Choledochoduodenostomy - VCU Department of Surgery
advertisement

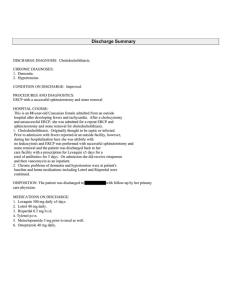
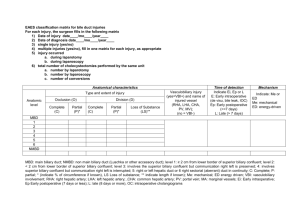
Choledochoduodenostomy 3/5/15 COMPLICATION, 3/2/15 Faculty/Resident: Bittner/Kaplan/Uchiyama Diagnosis: Choledocholithiasis Procedures: 2/16/15: Open common bile duct exploration, choledochoduodenostomy, lysis of adhesions, upper endoscopy 3/2/15: Incision and drainage of deep abdominal wound infection Other Involved Services: Interventional radiology, Internal medicine Complication: Wound infection Outcome: Resolution of wound infection after I&D BACKGROUND H&P: 84 yr old female presented to General Surgery ACC clinic on 1/13/2015 after hospitalization at Community Memorial Hospital (12/29/2014) with weakness, dizziness, itchiness & 18lb weight loss over previous 2 months. CMH labs: Elevated bilirubin, AST, ALT, ALP BACKGROUND PMHx: Atrial fibrillation, CVA, uncontrolled essential hypertension, Raynaud’s phenomenon, hyperlipidemia PSHx: Open roux-en-y gastric bypass (1980), open cholecystectomy, total abdominal hysterectomy, laparoscopic ovarian cystectomy, total knee replacement, breast reduction Family Hx: Heart disease, HTN Social Hx: Denied tobacco, drug or alcohol use. Medications: Amlodipine, Carvedilol, B12. dicyclomine, Pepcid, hydroxyzine, Losartan/HCTZ BACKGROUND PHYSICAL EXAM (from clinic visit 1/13/15): Gen: Thin 84 yr old female, NAD HEENT: Sclera non-icteric Lungs: CTAB Heart: RRR Abdomen: Soft, non-tender/non-distended, old well healed vertical midline incision & right subcostal Kocher incision, no palpable masses or hernias BACKGROUND CT A/P (w/o IV contrast, CMH) BACKGROUND CT A/P (w/o IV contrast, CMH) BACKGROUND RUQ US (1/5/15, VCU) BACKGROUND RUQ US (1/5/15, VCU) BACKGROUND RUQ US (1/5/15, VCU) BACKGROUND MRCP (1/20/15, VCU) BACKGROUND MRCP (1/20/15, VCU) BACKGROUND IR (1/27/15, VCU) - PTC tube placement BACKGROUND Operative Course: 2/16/15: Exploratory laparotomy, lysis of adhesions, open common bile duct exploration, choledochoduodenostomy, upper endoscopy Intraoperative bile cultures: VRE (E. faecalis) Postop Course: 2/18/15: Epidural removed 2/20/15: Discharged to rehab facility 2/27/15: PTC tube studied & removed by IR BACKGROUND IR (2/27/15, VCU) - PTC removed BACKGROUND Operative Course: 2/16/15: Exploratory laparotomy, lysis of adhesions, open common bile duct exploration, choledochoduodenostomy, upper endoscopy Intraoperative bile cultures: VRE (E. faecalis) Postop Course: 2/18/15: Epidural removed 2/20/15: Discharged to rehab facility 2/27/15: PTC tube studied & removed by IR 3/1/15: Sent from rehab facility to ED with incisional drainage, leukocytosis 3/2/15: Incision and drainage of deep abdominal wound infection, cultures positive for E. Faecium (VRE) ASSESSMENT Clavien-Dindo Classification FISHBONE PRE-OP POST-OP 1. Bile duct obstruction/cholangitis 2. Bile duct instrumentation (PTC) 3. Recent weight loss/poor nutrition 1. ?Extended postoperative antibiotic coverage 2. 3. OUTCOME 1. Peri-operative antibiotic selection 1. Wound infection 2. Case length >2 hours 3. INTRA/PERI-OP PATIENT SPECIFIC FACTORS: Age, Patient comorbidities – HTN, HLD, Atrial Fibrillation 4 minutes INDICATION FOR OPERATION • Primary common duct stone formation as a late complication after cholecystectomy with failed stone extraction DISCUSSION 1. Primary common bile duct stone formation after cholecystectomy 2. Choledochoduodenostomy PRIMARY CBD STONE FORMATION AFTER CHOLECYSTECTOMY • Primary CBD stone formation years after cholecystectomy associated with bile stasis, cholangitis, foreign bodies • Multiple publications from 1897-present cite suture material as the nidus for stone formation • Other foreign bodies attributed to stone formation mentioned in literature: shrapnel, buck shot, wire fragments, vegetable residue, fish bone, surgical clips PRIMARY CBD STONE FORMATION AFTER CHOLECYSTECTOMY • Cameron et al (Annals of Surgery, 1977) published results of a series of patients after cholecystectomy with primary CBD stones who underwent CBDE from 1952-75 – Previous cholecystectomy ± CBD exploration with 2 year asymptomatic period postoperatively without evidence of long cystic duct remnant or strictures – Morphologically soft, crushable, light brown stones/sludge in CBD • Pathogenesis not completely clear (Dilated ducts after cholecystectomy → Stasis → Stone Formation) PRIMARY CBD STONE FORMATION AFTER CHOLECYSTECTOMY • GI literature quotes CBD stone clearance rate exceeds 90% with ERCP/sphincteroplasty • Recurrence of CBD stones in patients treated with ERCP not uncommon • Management of patients in which duct is unable to be cleared or with recurrent primary choledocholithiasis – – – – Repeat ERCP Choledochoduodenostomy Choledochojejunostomy Transduodenal sphincteroplasty CHOLEDOCHODUODENOSTOMY • First published experience with CDD was by R.L Sanders & presented at the 57th Southern Surgical Association, 1945 – 25 patients (15 survived >6 months with “good” results) – Side-to-side anastomosis performed – Descried important of dilated CBD to achieve optimal outcome • Only 2 large case series were published in the subsequent 20 years by Schwartz (1959) & Madden (1965) – General consensus that it is critical for CBD to measure at least 15mm in diameter for success Side-to-Side Technique Mastery of Surgery, 6th Edition End-to-Side Technique Scientific American Surgery, 2014 CHOLEDOCHODUODENOSTOMY • Advantages: – No need for construction of roux limb or additional anastomosis (JJ) – No potential for internal hernia compared with hepatojejunostomy – Side-to-side choledochoduodenal anastomosis avoids the issue of a residual unretrievable distal stone – Requires less enterolysis/mobilization in patients with adhesive disease & portal hypertension – Facilitates subsequent endoscopic interventions CHOLEDOCHODUODENOSTOMY • Disadvantages – Two feared complications: Cholangitis & sump/blind sac syndrome (published incidence 0.5-9.6%) • Pathogenesis of cholangitis related to reflux of pancreatic secretions and bacteria (function of sphincter of Oddi) • Chronic relapsing cholangitis possibly related to late development of cholangiocarcinoma – Not ideal for palliative management of malignant causes of bile duct obstruction Conclusions • Foreign bodies & stasis are a nidus for primary CBD stone formation after cholecystectomy • ERCP/sphinterotomy is effective and ideal for sick/elderly patients but papillary restenosis may occur • If endoscopically inaccessible, PTC tube placement and stone retrieval is an option • Options for surgical management include CDD, HJS, transduodenal sphincterotomy • Major complications of CDD include cholangitis, sump syndrome Nonoperative dilatation, performed either endoscopically or percutaneously, can be used successfully to manage which of the following causes of bile duct stricture? A. Oriental cholangiohepatitis. B. Distal bile duct stricture due to chronic pancreatitisIncorrect. C. Complete transection of the bile duct during laparoscopic cholecystectomy (the so-called "classic" laparoscopic cholecystectomy injury) D. Postoperative bile duct stricture following hepaticojejunostomy for reconstruction during a Whipple procedure Answer: D • Nonoperative management of bile duct strictures is an option in many cases of biliary strictures; however, this approach has technical limitations because of the anatomic or clinical situation. In the so-called "laparoscopic bile duct injury," complete bile duct transection and discontinuity of the biliary tree eliminates the possibility of nonoperative management. Percutaneous dilatation of biliary enteric anastomosis has been shown in a number of series to have a success rate approaching that of surgical reconstruction. Oriental cholangiohepatitis is an unusual infection of the biliary tree frequently associated with infection by Clonorchis sinensis and other parasites. Cholangiography shows numerous strictures of the intrahepatic and extrahepatic biliary tree and bile ducts filled with sludge and stones. Surgical management consisting of cholecystectomy and improving biliary drainage by means of a Roux-en-Y choledochojejunostomy or choledochoduodenostomy is necessary for almost all patients. There has been limited experience with the role of balloon dilatation of distal bile duct stricture secondary to chronic pancreatitis with little long-term follow-up. The length of the stricture as well as the chronic associated fibrosis caused by pancreatitis makes this option less attractive. Compared with endoscopic sphincterotomy, transduodenal sphincteroplasty is associated with which of the following? A. Decreased incidence of restenosis B. Improved symptomatic relief C. Shorter length of hospitalization D. Ability to perform concomitant diagnostic evaluation E. Increased incidence of pancreatitis Answer: A When properly performed, transduodenal sphincteroplasty results in decreased incidence of restenosis when compared with endoscopic treatments. Which of the following statements is true concerning bile duct strictures caused by chronic pancreatitis? A. The course of untreated bile duct stricture caused by chronic pancreatitis is usually benign and not progressive. B. Most patients present with marked jaundice. C. Serum bilirubin is the most sensitive laboratory finding in diagnosing bile duct strictures caused by chronic pancreatitis. D. Common bile duct strictures can be expected to develop in almost 50% of patients with alcohol-induced chronic pancreatitis. E. A suitable option for surgical management is choledochoduodenostomy. Answer: E • Chronic pancreatitis is an uncommon cause of benign bile duct strictures (<10% of cases). The clinical problem in chronic pancreatitis is a distal bile duct obstruction resulting from inflammation and parenchymal fibrosis of the gland. These strictures classically involve the entire intrapancreatic segment of the common bile duct and are associated with dilatation of the entire proximal biliary tree. In most cases the cause of chronic pancreatitis is alcoholism. Common bile duct strictures have been reported to occur in 3% to 29% of patients with chronic alcoholic pancreatitis. In a review of a number of clinical studies, the overall incidence of common bile duct strictures in patients with chronic pancreatitis was 5.7%. The clinical presentation of patients with common bile strictures secondary to chronic pancreatitis is variable. Some patients have no symptoms, and the diagnosis of bile duct stricture is suggested only by abnormal liver function test results. The serum alkaline phosphatase appears to be the most sensitive laboratory finding and is elevated in more than 80% of patients. Indications for surgical management of common bile duct strictures caused by chronic pancreatitis are clear in patients with significant pain, jaundice, or cholangitis. In general, biliary bypass, either as a Roux-en-Y hepaticojejunostomy or a choledochoduodenostomy, is indicated in patients who are asymptomatic with persistent elevation of serum alkaline phosphatase because changes from obstructive biliary cirrhosis have been observed in patients with long-standing, functionally significant biliary obstruction caused by chronic pancreatitis. A 70-year-old woman presents with fever, right upper quadrant abdominal pain, jaundice, hypotension, and mental status changes. Labs demonstrate leukocytosis, a direct of 3.5 mg/dL, and elevated transaminases in the presence of a normal amylase and lipase assay. Abdominal ultrasonography shows a common bile duct diameter of 1.5 cm. In addition to ICU admission, fluid resuscitation, and the initiation of antibiotics, the most appropriate intervention for this patient is: A. Endoscopic retrograde cholangiopancreatography (ERCP) with stone extraction and sphincterotomy B. Percutaneous transhepatic cholangiography (PTC) and drain placement C. Open common bile duct exploration with extraction of stones D. Choledochoenterostomy E. Biliary t-tube placement Answer: A This patient clinically has “Reynolds’ pentad” and is in septic shock from cholangitis. In addition to resuscitation and initiation of antibiotics, source control is absolutely necessary. The preferred management strategy with the least morbidity would be ERCP with stone extraction and sphincterotomy. Open common bile duct exploration, choledochoenterostomy, and biliary t-tube placement require laparotomy which would impart a higher morbidity upon this patient, but may be necessary if gastroenterology is unable to perform an ERCP for this patient. PTC drainage is an alternative to ERCP but does not remove the obstructing stone. A 63-year-old woman has severe jaundice and back pain. She has been losing weight for three months. Workup reveals obstructive jaundice secondary to a distal common bile duct tumor. Among the following, the preoperative laboratory test most likely to be abnormal is: A. Prothrombin time (PT) B. Serum potassium C. Serum bicarbonate D. Partial thromboplastin time (PTT) E. Carcinoembryonic antigen (CEA) Answer: A Among the laboratory tests listed, prolongation of the prothrombin time (PT) is most characteristic of patients with severe obstructive jaundice of long standing. Biliary obstruction deprives the duodenum and small intestine of the bile necessary for the formation of micelles. Micelles have a hydrophilic external environment and a hydrophobic core and are essential for aiding fat digestion (by increasing the available surface area for enzymatic activity), as well as for absorption of the fat soluble vitamins A, D, E, and K. Vitamin K is a necessary cofactor for hepatic synthesis of prothrombin, and factors VII, IX, and X. Continuing vitamin K deficiency will eventually be manifested as an elevation in the PT. Which of the following statements regarding elective repair of a bile duct stricture is true? A. End-to-end bile duct anastomosis is an appropriate option. B. Stenting for approximately 1 year is necessary for an anastomosis performed at the distal common bile duct. C. Preoperatively placed biliary catheters facilitate dissection and identification of the injury and facilitate reconstruction. D. A transanastomotic stent is necessary for a successful result. Answer: C Several principles are associated with successful repair of a biliary injury or stricture: (a) exposure of healthy proximal bile ducts that provide drainage to the entire liver; (b) preparation of a suitable segment of intestine that can be brought to the area of the stricture without tension, most frequently a Roux-en-Y jejunal limb; and (c) a creation of a direct biliary-enteric mucosal-to-mucosal anastomosis. The choice of procedure is dictated by the location of the stricture, the history of previous unsuccessful attempts at repair, and the surgeon's personal preference. Simple excision of a bile duct stricture and end-to-end bile duct anastomosis or repair of the damaged duct can rarely be accomplished because of the invariable loss of duct length as a result of fibrosis associated with the injury. Thus, in almost all cases, hepaticojejunostomy constructed to a Roux-en-Y limb of jejunum is the preferred procedure. Many surgeons believe that a transanastomotic stent is helpful in almost all cases. A number of series, however, have had successful results without the use of such stents. The use of preoperatively placed percutaneous catheters facilitates the identification of the proximal biliary segment, which can be difficult because of retraction high into the porta. The catheters also facilitate mobilization and the anastomotic technique including the placement of Silastic (Dow Corning, Midland, MI) biliary catheters. The length of stenting depends on the location of the stricture. If the stricture involves the common bile duct or common hepatic duct at least 2 cm distal to the hepatic duct bifurcation and adequate proximal bile duct mucosa can be identified, the use of longterm biliary stenting is not necessary. In these situations, transanastomotic stenting for 4 to 6 weeks after the operation is adequate. A longer period of stenting is necessary if adequate proximal bile duct is not available or if a good mucosal-tomucosal anastomosis cannot be completed.