Resident
advertisement

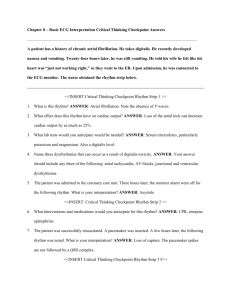
Resident Version Atrial Fibrillation Module Created by Dr. R. Shaun Aries Objectives: 1) You will be able to recognize atrial fibrillation on an EKG. 2) You will be able to appropriately assess and treat a patient with atrial fibrillation during the acute phase. 3) You will be able to provide long term management for atrial fibrillation. 4) You will be able to recognize the causes of and do the initial work up for new onset atrial fibrillation. References: 1. Arnsdorf, MF, Podrid, PJ. Up to Date: Overview of the presentation and management of atrial fibrillation. Updated Sept. 13, 2006. 2. MedStudy: Internal Medicine Review Core Curriculum. 12th ed. 2007, Book 3: Cardiology/Rheumatology. 3. Sabatine MS, et. al. The Massachusetts General Hospital Handbook of Internal Medicine. Pocket Medicine 2nd ed. Lippincott Williams & Wilkinson. 4. Kasper DL, Baunwald E, Fauci AS, Hauser SL, Longo DL, Jameson JL. Harrison’s: Manual of medicine. Sec 8: Cardiovascular diseases. Ch. 125: Arrhythmias, Pg. 638-41. 5. Medstudy: Q & A board style review questions. 2007. CASE Patient is a 67 yo male with h/o DM, HTN, and dyslipidemia who presents to the ED c/o feeling tired. Patient had a cold a couple of weeks ago and has notice that now, although the cold has resolved, he continues to tire more rapidly than usual. He notices this most when he exerts himself. Prior to his cold he could walk several blocks without any problems. Now he has to stop to rest after a couple of blocks. He also finds it hard to make it up the single flight of stairs to his apartment whereas he had no problems with this before. He has a 20 pack year history of smoking but quite several years ago. He drinks alcohol occasionally but denies any history of recreational drug use. He is on Metformin and Glyburide for his diabetes. Additionally he takes HCTZ and Simvastatin for blood pressure and cholesterol respectively. He has no drug allergies and family history is only significant for DM. PE T=37.2, HR=114, BP=98/67, RR=16, O2=93% RA Gen: elderly man who appears his stated age, AAOX3, NAD HEENT: PERRLA, EOMI, OM moist w/o erythema/exudates. Neck: No LAD, trach midline, thyroid normal Lung: CTAB, Normal WOB CV: Tachycardia with an irregular rhythm. Cannot appreciate murmurs as rate is too fast. Abd: Soft, non-tender, non-distended. Normal active bowels and no organomegally. Ext: no edema Neuro: nonfocal. Labs CBC: WBC=9.8, H/H=15/45, Plt=247,000. Chem 10: Na=137, K=3.6, Cl=108, HCO3=20, BUN=14, Cr=0.8, Glu=183, Ca=8.4, Phos=2.3, Mag=1.8. LFT’s: TP=8.2, Alb=3.9, AST=23, ALT=21, AP=96, TB=0.8, DB=0.2. TSH=2.6 D-Dimer=0.4 Trop=<0.04 BNP=100 (normal <100) ECG: please interpret Echo: Irregular rhythm, EF=45-55%, Mild LV hypertrophy, Moderate MR with mild to moderate LA enlargement. No pericardial effusion. Case Questions 1) What is the diagnosis? 2) What would you do now? 3) What is the long term treatment of this condition? Discussion Outline Classification=4 Categories: 1) Paroxysmal AF: Self-terminating within 7 days but may recur. 2) Persistent: Any episode lasting longer than 7 days. 3) Permanent: Lasting longer than 1 years and cardioversion either has not been attempted or has failed. 4) “Lone” AF: Any of the above in individuals without structural heart disease. Causes: 1) PIRATES a. PE/Pericarditis b. Infection c. Regurgitation/stenosis (mitral/tricuspid) d. Alcohol e. Thyroid f. Electrolyte abnormalities (hypomagnesemia) g. Surgery (esp. cardiac) Evaluation: History i. Onset, duration, triggers, relieving elements, and symptoms such as dizziness, weakness, palpitations, decreased exercise capacity, and dyspnea but it may be asymptomatic. Physical i. Auscultation of heart sounds demonstrates an irregular rhythm +/rapid heart rate. May also demonstrate a murmur in the presence of concurrent valvular disease. Labs/studies i. EKG ii. CXR iii. Echo iv. TSH/T4 v. Stress testing vi. Holter monitor vii. EP studies Treatment/Approach to the Patient: AF with rapid ventricular response (RVR) If patient is unstable (eg. Low BP, altered mental status, etc.), consider electrical cardioversion a. Consider risk of thromboembolic event vs. death from vascular collapse. Avoid cardioversion (chemical or electrical) in stable patients because of risk of embolization. Cardioversion without anticoagulation may be safe in the first 48 hours after onset but it is safer to do a TEE first to r/o LA appendage thrombus. Reverse/correct the underlying cause if possible ie. treat fever, hyperthyroidism, infection etc. Rate control with IV beta blocker or AV nodal calcium channel blocker. Avoid antiarrhythmic if possible as they may cause cardioversion. For refractory AF consider radiofrequency ablation and pacer placement. AF with or without RVR Control rate as above if needed. o Consider inserting a temporary pacer in patients with “slow” AF before cardioversion because the patient likely as AV node disease and they may go into asystole. Anticoagulate for 3-4 weeks prior to cardioversion. Then another 4 weeks after cardioversion. Anticoagulate with adjusted dose Warfarin with goal INR of 2-3 if the patient has no contraindications (high risk for falls, allergy to Warfarin, recent GI bleed or surgery, or other bleeding risk). For patients with contraindications, aspirin should be offered as it had a trend toward benefit although not statistically significant (OR 0.68 compared to placebo with 95% CI 0.46-1.02, p = 0.06). Warfarin does not need to be used in “Lone” AF. Indications for anticoagulation is assessed by the mnemonic: CHADS2 o CHF/CAD, HTN, Age >75, DM, Stroke/TIA or prior embolic event. o Patients with a score of 0 (none of these risk factors) can be managed on ASA. Rate control vs. Rhythm control. o Several trials including AFFIRM and RACE trials demonstrated no difference between rate control vs. rhythm control for significant end points and quality of life. o 90 percent of patient with rate control continued to have periodic episodes of AF that were often times asymptomatic. o Only 20-30 percent of patients maintained normal sinus rhythm (NSR) for more than 1 year after cardioversion if antiarrhythmics were not used. Therefore, in general, rate control is easier to maintain and therefore preferred over rhythm control. Take Home Points 1. AF is a common arrhythmia with the hallmarks of an irregularly irregular rhythm on ECG and no P-waves. 2. Approach patient with AF systematically using tools like the “PIRATES” pneumonic. 3. Acute treatment consists of cardioversion for unstable patients and AV nodal blockers for stable patients with tachycardia. 4. Chronic treatment consists of rate lowering meds like metoprolol or digoxin and anticoagulation with either Warfarin or Aspirin depending on CHADS2 criteria. 5. In General, rate control with anticoagulation is preferred to rhythm control. Review Questions 1) A 32 yo female presents with feeling of “doom” and rapid heart beat. She has been healthy and without problems until this presentation. On further questioning, however, you discern that she has lost 15 lbs without a change in her diet. You also note that she appears to have bulging eyes and a fine tremor in her left hand. ECG shows a-fib with normal rate. What are you most concerned about at this point? a) Cor Pulmonale b) Eisenmengers transformation c) Bacterial endocarditis d) Ventricular tachycardia e) Systemic embolization. 2) A 35 yo female presents with sudden onset of SOB. She has AF on the monitor. The PE shows an opening snap at the apex and the S1 appears to be loud. You hear a low-pitched diastolic rumble at the apex. ECG shows AF with left atrial enlargement Which of the following cardiac abnormalities is most likely? a) b) c) d) e) Hypertrophic Cardiomyopathy Mitral Regurgitation Aortic Regurgitation Mitral Stenosis Aortic Stenosis Post Module Evaluation Please place completed evaluation in an interdepartmental mail envelope and address to Dr. Wendy Gerstein, Department of Medicine, VAMC (111). 1) Topic of module:__________________________ 2) On a scale of 1-5, how effective was this module for learning this topic? _________ (1= not effective at all, 5 = extremely effective) 3) Were there any obvious errors, confusing data, or omissions? Please list/comment below: ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ 4) Was the attending involved in the teaching of this module? Yes/no (please circle). 5) Please provide any further comments/feedback about this module, or the inpatient curriculum in general: 6) Please circle one: Attending Resident (R2/R3) Intern Medical student