Transitions of Care - Heart Rhythm Society
advertisement
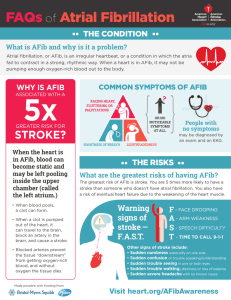
For the Mended Hearts Volunteer TRANSITIONS OF CARE ATRIAL FIBRILLATION TABLE OF CONTENTS • What is Atrial Fibrillation? • Transitions of Care? • Project Scope • The Role of the Care Provider • The Role of the Patient • Your Role • Resources • Feedback Survey 2 ATRIAL FIBRILLATION (AFIB) • Most commonly diagnosed arrhythmia disorder • 2.3 million people in U.S. living with AFib - 160,000 new cases annually • Patients with multiple chronic conditions can visit ~16 physicians annually • AFib is responsible for 88,000 deaths per year - $16 billion in health care costs • Challenge of coordinating basic information (e.g., test results, prescription medications, diagnosis) • Poor coordination often leads to adverse clinical outcomes, increased readmissions, overutilization of health care services, and untimely follow up 3 AFIB MYTHS • Myth: Heart rate and heart rhythm are the same thing • Fact: The rate and rhythm of your heart are different. Rate refers to the speed of your heart beat while rhythm is the pattern of the beat. AFib causes the heart to race and beat out of rhythm. • Myth: If I don’t feel any symptoms, my heart is beating in rhythm • Fact: Even if you do not experience symptoms, your heart may still beat out of rhythm. In fact, as many as 30 percent of people with AFib do not feel any symptoms. • Myth: As long as I am managing the stroke risk associated with AFib, it’s OK for my heart to stay out of rhythm • Fact: Managing your stroke risk treats just one of the serious consequences of AFib. As long as your heart remains out of rhythm, you will be at increased risk for permanent heart damage, heart failure, heart attack, stroke, and death. AFib is a complicated disease that can worsen over time. If your heart continues to beat out of rhythm, a process called “remodeling” can occur, changing the shape and size of your heart. A remodeled heart can become less efficient at pumping blood, making it work harder and harder over time. Heart remodeling is progressive and can become permanent. 4 AFIB MYTHS • Myth: Having AFib means I can no longer enjoy an active lifestyle • Fact: While some people with AFib are limited by their disease and symptoms, many can still lead an active lifestyle. Exercise is usually beneficial for someone with AFib because it has a positive effect on mood and can help keep weight controlled, which is good for the heart. It’s important to check diet, exercise, and other lifestyle habits, and discuss your personal AFib medical treatment plan with a health care provider. • Myth: AFib is an “old person’s” disease. • Fact: While AFib primarily affects people over the age of 65 and the risk of getting AFib increases as you age, it is important to recognize that AFib can be found in younger patients. As the “Baby Boomer” generation gets older, it’s estimated that 12 million Americans will have AFib by the year 2050. 5 TRANSITIONS OF CARE DEFINITION • Transitions of Care refers to the movement of patients between health care locations, providers, or different levels of care within the same location as their conditions and care needs change • Specifically, they can occur: • Within settings • Between settings • Across health states • Between providers 6 CARE COORDINATION DEFINITION • Care coordination is a function that helps ensure the patient’s needs and preferences for health services and information sharing across people, functions, and sites are met over time. Coordination maximizes the value of services delivered to patients by facilitating beneficial, efficient, safe, and high-quality patient experiences and improved health care outcomes 7 PRINCIPLES 1. 2. 3. 4. Care coordination is important for everyone Some populations are particularly vulnerable Care coordination measures may be appropriate at the clinician level; others may be appropriate at the group, practice, or organizational level Patient/family surveys are essential to measure care coordination; surveys performed within close time proximity to the health care event 8 ELEMENTS OF TRANSITIONS OF CARE • Medication reconciliation • Follow-up tests and services • Changes in plan of care • Involvement of team during hospitalization, discharge, follow up, etc. • Communication • Transfer of all information when site of care changes • Education of the patient and family 9 AFIB TRANSITIONS OF CARE GOAL Project Goal: • To develop practical resources to encourage best practices in clinical decision making, patientprovider communication, and patient selfmanagement 10 ROLE OF THE CARE PROVIDER • Engaging Mended Hearts Volunteers • Making a referral to post-ablation patients • Review Patient Care Pathway • • • Patient Care Plan Review Patient Discharge Checklist (provided in patient kits) Review AF Educational Resources (provided in patient kits) 11 ROLE OF THE PATIENT AND CAREGIVER • Understand the Patient Care Pathway Patient Care Plan • • Patient Discharge Checklist • • • And what is it and why is this important? And what is it and why is this important? Atrial Fibrillation Educational Resources 12 ROLE OF THE MENDED HEARTS VOLUNTEER • Understand the Patient Care Pathway Peer-to-peer patient support Patient Care Plan (No interpretation of orders/prescriptions) • • • Patient Discharge Checklist (General) • • • And what is it and why is this important? And what is it and why is this important? Atrial Fibrillation Educational Resources 13 PATIENT CARE PLAN • A plan of care is a written plan for services developed by the health care provider team to assess and determine the patient’s status and needs to ensure optimal outcomes for the patient MINIMUM CARE PLAN ELEMENTS • Patient’s routine needs/schedule • Tracking patient’s progress • • • • Weight Blood pressure Heart rate Other • Specific instructions regarding care after the procedure, including: • • • • • Medication guidelines Wound care Physical activity guidelines Post-procedure symptoms Follow-up schedule PATIENT DISCHARGE CHECKLIST • The hospital discharge is a complex process requiring integrated communications among the inpatient care team, primary care team, community services, and the patient and patient’s caregivers • The patient discharge checklist is intended as a tool to assist the patient and his/her caregiver(s) during the process to ensure a smooth and effective transition at discharge 16 DISCHARGE CHECKLIST Have a list of all medications Tell your doctors if you have any trouble affording or taking your medications Separate any medications that were stopped during the hospital stay Obtain a written description of potential side effects Know the time and date of your follow-up doctor appointments and lab/blood work. Make these before you leave the hospital Know/understand any restrictions on diet and exercise DISCHARGE CHECKLIST Continued Know what symptoms should prompt a call to your physician or a trip to the emergency department Know the phone number of the physician or health care provider to call in case of emergency Have a caregiver or designee also understand all discharge instructions and, if possible, have that person attend all doctor’s appointments Know when you can go back to work, if applicable Compile any questions you have for the health care provider PROVIDER/PATIENT KIT RESOURCES •Provider Resource Kit • Best practices • Patient care plan elements •Discharge checklist •Transition record checklist •Mended Hearts Info •Patient Resource Kit •Elements of a care plan •Patient discharge checklist •Role of the caregiver •Guide to AFib brochure •AFib Patient DVD •Mended Hearts Info 19 FEEDBACK SURVEYS • Care Provider • Web-based/monthly survey - 4 questions/feedback • Mended Hearts Volunteer • Telephone/Web-based surveys – Monthly/Quarterly • Patients • Postcard/Received during visit – 4 questions for 30 days post event 20 QUESTIONS? Thank You! 21