staph
advertisement

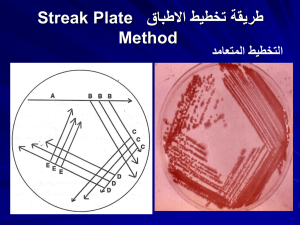
Dr.wasan sami shukur Gram positive cocci There are two medically important genera of gram positive cocci: Staphylococcus and Streptococcus. Staphylococcal infections range from the trivial to the rapidly fatal. They can very difficult to treat, especially those contracted in hospitals, because of the remarkable ability of Staphylococci to become resistant to antibiotics. Staphylococci are ubiquitous in nature, with about a dozen species occurring as a part of human flora. The most virulent of the genus, S.aureus , is one of the most common causes of bacterial infections Staphylococci & Streptococci are non motile & do not form spores. Both Staphylococci & Streptococci are gram positive cocci, but they are distinguished by two main criteria. *Microscoplly, Staphylococci appear in grape-like clusters, whereas Streptococci are in chains. *Biochemically, Staph .produce catalase (ie, they degrade hydrogen peroxide), whereas Streptococci do not. General features of Staphylococci Staphylococci generally stain darkely gram positive, they are round &tend to occur in bunches like grapes. They are true facultatively anaerobic org. They produce catalase. The most virulent spp. of Staphylococcus is S.aureus, almost all isolates of which secrete coagulase-an enzyme that causes citrated plasma to clot. There are other spp. that occasionally cause disease; these lack coagulase & are often referred to as coagulase negative Staphylococci Staphylococcus aureus S.aureus disease may be: *Largely or wholly the result of actual invasive infection (that is, colonization), overcoming host defense mechanisms, & the production of extracellular substances which facilitate invasion. *A result of toxins in the absence of invasive infection. or *A combination of invasive infection and intoxication. Epidemiology S.aureus is frequently carried by healthy individuals on the skin & mucous membranes. Carriers serve as a source of infection themselves & others; ex, by direct contact, by contamination of fomites or food, which can then result in food poisoning. Pathogensis S.aureus causes disease by infecting tissues typically creating abscesses and/or by producing toxins. A common entry point into the body is a break in the skin. Another portal of entry is the respiratory tract. The localized host response to Staphylococcal infection is inflammation, characterized by swelling, accumulation of pus, and necrosis of tissue. Fibroblasts and their products may form a wall around the inflamed area, which contains bacteria & leukocytes. This creates a characteristic, pusfilled boil or abscess. Serious consequences of staphylococcal infections occur when the bacteria invade the bloodstream. The resulting septicemia may be rapidly fatal. Bacteremia may result in seeding internal abscesses, skin lesions, or infections in the lung , kidney, heart, skeletal muscle, or meninges. Pathogenic virulence factors are the genetic, biochemical, or structural features that enable an organism to produce disease. The clinical outcome of an infection depends on the virulence of the pathogen and the opposing effectiveness of the host defense mechanisms. S.aureus produce many enzymes include coagulase, fibrinolysin, hyaluronidase, proteases, nucleases, & lipases Also these orgs expresses many potential virulence factors as follows: 1-Cell wall virulence factors a) Protein A is a major component of the S.aureus cell wall. It binds to the Fc moiety of IgG, exerting an antiopsonin( and therefore strongly antiphagocytic) effect. b) Fibronectin-binding protein (FnBP) and other staphylococcal surface proteins promote binding to mucosal cells and tissue matrices. 2-Cytolytic exotoxins: α, β, γ, and δ toxins attack mammalian cell (including red blood cell) membranes, and are often referred to as hemolysins. 3-Superantigen exotoxins: These toxins have affinity for the T cell receptor-MHC Class II antigen complex. They stimulate enhanced T lymphocyte response. This major T cell activation can cause toxic shock syndrome, primarily by release into the circulation of inordinately large amounts of T cell cytokines, such as interleukin-2 (IL-2), interferon- γ (IFN- γ), and tumor necrosis factor- α (TNF- α). a-Enterotoxins: Enterotoxins (six major antigenic types: A, B, C, D, E, and G) are produced by approximately half of all S.aureus isolates. When these bacteria contaminate food and are allowed to grow, they secrete enterotoxin, ingestion of which can cause food poisoning. Enterotoxins are superantigens that are even more heat stable than S.aureus; therefore, organisms are not always recovered from incriminated food b- Toxic shock syndrome toxin (TSST-1) is the classic cause of toxic shock syndrome. Because of similarities in molecular structure, it is sometimes referred to as staphylococcal enterotoxin F (SEF), although it does not cause food poisoning when ingested. c-Exfoliatin (exfoliative toxin, ET) is also a superantigen. It causes scalded skin syndrome in children Clinical findings The important clinical manifestations caused by S.aureus can be divided into two groups: inflammatory & toxin-mediated. 1-Inflammatory Skin infections, such as impetigo, furuncles, carbuncles, folliculitis…..etc. Septicemia can originate from any localized lesion, especially wound infection, or as a result of intravenous drug abuse. Endocarditis on normal or prosthetic heart valves. Osteomyelitis and arthritis Pneumonia in postoperative patients or following viral respiratory infection. Abscesses can occur in any organ when the organism circulates in the bloodstream (bacteremia). Toxin-mediated Food poisoning caused by ingestion of enterotoxin, which is performed in foods & hence has a short incubation period (1-8 hours). Toxic shock syndrome is characterized by high fever, hypotension, rash, vomiting, diarrhea & multiorgan involvement (especially GI, renal, &/or hepatic damage). TSST causes toxic shock , especially in tampon-using menstruating women or in individualswith wound infections. Toxic shock also occur in patients with nasal packing used to stop bleeding from the nose. TSST is produced locally by S.aureus in either the vagina, nose, or other infected site. The toxin enters the bloodstream, causing a toxemia. Scalded skin syndrome is characterized by fever, large bullae resulting from the action of an exfoliative toxin that attacks the intracellular adhesive of the stratum granulosum causing marked epithelial desequamation.This syndrome occurs most often in young children Lab. Diagnosis Specimen: There are to be collected depending on the nature of lesion, pus from suppurative lesions, CSF from meningitis, blood from septicemia, sputum from respiratory infection and suspected food, vomit or faeces from food poisoning. Smear: Examination of gram stained smear of pus & other specimens shows gram positive cocci in clusters with some single & paired cocci. Culture : Specimens inoculated on blood agar or mannitol agar (selective media for Staph.aureus show typical colonies on 18 hr incubation at 37 Cْْ . Coagulase test: the coagulase positive strain is identified . Typing test. Coagulase negative staphylococci There are two coagulase negative staphylococci of medical importance: S.epidermidis & S. saprophyticus. S.epidermidis infections are almost always hospital acquired, whereas S. saprophyticus infections are almost always community- acquired. S.epidermidis is part of the normal human flora on the skin & mucous membranes but can cause infections of intravenous catheters & prosthetic implants, eg, heart valves (endocarditis), vascular grafts, & joints. S.epidermidis is also a major cause of sepsis in neonates & of peritonitis in patients with renal failure who are undergoing peritoneal dialysis through an indwelling catheter. It is the most common bacterium to cause cerebrospinal fluid shunt infections S.epidermidis produces an extracellular polysaccharide material (sometimes called"slime") that facilitates adherence to bioprosthetic material surfaces, such as intravenous catheters, & acts as a barrier to antimicrobial agents. S. saprophyticus causes urinary tract infections, particularly in sexually active young women. Lab. Diagnosis Specimen: There are to be collected depending on the nature of lesion, pus from suppurative lesions, CSF from meningitis, blood from septicemia, sputum from respiratory infection and suspected food, vomit or faeces from food poisoning. Smear: Examination of gram stained smear of pus & other specimens shows gram positive cocci in clusters with some single & paired cocci. Culture : Specimens inoculated on blood agar or mannitol agar (selective media for Staph.aureus show typical colonies on 18 hr incubation at 37 Cْْ . Coagulase test: the coagulase positive strain is identified . Typing test. Differential properties of some Staphylococcal species Species Frequency Coagulase Color of of disease colonies S.aureus common + Golden,yellow S.epidermidis common white S. occasional variable saprophyticus Mannitol fermentation + - Novobiocin resistant +