6-Staphylococci
advertisement

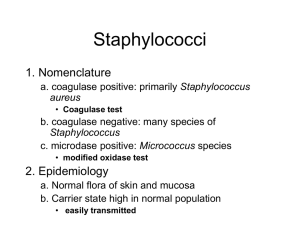
STAPHYLOCOCCI PROF AM KAMBAL Staphylococci Definition: Gram +ve cocci in clusters, catalase positive. Other gram positive cocci include Streptococci and Micrococci Differences between Staphylococci, Micrococci and Streptococci Character Staphylococci (& Micrococci) Streptococci Gram Stain Positive Positive Arrangement Clusters (Micrococci) in Fours) Chains Size Large 1 um Catalase Positive Smaller 0.5 – 1 um Negative H2O2 Catalase H2O + O2 Staphylococci are similar to Micrococci in shape But Staphylococci can be: a) Pathogenic b) Commensals (Normal Flora) c) Oxidative & fermentative While Micrococci are: a) Commensal (Normal flora of skin) b) Only oxidative (Non fermentative) Can be differentiated from Staphylococci by oxidation, fermentation reactions (O – F) test Gram Positive Cocci In Clusters Species : S.aureus : main pathogen S.epidermidis (S.albus) : opportunistic S.saprophyticus : UTI Laboratory Characteristics Morphology: Culture: ordinary media,aerobic/ non aerobic, positive catalase reaction. Colonies : S.aureus : golden yellow-white S.epidermidis : white, no pigment Both tolerate 5-10 % NaCL. Staphylococci are divided into two main groups: 1) Coagulase +ve i.e. Staphylococcus aureus 2) Coagulase negative a) Staphylococcus epidermidis b) Staphylococcus saprophyticus Differentiating Tests Coagulase test : main test S.aureus : coagulase positive S. epidermidis and albus : coagulase negative Two types of coagulase tests: Tube coagulase Slide coagulase Coagulase Test A) Enzyme secreted by Staphylococcus aureus. B) Differentiate between Staphylococcus aureus and other Staphylococci C) Coagulates Plasma Fibrinogen to Fibrin in clot form D) Tested By: 1. 2. Slide test for bound coagulase or clumping factor Tube test free coagulase test Other Tests DNAse test Phosphatase test Mannitol fermentation Novobiocin sensitivity to differentiate between S.epid. and S. saproph. which is resistant Staphylococci are divided into two main groups: 1) Coagulase +ve i.e. Staphylococcus aureus 2) Coagulase negative a) Staphylococcus epidermidis b) Staphylococcus saprophyticus Habitat Staph. aureus Staph. epidermidis Certain areas of skin All skin surface (see diagram) Colour Mainly golden yellow (on Blood agar) Catalase +ve White (on Blood agar medium) +ve (Continued) Staph aureus Staph epidermidis Coagulase Dnase +ve +ve -ve -ve Phosphalase +ve -ve Growth on Mannitol salt agar due to fermentation of mannitol Yellow Red Phage typing available Groups I, II, III Not available Staphylococcus aureus Carried by 20 – 50 % of healthy people on the skin mainly in a. Nose b. Axilla c. Perineum d. Throat e. Gut Human Staphylococcal Species most important are: Species Frequency Coagulase of Infection Production Common Human Habitat S. aureus Common Positive Anterior nares, perineum S. epidermidis Common Negative Anterior nares, head, axilla, arms and legs S.saprophyticus Common Negative Urinary tract Species Frequency of infection Other species are: Coagulase production Common Human habitat S. hemolyticus Uncommon Negative Axilla, pubes (apocrine glands) Axilla, pubes (apocrine glands) - S. hominis Uncommon Negative S. simulans Uncommon Negative S. auricularis Rare Negative S. capitis Rare Negative S. cobnii Rare Negative S. saccharolyticus Rare Negative - S. warneri Rare Negative - S. xylosis Rare Negative - Ear canal Scalp, forehead (sebaceous gland) - Virulence Factors: A. Toxins and toxic components produced by Staphylococcus aureus Toxins Activity Haemolysins a, B, y and - Cytolytic, lyse erythrocytes of various animal species Coagulase Fibronolysin Leucoccidin Hyaluronidase DNAase Clots Plasma Digests fibrin Kills leucocytes Breaks down hyaluronic acid Hydrolysis DNA Virulence Factors: (Continued) Toxins Activity Lipase Lipolytic (produces opacity in egg-yolk medium) Antiphagocytic Epidermal splitting and exfoliation Protein A Epidermolytic toxins A and B Enterotoxin(s) Toxic shock syndrome toxin - 1 Causes vomiting and diarrhoea Shock, rash, desquamation B. Other virulence factors include: 1. 2. Peptidoglycan of the cell wall Teichoic acid Pathogenecity Or Infections Caused By: Staph. aureus 1) Superficial Infection 1. Pustules 2. Boils 3. Carbuncles 4. Impetigo 5. Collection of pus 6. Abscesses 7. Wound infection (Hospital Acquired) 8. Paronychia – Infection of nail bud 2) Skin Exfoliation Toxic epidermal necrocysis S.S.S.S. = Staphylococcus Scalded Skin Syndrome 3) Deep Infections Septicaemia, Endocarditis Pyaemia Osteomyelitis – Infection of bone Pneumonia 4) Food Poisoning Due to an enterotoxin produced in the food before ingestion. An intoxication not infection 5) Toxic Shock Syndrome 1l – 1 = Interlukin I TNF = Tumour necrosis factor Treatment: Drain Pus if any + Antibiotics Antibiotic Sensitivity (Staphylococcus aureus) Penicillin 95% ®: if sensitive, it is the best drug Flu/Cloxacillin (Methicillin) Drug of choice Fucidic Acidpenetrate well in bones Vancomycin if the organism is resist to methicillin (MRSA) 5. Erythromycin 6. Clindamycin 7. Rifampicin 1. 2. 3. 4. MRSA = Methicillin Resistant Staphylococcus aureus MRSA: Also Resistant to Cloxacillin & Flucloxacillin Treatment For MRSA = Vancomycin Treatment of Staphylococcus aureus 95% Resistant to Penicillin so treated by Cloxacillin if Resistant to Cloxacillin or Methicillin = MRSA = so treat with Vancomycin. MRSA = Methicillin Resistant Staphylococcus aureus MRSA: Also Resistant to Cloxacillin & Flucloxacillin Treatment For MRSA = Vancomycin Treatment of Staphylococcus aureus 95% Resistant to Penicillin so treated by Cloxacillin if Resistant to Cloxacillin or Methicillin = MRSA = so treat with Vancomycin. M.R.S.A Methicillin and cloxacillin resistant S.aureus. Due to mec A gene which codes for PBP 2a with low affinity to beta lactam antibiotics nosocomial infections. Treatment: vancomycin for systemic infections only. B) Staphylococcus saprophiticus It causes urinary tract infection in young female. Coagulase Negative Staphylococci (it is novobiocin resistant) The commonest coagulase negative is: Staph. epidermidis Pathogenesis: They produce very small amounts of toxins. Pathogenesis is mainly due to production of (slime) which consists of: a. Polysaccharide b. Techoic acid enhanced by presence of fibrinogen. This makes them sticky on biomaterial like catheters. Sticky material called is Biofilm. They Cause: 1. 2. 3. 4. 5. 6. 7. 8. Endocarditis in artificial valves “shunts”. Infections of spitz holter valves connecting brain ventricle with jugular vein Infection of cannulae Infection of Intravenous catheters Infections of prosthesis e.g. Artificial valves (heart) Orthopaedic fixing nails Infection in premature babies (Bacteriaemia) Infection in Oncology patients Staphylococcus saprophyticus causes urinary infection in young females Treatment of Coagulase Negative Staphylococci “Staphylococcus epidermidis” and others : Depends on testing antibiotics sensitivity on the isolates But Vancomycin is the drug of choice for severe serious infection