Traumatic Coma
advertisement

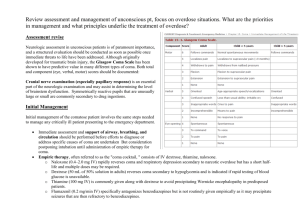
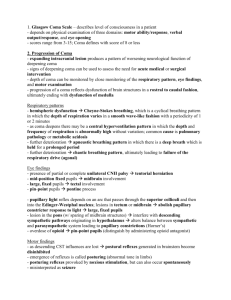
Decreased level of consciousness Ali Shoeibi MD, assistant professor of neurology, Mashhad University of Medical Sciences Consciousness State of awareness of self and surroundings Types • Level of arousal • Cognitive and affective function – dementia – delusions – Confusion – inattention APPROACH TO THE PATIENT IN COMA • Stabilize vital functions such as blood pressure and oxygenation (A,B,C) • Brief history & examination • I.V. line & sampling • Treat reversible causes of coma 1. supplemental oxygen 2. intravenous thiamine (at least 100 mg) 3. intravenous 50% dextrose in water (25 g) 4. Naloxone hydrochloride may be given parenterally, preferably intravenously, in doses of 0.4 to 2.0 mg APPROACH TO THE PATIENT IN COMA • Comprehensive history & examination • The neck should be stabilized in all instances of trauma until cervical spine fracture or subluxation can be ruled out • in unconscious patients with a history of trauma, peritoneal lavage by an experienced surgeon may be warranted Causes of Coma Causes of Coma More than half of all cases of coma are due to metabolic brain dysfunction (Almost half of these are drug poisonings) Differentiating Toxic-Metabolic Coma from Structural Coma • When the history is available, the patient's underlying illnesses and medications, or the setting in which they are found, often help guide the physician to the appropriate cause • The time course of the illness resulting in coma can be helpful. Generally, structural lesions have a more abrupt onset, whereas metabolic or toxic causes are more slowly progressive • The response to initial emergency therapy may help differentiate metabolic or toxic causes of coma • In general, structural lesions have focal features or at least notable asymmetry on neurological examination. Toxic, metabolic, and psychiatric diseases are characterized by their symmetry State of consciousness • Patients with metabolic problems often have milder alterations in arousal, typically with waxing and waning of the behavioral state • Patients with acute structural lesions tend to stay at the same level of arousal or progressively deteriorate • Toxins may also cause progressive decline in level of arousal Respiration Deep, frequent respiration most commonly is due to metabolic abnormalities, though rarely it is caused by pontine lesions or by neurogenic pulmonary edema secondary to acute structural lesions Funduscopic examination • Subhyaloid hemorrhage or papilledema are almost pathognomonic of structural lesions • Papilledema due to increased ICP may be indicative of an intracranial mass lesion or hypertensive encephalopathy • Papilledema does not occur in metabolic diseases except hypoparathyroidism, lead intoxication, and malignant hypertension Pupil size • The pupils usually are symmetrical in coma from toxicmetabolic causes. • Patients with metabolic or toxic encephalopathies often have small pupils with preserved reactivity. • Exceptions – methyl alcohol poisoning, which may produce dilated and unreactive pupils – late in the course of toxic or metabolic coma if hypoxia or other permanent brain damage has occurred. In terminal asphyxia the pupils dilate initially and then become fixed at midposition within 30 minutes Pupil reactivity • Pupillary reactivity is relatively resistant to metabolic insult and usually is spared in coma from drug intoxication or metabolic causes, even when other brainstem reflexes are absent. • Exceptions – Hypothermia may fix pupils – severe barbiturate intoxication may fix pupils – neuromuscular blocking agents produce midposition or small pupils – glutethimide and atropine dilate pupils common mistakes • the use of insufficient illumination • preexisting ocular or neurological injury may fix the pupils or result in pupillary asymmetry • Seizures may cause transient anisocoria • Local and systemic medications may affect pupillary function Pupil Size and Reactivity Ocular motility Asymmetry in oculomotor function typically is a feature of structural lesions Spontaneous and reflex eye movements • Roving eye movements with full excursion are most often indicative of metabolic or toxic abnormalities • Reflex eye movements normally are intact in toxic-metabolic coma • Exceptions: – rarely in phenobarbital or phenytoin intoxication – rarely deep metabolic coma from other causes Doll's eye phenomenon Muscle tone • Muscle tone usually is symmetrical and normal or decreased in metabolic coma • Structural lesions cause asymmetrical muscle tone. Tone may be increased,normal, or decreased by structural lesions • Any toxic-metabolic cause of coma may be associated with focal features; however, such features most often are observed with – – – – barbiturate or lead poisoning Hypoglycemia hepatic encephalopathy hyponatremia Differentiating Psychiatric Coma from Metabolic or Structural Coma • In the patient with true stupor or coma, passive eyelid opening is easily performed and is followed by slow, gradual eyelid closure. – The malingering or hysterical patient often gives active resistance to passive eye opening and may even hold the eyes tightly closed. – It is nearly impossible for the psychiatric or malingering patient to mimic the slow, gradual eyelid closure. • The pupils normally constrict in sleep or (eyes-closed-type) coma but dilate with the eyes closed in the awake state. Passive eye opening in a sleeping person or a truly comatose patient (if pupillary reflexes are spared) results in pupillary dilation. – Opening the eyes of an awake person produces constriction. Differentiating Psychiatric Coma from Metabolic or Structural Coma • Roving eye movements cannot be mimicked and thus also are a good sign of true coma • during cold caloric testing, the eyes do not tonically deviate to the side of the caloric instillation, and the fast phases are preserved, stupor or true coma is essentially ruled out • Blinking also increases in psychiatric and malingering patients but decreases in patients in true stupor. PROGNOSIS • outcome in any comatose patient cannot be predicted with 100% certainty unless that patient meets the criteria for brain death • subcategories: – drug-induced – Nontraumatic – traumatic coma • Drug-induced coma usually is reversible unless the patient has not had appropriate systemic support whiIe comatose and has sustained secondary injury from hypoperfusion, hypoxia, or lack of other necessary metabolic substrates Nontraumatic Coma • Only about 15% of patients in nontraumatic coma make a satisfactory recovery • Functional recovery is related to the cause of coma. – Diseases causing structural damage, such as cerebrovascular disease including subarachnoid hemorrhage, carry the worst prognosis – coma from hypoxia-ischemia due to such causes as cardiac arrest has an intermediate prognosis – coma due to hepatic encephalopathy and other metabolic causes has the best ultimate outcome • Age does not appear to be predictive of recovery • The longer a coma lasts, the less likely the patient is to regain independent functioning. Nontraumatic Coma • patients with nontraumatic coma who have not regained awareness by the end of 1 month are unlikely to do so. Even if they do regain consciousness, they have practically no chance of achieving an independent existence • poor neurological outcome: within 3 days of coma – The absence of pupillary light responses – The absence of motor responses to pain – low Glasgow Coma scores (less than 5) Traumatic Coma • The prognosis for traumatic coma differs from that for nontraumatic coma in many ways – First, many patients with head trauma are young – Second, prolonged coma of up to several months does not preclude a satisfactory outcome in traumatic coma – Third, in relationship to their initial degree of neurological abnormality, traumatic coma patients do better than nontraumatic coma patients Traumatic Coma • early predictors of the outcome of posttraumatic coma include – – – – patient's age motor response pupillary reactivity depth and duration of coma • The prognosis worsens with increasing age • little influence on the outcome – – – – Cause of injury skull fracture lateralization of damage to one hemisphere extracranial injury