S. aureus - Pathology
advertisement

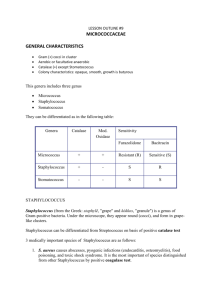
Staphylococci 1. Nomenclature a. coagulase positive: primarily Staphylococcus aureus • Coagulase test b. coagulase negative: many species of Staphylococcus c. microdase positive: Micrococcus species • modified oxidase test 2. Epidemiology a. Normal flora of skin and mucosa b. Carrier state high in normal population • easily transmitted 3. Pathogenesis a. localized skin infections • follicles, boils, furuncles, carbuncles Furuncle Carbuncle http://dermatology.about.com/od/infectionbacteria/tp/bacterial_infections.htm 3. Pathogenesis b. toxin mediated diseases • • • • Enterotoxin: food poisoning Exfoliatin: scalded skin syndrome TSST-1: toxic shock syndrome Pantone-Valentine Leukocidin? 3. Pathogenesis c. systemic infections • all species: bacteremia • S. saprophyticus: UTI • Central Nervous System (CNS): indwelling devices (catheters, valves, hardware, shunts) d. antimicrobial resistance • Methicillin Resistant Staphylococcus aureus (MRSA) – nosocomial v. community (PVL as marker?) – screening programs to detect colonization in hospitalized patients • Vancomycin Intermediate Staphylococcus aureus (VISA) – thicker cell wall, grow poorly, vanco less active • VRSA – vancomycin resistant – MRSA acquire plasmids containing van genes from Vanco resistant enterococci (VRE) Streptococci 1. Nomenclature a. Hemolytic criteria: alpha, beta, gamma b. Lancefield group carbohydrates for betahemolytic streptococci: A, B, C, F, G c. some beta-hemolytic streptococci produce identical carbohydrate antigens in unrelated species, and some genetically related species have heterogeneous carbohydrate antigens 2. Epidemiology a. normal flora of skin, mucosa (upper respiratory tract, GU tract, GI tract) b. disease can be due to person-person transmission or from endogenous strains 3. Pathogenesis a. S. pyogenes i. Group A, beta-hemolytic ii. acute pharyngitis, skin infections, bacteremia with potential for severe systemic effects – toxic shock syndrome, necrotizing faciitis (“flesh-eating” disease) iii. many toxins, enzymes, M protein which are all virulence factors iv. post infection sequelae: Rheumatic fever, acute glomerulonephritis (AGN) • reason for treating strep throat is to prevent these b. S. agalactiae i. Group B, beta-hemolytic ii. neonatal infections following PROM early onset (day 0 – 5) late onset (day 7 – 90) iii. screening of pregnant women at week 3537 c. S. pneumoniae i. alpha hemolytic ii. pneumonia, meningitis, and otitis media iii. capsule has antiphagocytic activity 23 valent polysaccharide vaccine for adults 7 valent conjugated vaccine for kids c. Enterococcus i. alpha, beta, or gamma hemolytic ii. most infections are nosocomial: UTI, bacteremia, endocarditis iii. multi-drug resistance contributes to pathogenesis; penicillins, aminoglycosides, glycopeptides E. faecalis, vanA, vanB (plasmid, inducible) E. faecium, vanA, vanB (plasmid) E. gallinarum, vanC (chromosome) E. casseliflavus, vanC (chromosome) d. Viridans streptococci and Abiotrophia sp. i. normal skin flora; non-pathogens ii. endocarditis in compromised hosts iii. alpha hemolytic iv. Abiotrophia show satelliting C. Identification algorithms 1. Gram stain: pairs, chains, clusters 2. Direct antigen detection a. GAS from throat b. Pneumococcus from CSF or blood cultures 3. Selective media a. SSA for GAS from throat b. GBS broth + Grenada agar 4. catalase a. positive: coagulase i. positive: CPS (S. aureus) ii. negative: CNS Yellow pigment: Micrococcus high numbers in urine, screen for Staphylococcus saprophyticus using novobiocin (R = S. saprophyticus) b. negative: hemolysis i. beta: typing: A, B, C, D, F streptolysin O, S CAMP test for GBS ii. alpha: optochin sensitive: S. pneumoniae resistant: Alpha-hemolytic streptococci iii. gamma: PYR positive: Enterococcus motile: E. casseliflavus or E. gallinarum non-motile: biochems for E. faecalis or E. faecium negative: Gamma-hemolytic streptococci Staphylococcus sp. on Gram stain http://www.bact.wisc.edu/Microtextbook/modules.php?op=modload&name=Sections&file= index&req=viewarticle&artid=35&page=1 S. aureus, beta-hemolytic S. aureus, gold colonies Coagulase-negative Staphylococci Micrococcus sp., yellow colonies MRSA chromogenic agar Streptococcus sp. on Gram stain http://www.life.umd.edu/classroom/bsci424/PathogenDescriptions/StreptococcusImages.htm GBS GAS Alpha-hemolytic S. pneumoniae CAMP positive GBS Optichin-sensitive S. pneumoniae Satelliting of Abiotrophia S. agalactiae (GBS) on Grenada agar D. Susceptibility testing 1. Staphylococcus sp. a. resistance in multiple classes b. usually test all S. aureus; test Coag Neg Staph if appropriate c. VITEK, disk diffusion or broth dilution d. inducible clinda resistance 2. GAS, GBS a. not resistant to pen, ceph, vanco b. resistance to macrolides, so test if considering use c. disk diffusion or broth dilution d. inducible clinda resistance in GBS D. Susceptibility testing 3. S. pneumoniae a. resistance to pen, ceph, macrolides b. VITEK, disk diffusion or broth dilution c. different interpretive criteria for CNS v. non-CNS infections 4. Enterococcus a. usually use cell wall active agent plus aminoglycoside to achieve sufficient bactericidal activity b. resistance to all clinically useful agents has been documented c. test using broth dilution, including high level resistance to aminoglycosides (VITEK) 5. other strep (not routine)