Neurological Failure - CriticalCareMedicine
advertisement
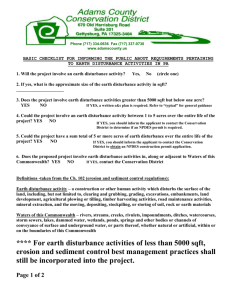
Neurological Failure 73 year old man is transferred to the ICU postop after emergency AAA surgery. He is hemodynamically stable. Two days later, he is weaning from the ventilator and the nurse calls you. The patient is fighting with the ventilator, thrashing about and hypertensive. When you arrive, he is trying to sit up and will not obey commands. He looks at you like you are the devil himself. This man clearly has an altered level of consciousness. What is the definition for delirium? Disturbance of consciousness with reduced ability to focus, sustain, or shift attention. A change in cognition or the development of a perceptual disturbance that is not better accounted for by a pre-existing, established, or evolving dementia. The disturbance develops over a short period of time (usually hours to days) and tends to fluctuate during the course of the day. There is evidence from the history, physical examination, or laboratory findings that the disturbance is caused by a medical condition, substance intoxication, or medication side effect. How is it different from coma? Coma is a clinical states in which patients have impaired responsiveness (or are unresponsive) to external stimulation and are either difficult to arouse or are unarouseable Coma is defined as "unarousable unresponsiveness" What is the differential diagnosis for delirium? Toxins Drugs: Prescription medications, polypharmacy Drugs of abuse including alcohol intoxication or withdrawal, narcotics, cocaine, LSD, and phencyclidine Infection: sepsis, systemic infections Poisons: ethylene glycol, methanol, insecticides, carbon monoxide, etc. Metabolic derangements Electrolyte disturbance (elevated or depressed): sodium, calcium, magnesium, phosphate Endocrine disturbance (depressed or increased): thyroid, parathyroid, pancreas, pituitary, adrenal Hypercarbia Hyperglycemia and hypoglycemia Hyperosmolar and hypoosmolar states Hypoxemia Inborn errors of metabolism: porphyria, Wilson's disease, etc. Nutritional: Wernicke's encephalopathy, vitamin B12 deficiency, possibly folate and niacin deficiencies Brain disorders CNS infections: encephalitis, meningitis, brain or epidural abscess Epileptic seizures, especially nonconvulsive status epilepticus* Head injury* Hypertensive encephalopathy Psychiatric disorders* Systemic organ failure Cardiac failure Hematologic: thrombocytosis, hypereosinophilia, leukemic blast cell crisis, polycythemia Liver failure: acute, chronic Pulmonary disease, including hypercarbia and hypoxemia Renal failure: acute, chronic Physical disorders Burns Electrocution Hyperthermia Hypothermia Trauma: with systemic inflammatory response syndrome, *head injury, fat embolism What are some of the risk factors for the development of delirium? Consider: underlying brain diseases, polypharmacy, advanced age and sensory impairment How would you investigate this patient? What pharmacological and non-pharmacological treatments can be used to manage this patient? Later that day… A 50 year old man presents to the emergency department with the worse headache of his life. Over 30 minutes he becomes progressively obtunded to the point of coma. After intubation for airway control, he has a CT scan. What is the problem? What is the cause? How does it usually present? How is the diagnosis made? What treatments (supportive and definitive) are available? What complications can occur? Still later that day… A 50 year old man presents to the emergency department with the worse headache of his life. Over 30 minutes he becomes progressively obtunded to the point of coma. After intubation for airway control, he has a CT scan. What is the problem? What is the cause? How does it usually present? How is the diagnosis made? What treatments (supportive and definitive) are available? What complications can occur? At 2:30 in the morning… A 19 university student presents to the health centre with increasing confusion and headache over the last 24 hours. On examination, he has a blood pressure of 91/43, heart rate of 140, respiratory rate of 23, temperature of 40.1 and oxygen saturations of 89%. He is delirious and has a diffuse rash. What is the most concerning diagnosis on the differential? What treatments should be initiated immediately? What is the role for steroids in meningitis? What are the most common causative organisms? What other adjuvant treatment should be considered for this patient? Then your pager goes off (again)… You are call to the neurology ward for a 29 year old woman with a long history of temporal lobe epilepsy. She was admitted for EEG monitoring and planned surgery. Her medications have been stopped for four days. Upon your arrival, she has been having generalized tonic clonic seizures for 10 minutes. What are your immediate concerns? What is the definition of status epilepticus? Why is this an emergency? After 8 mg of ativan, she is still seizing. What do you do now? Describe the approach to the treatment of status epilepticus. Next is a STAT trauma call… 19 year old man is involved in a two car MVC. His GCS at the scene is 3 and he is intubated and resuscitated. Upon arrival in the trauma room, he is hemodynamically stable with no major injuries. He remains a GCS 3. He is taken urgently for CT head. Sidebar Identify the findings on the following CT scans Back to the case The patient is seen by the Neurosurgery service and they insert an intraventricular drain. He is then transferred to the ICU. What is the purpose of an intraventricular drain? What is the cerebral perfusion pressure? Describe the Monroe-Kelly doctrine, Later in the evening, the nurse calls you because the ICP is 45 for the last 20 minutes. What are some of the causes of intracranial hypertension? How would you emergently manage this problem? What is secondary injury and why is it important? Questions??