (%) 90 80 70 60 Log-rank p=0.009 50 40 30 20 10 0 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 Days after surgery Calò L, et al. J Am Coll Cardiol (2005) 45: 1723 AFib-Free Survival According to Fish Consumption Tuna or other broiled/baked fish 1.0 Survival free of AFib p<0.0001 (log-rank test for equality of survivor functions) 0.9 5+/wk 0.8 1-4/wk 1-3/mo 0.7 <1/mo 0.6 0 2 4 6 8 10 12 Years Mozzafarian D, et al. Circulation (2004) 110: 3683 AFib-Free Survival According to Fish Consumption Fried fish or fish sandwich 1.0 Survival free of AFib p=0.0001 (log-rank test for equality of survivor functions) 0.9 0.8 <1/mo 1-3/mo 1+/wk 0.7 0.6 0 2 4 6 8 10 12 Years Mozzafarian D, et al. Circulation (2004) 110: 3683 n-3 Fatty Acid Intake from Fish and Incidence of AFib Rotterdam study • European population-based prospective cohort study among subjects aged 55 years and above (n=6808) • Dietary intake data available from 5184 subjects without AFib – In the subsequent 6.4y follow-up period, 312 subjects developed AFib – Incidence of AFib was not significantly associated with either long-chain fatty acid consumption or fish consumption Brouwer IA, et al. Am Heart J (2006) 151: 857 Treatment Options for AFib Drugs to Control Ventricular Rate Permanent AFib and Ventricular Rate Control Indications for control of ventricular rate: • Failure of antiarrhythmic therapy for preventing recurrence • Alternative treatment to maintain sinus rhythm Definitions and Criteria for Rate Control Clinical symptoms ECG Criteria Hemodynamic data VR 60 - 80 bpm At rest VR 90 - 115 bpm During moderate exercise Drugs Used for Rate Control • Digoxin • Calcium Antagonists • Beta-Blockers • Antiarrhythmic Drugs ACC/AHA/ESC 2006 Guidelines for the Management of Patients With Atrial Fibrillation J Am Coll Cardiol (2006) 48: 854 Rate Control Drugs in AFFIRM • Digoxin 51% • Beta-blockers 49% • Calcium antagonists 41% • AV node ablation 5% Digoxin in Permanent AFib • Heart rate during physical exercise and at various plasma concentrations 190 191 SR Low Nil High 182 171 170 p<0.05 150 bpm 164 161 140 130 118 108 110 105 93 90 83 72 70 50 Rest Moderate Strenuous Beasley R, et al. Br Med J (1985) 290: 9 Digoxin plus Diltiazem in Permanent AFib • Medium and high doses alone or in combination with digoxin 190 DG DL 240 DG+DL 240 DL 360 170 170 *° bpm 150 * p<0.05 vs DG+DL * p<0.05 vs DL 360 ° p<0.05 vs DG 240 130 110 90 70 50 142 132 128 * 101 136 106 88 86 * 154 79 67 Rest Submax Exercise Max Exercise Roth A, et al. Circulation 73: 316 Calcium Antagonists in Permanent AFib Study protocol • Gallopamil 100 mg b.i.d. • Diltiazem 120 mg b.i.d. • Verapamil 120 mg b.i.d. • Digoxin 0.8 – 1.4 µg/ml (7 day administration of slow release formulation) Botto GL, et al. Clin Cardiol 21: 837 Calcium Antagonists in Permanent AFib Holter and walking test 175 DGX DLT GLL VRP 167 149 150 ° * p<0.001 o p<0.01 vs DGX * 137 * bpm 125 142 100 90 91 82 80 75 59 50 Median VR 63 59 59 Minimum VR Maximum VR Botto GL, et al. Clin Cardiol 21: 837 Nadolol for Control of Ventricular Rate • Effect on heart rate in patients on digoxin 200 175 DGX NDL p<0.01 150 bpm 125 100 75 50 25 0 Resting Low Average 3’ Exercise Max Exercise Nadolol median dose 87 mg DiBianco R, et al. Am Heart J (1984) 108: 1121 Beta-blockers for Control of Ventricular Rate • Effect of nadolol on physical exercise capacity 500 DGX 24 DLT p<0.01 22 kg/min Sec CLP p<0.01 450 400 350 300 DGX 20 18 Exercise time DiBianco R, et al. Am Heart J (1984) 108: 1121 16 O2 Consumption Atwood JE, et al. J Am Coll Cardiol (1987) 10: 314 Modulation of Ventricular Rate Study protocol • Metoprolol 200 mg/d • Diltiazem 300 mg/d • Digoxin 0.8 – 1.4 µg/ml • Placebo Randomized, cross-over study with administration for 7-10 days Botto GL, et al. PACE (2000) 23: 649 Modulation of Ventricular Rate • Walking test results 190 Placebo DGX 320 DLT MTP 185 300 175 170 * 165 o 160 Metres walked Max heart rate 180 280 * *o * 260 155 150 240 * p<0.05 vs PLA e DGX o p<.,01 vs PLA e DGX * p<0.005 vs DGX o p<0.05 vs MTP Botto GL, et al. PACE (2000) 23: 649 Antiarrhythmic Drugs for Control of Ventricular Rate • Amiodarone • Solatolol CHF-STAT Study: Amiodarone in Permanent AFib 100 90 Placebo Amiodarone (400 mg/d) NS p=0.001 p=0.001 p=0.006 Baseline 2w 6m 12 m 80 70 bpm 60 50 40 30 20 10 0 Deedwania PC, et al. Circulation (1998) 98: 2574 Treatment Options for AFib Drugs to Reduce Thromboembolic Risk Atrial Fibrillation and Stroke • Anticoagulant therapy is clearly indicated and beneficial in valvular atrial fibrillation. • In non-valvular atrial fibrillation, major randomized trials have provided useful guidelines for identifying and treating patients at risk. Major Clinical Trials of Primary Prevention in Non-Valvular AFib • SPAF1 Stroke Prevention in Atrial Fibrillation • BAATAF2 Boston Area Anticoagulation Trial for Atrial Fibrillation • CAFA3 Canadian Atrial Fibrillation Anticoagulation • AFASAK4 Copenhagen Investigators • SPINAF5 Stroke Prevention in Non-rheumatic Atrial Fibrillation 1 Lancet (1989) 1: 175 2 N Engl J Med (1990) 323: 1505 3 J Am Coll Cardiol (1991) 18: 349 4 Circulation (1991) 84: 527 5 N Eng J Med (1992) 327: 1406 Major Clinical Trials of Primary Prevention in Non-Valvular AFib SPAF BAATAF CAFA 1330 420 378 Warfarin ASA (INR 2-4.5) 325 mg Warfarin (PT 1.2-1.5x Control) Warfarin (INR 2-3) Number of Patients Drug Used AFASAK SPINAF 1007 571 Warfarin ASA Warfarin (INR 2.8-4.2) 75 mg (INR 1.2-1.5) Embolic Rate (%) Treatment Control Risk Reduction (%) (95% confidence) 2,3 7,4 3,6 6,3 0,41 2,98 3,5 5,2 1,5 6,2 6,0 6,2 4,3 0,9 67 42 86 45 53 — 79 1.5 1.6 1.4 1.9 0.9 0.5 2.5 0.5 6.3 0.0 0.6 0.0 1.5 0.9 Major Bleeding Complications (%) Treatment Control Adjusted Dose Warfarin vs Placebo Risk reduction Events Pts/y AFASAK 27 811 BAATAF 15 922 CAFA 14 478 SPAF 23 508 SPINAF 29 972 108 3691 All 100% 50% Warfarin better 0% -50% -100% Warfarin worse Reduction in Stroke Risk – Metaanalysis of 5 Trials Annual risk of stroke (%) 5 4.5% 4 Reduction in risk = 68% 3 2 1.4% 1 0 Control Warfarin Atrial Fibrillation Investigators Arch Intern Med (1994) 154: 1449 Secondary Prevention Study Range INR Average EAFT 2.5 – 4.0 Stroke risk reduction - 68% - 62% vs placebo 1007 patients > 70 with previous TIA or minor stroke European Atrial Fibrillation Trial Lancet (1993) 342: 1255 Aspirin vs Placebo Study ASA dose Stroke risk reduction Primary prevention AFASAK SPAF 75 mg 325 mg - 18% (ns) - 44% (p<0.02) Secondary prevention EAFT 300 mg - 14% (ns) Global reduction in risk = 25% (range 14-44%) Warfarin Superior to Aspirin Warfarin compared with aspirin Aspirin compared with placebo Relative Risk Reduction (95% CI) Relative Risk Reduction (95% CI) AFASAK I (1) AFASAK I (1) SPAF I (3) AFASAK II (2) EAFT (9) EAFT (9) ESPS II (14) PATAF (15) LASAF (13) SPAF II (4) UK-TIA (16) All trials (n=5) All trials (n=6) 100 50 0 -50 -100 Warfarin better Warfarin worse (%) (%) 100 50 Aspirin better (%) 0 -50 -100 Aspirin worse (%) ACC/AHA/ESC 2006 Guidelines for the Management of Patients With Atrial Fibrillation J Am Coll Cardiol (2006) 48: 854 SPAF III - Adjusted-dose vs. Lowintensity, Fixed-dose warfarin + ASA 1044 eligible patients randomised Adjusted dose warfarin (n = 523) Fixed, low dose warfarin plus aspirin (n = 521) Weekly INR control until stable, then monthly INR assessed at 1m and 2m then every 3m Discontinued = 31 Lost to follow-up = 0 Discontinued = 41 Lost to follow-up = 0 Primary events = 11 Deaths = 34 Completed without primary event = 478 Primary events = 44 Deaths = 35 Completed without primary event = 442 SPAF Investigators Lancet (1994) 343: 634 Cumulative event rate (% per year) SPAF III – Stroke Rate 20 18 16 14 Combination therapy 12 10 8 6 Adjusted-dose warfarin 4 2 0 365 0 730 Days from randomization Number at Risk Combination therapy 521 378 265 166 61 Warfarin therapy 523 397 273 173 65 SPAF Investigators Lancet (1996) 348: 633 SPAF III – Relative Risk Primary events Disabling ischaemic stroke All disabling strokes Vascular death Stroke, MI, Vascular death Major haemorrhage 0 0-5 Adjusted dose warfarin better 1 1-5 2 Combination therapy better SPAF Investigators Lancet (1996) 348: 633 AFASAK 2 - Copenhagen Investigators 677 patients with permanent AFib Warfarin fixed-dose 1.25 mg 5.8 % Warfarin fixed-dose 1.25 mg + ASA 300 mg 7.2 % ASA 300 mg 3.6 % Warfarin dose variable (INR 2.03.0) 2.8 % Cumulative incidence of primary events – 12m follow-up Primary Prevention Trials – Anticoagulation Ranges Warfarin – INR range AFASAK 2.8-4.2 SPAF I + II 2.0-4.5 BAATAF 1.5-2.7 2.0-3.0 CAFA SPINAF 1.4-2.8 2.5-4.0 EAFT SPAF III 1.2-1.5 (fixed) SPAF III 2.0-3.0 (adjusted) 1.0 1.5 2.0 2.5 3.0 3.5 4.0 INR range (2.0-3.0) recommended by 4th ACCP Consensus on Antithrombotic Therapy 4.5 Optimal Anticoagulation Ranges Therapeutic window Clinical events Thromboembolic 2 INR 3 Haemorrhagic Intracranial haemorrhage (%/y) Intracranial Haemorrhage in Trials – Influence of Age 2 Oral anticoagulant SPAF II (>75) Aspirin CAFA SPAF I SPINAF 1 BAATAF SPINAF (>70) 4 trials (>75) SPAF II (<75) 60 EAFT 65 70 AFASAK 75 80 85 Median age (y) Petersen P, et al. Lancet (1989) 171 SPAF Circulation (1991) 84: 527 BAATAF N Engl J Med (1990) 323: 1505 EAFT Lancet (1993) 342: 1255 Connolly SJ, et al. J Am Coll Cardiol (1991) 18: 349 Ezekowitz MD, et al. N Engl J Med (1992) 327: 1406 SPAF II Lancet (1994) 343: 687 Connolly SJ, et al. Lancet (1994) 343: 1509 Treatment Options for AFib Drugs to Reduce Thromboembolic Risk Risk stratification Thromboembolic Risk Stratification Clinical risk factors Echocardiographic risk factors Clinical Risk Factors Advanced age (> women) Hypertension Cardiac insufficiency Previous TIA (Diabetes) Transthoracic Echocardiographic Risk Factors Left atrial dilatation Left ventricular systolic dysfunction Trans Esophageal Echocardiographic Risk Factors Thrombus – atrium and/or left atrial appendage Dense spontaneous echo contrast Reduced blood flow in left atrial appendage Dilatation of left atrial appendage Septal aneurysm Complex aortic plaque Risk Stratification in Patients with AFib HIGH RISK MODERATE RISK LOW RISK 1 major risk factor NO major risk factor No major or > 1 moderate risk factor 1 moderate risk factor minor risk factors Major Risk Factors Age > 75 Previous stroke or systemic embolism History of arterial hypertension Cardiac insufficiency o ventricular dysfunction Mitral valve disease Prosthetic valve replacement Minor Risk Factors Age 65 - 75 Diabetes mellitus Ischaemic cardiopathy with normal ventricular function sinistra adapted from the 6th ACCP Consensus Conference on Antithrombotic Therapy, Chest (2001) 119 (Suppl): 194S Antithrombotic Therapy Recommendations Risk category No risk factors One moderate-risk factor Any high-risk factor or more than 1 moderate-risk factor Less validated or weaker Risk factors Recommended therapy Aspirin, 81 to 325 mg daily Aspirin, 81 to 325 mg daily, or warfarin (INR 2.0 to 3.0, target 2.5) Warfarin (INR 2.0 to 3.0, target 2.5)* Moderate-risk factors High-risk factors Female gender Age greater than or equal to 75 y Previous stroke, TIA or embolism Age 65 to 74 y Hypertension Mitral stenosis Coronary artery disease Heart failure Prosthetic heart valve* Thyrotoxicosis LV ejection fraction 35% or less Diabetes mellitus *If mechanical valve, target international normalized ratio (INR) greater than 2.5. INR = international normalized ratio; LV = left ventricular; TIA = transient ischemic attack Contraindications of Oral Anticoagulants • GI haemorrhage • Uncontrolled arterial hypertension • Pregnancy • Alcoholism • Severe hepatic insufficiency • Vascular malformations that can lead to risk of haemorrhage • Coagulopathies • Recent surgical interventions – eyes or CNS • Previous severe haemorrhage during anticoagulation therapy • Severe neoplastic disease Cardioversion and Anticoagulation Recommendations AFib > 48 hours TEE Warfarin (INR 2.0-3.0) 3-4 weeks + Cardioversion Warfarin 3-4 weeks Positive Negative Heparin + warfarin 24 h Cardioversion Naccarelli GV, et al. Am J Cardiol (2000) 85: 36D Treatment Options for AFib Non-Pharmacologic Treatment Options Non-Pharmacological Treatment Options for AFib Devices Electrophysiological Surgery Pacemaker (single or dual chamber) Internal atrial defibrillators Catheter ablation AV node ablation Maze procedure Modified Maze (mini-Maze) ACC/AHA/ESC 2006 Guidelines for the Management of Patients With Atrial Fibrillation J Am Coll Cardiol (2006) 48: 854 Management of AFib - Summary • Maintenance of sinus rhythm should be the primary objective of treatment whenever possible – sinus rhythm correlates with improved survival • Current antiarrhythmic drug therapies, however, are not highly effective in maintaining SR and generally have poor outcomes – high recurrence rates – adverse effects and high discontinuation rate • A potentially curative therapy for AFib is desirable