Atrial Fibrillation
Steve McGlynn
Specialist Principal Pharmacist (Cardiology),
Greater Glasgow and Clyde
Honorary Clinical Lecture,
University of Strathclyde
Some types of arrhythmia
Supraventricular
Sinus Nodal
Sinus bradycardia
Sinus tachycardia
Sinus arrhythmia
Atrial
Atrial tachycardia
Atrial flutter
Atrial fibrillation
AV Nodal
AVNSVT
Heart blocks
Junctional
Ventricular
Escape rhythms
Ventricular tachycardia
Ventricular fibrillation
Atrial fibrillation
A heart rhythm disorder (arrhythmia). It usually
involves a rapid heart rate, in which the upper heart
chambers (atria) are stimulated to contract in a very
disorganized and abnormal manner.
A type of supraventricular tachyarrhythmia
The most common arrhythmia
Aetiology
Rheumatic heart disease
Coronary heart disease
(MI)
Hypertension
Myopericarditis
Hypertrophic
cardiomyopathy
Cardiac surgery
Thyrotoxicosis
Infection
Alcohol abuse
Pulmonary embolism
Caffeine
Exercise
Lone AF
Incidence / Prevalence
1.7 / 1000 patients / year
3 / 1000 patients / year
(>60 years)
0.4 - 1% (overall)
2 – 4% (>60 years)
>8% (>80 years)
Classification
New / Recent onset
< 48 hours
Paroxysmal
variable duration
self terminating
Persistent
Non-self terminating
Cardiovertable
Permanent
Non-self terminating
Non-cardiovertable
Symptoms / Signs
Breathlessness /
dyspnoea
Palpitations
Syncope / dizziness
Chest discomfort
Stroke / TIA
6 x risk of CVA
2 x risk of death
18 x risk of CVA if
rheumatic heart disease
Irregularly irregular pulse
Atrial rate
300-600bpm
Ventricular rate depends
on degree of AV block
120-160bpm
Peripheral rate
slower (pulse deficit)
Investigations
Electrocardiogram (ECG)
All patients
May need ambulatory monitoring
Transthoracic echocardiogram (TTE)
Establish baseline
Identify structural heart disease
Risk stratification for anti-thrombotic therapy
Transoesophogeal echocardiography (TOE)
Further valve assessment
If TTE inconclusive / difficult
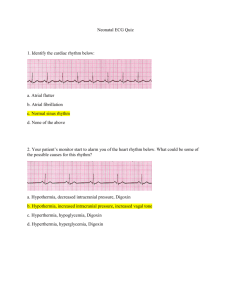
Normal Sinus Rhythm
‘Fast’ AF
‘Slow’ AF
Atrial Flutter
Investigations
Electrocardiogram (ECG)
All patients
May need ambulatory monitoring
Transthoracic echocardiogram (TTE)
Baseline
Structural heart disease
Risk stratification for anti-thrombotic therapy
Transoesophogeal echocardiography (TOE)
Further valve assessment
TTE inconclusive / difficult
Diagnosis
Based on:
ECG
Presentation
Response to treatment
Treatment objectives
Rhythm / rate control
Stroke prevention
Treatment strategies
New / Recent onset
Cardioversion
Rhythm control
Paroxysmal
Rate control or
cardioversion during
paroxysm
Rhythm control if
needed
Persistent
Cardioversion
Rhythm control
Peri-cardioversion
thromboprophylaxis
Permanent
Rate control
Thromboprophylaxis
Pharmacological Options
Class Ic Anti-arrhythmics
Flecainide / Propafenone
Rhythm control
May also be pro-arrhythmic
Class II Anti-arrhythmics
Beta-blockers
Mainly rate control
Control rate during exercise and at rest
Generally first choice
Choice depends on co-morbidities
Class III Anti-arryhthmics
Amiodarone / Dronedarone
Mainly rhythm control
May be pro-arrhythmic
Concerns over toxicity
Class IV Anti-arryhthmics
Calcium channel blockers (verapamil / diltiazem only)
Rate control only
Alternative to beta-blockers if no heart failure
Digoxin
Rate control only
Does not control rate during exercise
Third choice unless others contra-indicated
Acute AF
Treatment will depend on:
History of AF
Time to presentation (<> 24 hours)
Co-morbidities (CHD, CHF/LVSD etc)
Likelihood of success (History)
Rate Vs. Rhythm control
Rhythm control not feasible or safe
Beta-blocker
Verapamil
Digoxin (CHF)
Rhythm control if possible and safe
DC cardioversion (if possible)
Amiodarone (CHD or CHF/LVSD)
Flecainide (Paroxysmal AF)
Paroxymal AF
Rhythm control*
Antithrombotic therapy as
per risk assessment
Beta-blocker
Aspirin 75-300mg
Class 1c agent or sotalol
warfarin to INR 2-3
If CHD - sotalol
See later
If LVD: Amiodarone
Dronedarone?
*May be “Pill in the pocket”
Persistent AF
Rhythm control
Beta blocker
No structural heart
disease: Class 1c* or
sotalol
Structural heart
disease: amiodarone
Rate control
As for permanent AF
* not if CHD present
Antithrombotic therapy as
per risk assessment
Pre-cardioversion
thromboprophylaxis of at
least 3 weeks
If rate control, as for
permanent AF
Permanent AF
Beta blocker or
Antithrombotic therapy as per
risk assessment
Calcium channel blocker
and/or
Aspirin 75-300mg
Digoxin
Warfarin to INR 2-3
See later
Amiodarone?
Stroke prevention
(non-rheumatic AF)
Stroke Risk Assessment
(CHADS2)
C
H
A
D
S
Chronic Heart Failure (1 point)
Hypertension (1 point)
Age > 75 years (1 point)
Diabetes (1 point)
Stroke, TIA or systemic embolisation (2 points)
Score < 2: low risk, aspirin or anticoagulant
Score ≥ 2: high risk, anticoagulant indicated
Stroke Risk Assessment
(CHA2DS2VASc)
Alternative to CHADS2
C
H
A
D
S
V
A
Sc
Chronic Heart Failure (1 point)
Hypertension (1 point)
Age > 75 years (2 points)
Diabetes (1 point)
Stroke, TIA or systemic embolisation (2 points)
vascular disease (1 point)
Age 65-74 years (1 point)
Sex category (1 point if female)
Bleeding Risk Assessment
(HAS-BLED)
1 point each for:
Hypertension
Abnormal renal/liver function (1 for each)
Stroke
Bleeding history or predisposition
Labile INR
Elderly (age over 65)
Drugs*/alcohol** concomitantly (1 for each)
*Drugs that increase bleeding, e.g. aspirin
** Alcohol excess
Anticoagulants
Warfarin remains standard anticoagulant at present
3 new oral anticoagulants (unlicensed for AF as of June 2011)
Dabigatran (Direct thrombin inhibitor)
Rivaroxiban (Factor Xa inhibitor)
Apixaban (Factor Xa inhibitor)
Fixed doses
No monitoring
At least as effective as warfarin
Safer than warfarin?
Much more expensive (even allowing for INR costs)
Place in therapy not clear yet
Conclusions
AF is a common condition.
Patients may be unaware of its presence and are
therefore at risk of a stroke
Alternative treatment strategies exist to control
symptoms
Alternative treatment strategies exist to reduce the
risk of stroke
Patient education and choice are central to
improving the likelihood of treatment success