Biopsychology of Psychiatric Disorders
advertisement

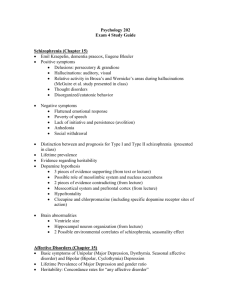
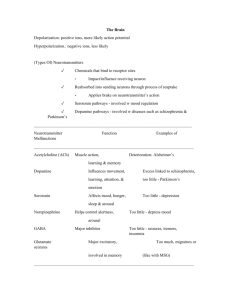
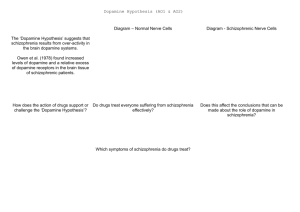
Biopsychology of Psychiatric Disorders Ch. 18 (cont’d) Outline • Schizophrenia (cont’d) – Dopamine Theory of Schizophrenia • Affective Disorders – – – – Symptoms and Etiology Antidepressant Drugs Monoamine Theory of Depression Diathesis Model of Depression Dopamine Theory of Schizophrenia • Side effects of chlorpromazine and reserpine are mild tremors at rest, muscular rigidity, and a decrease in voluntary movement Dopamine Theory of Schizophrenia • These side effects are the same as the symptoms of Parkinson’s Disease • Thus, neurochemical changes that were the basis of these drug’s antischizophrenic action were related to pathology underlying Parkinson’s symptoms Dopamine Theory of Schizophrenia • Parkinson’s disease is associated with dopamine deficiency • It seemed that chlorpromazine and reserpine reduced brain dopamine levels • And reduction of dopamine was alleviating schizophrenia symptoms Dopamine Theory of Schizophrenia • On the basis of these two inferences it was proposed that schizophrenia is associated with excessive activity in the dopaminergic systems in the brain Dopamine Theory of Schizophrenia • Two previous findings lent additional support to the dopamine theory of schizophrenia: Dopamine Theory of Schizophrenia – Reserpine was known to be a dopamine antagonist (it depleted the brain of dopamine by causing them to leak from their vessicles) – Stimulants, which are agonists of dopamine trigger schizophrenic episodes in healthy subjects at high doses (cocaine psychosis and amphetamine psychosis) Dopamine Theory of Schizophrenia • Additional research clarified that although chlorprozamine is a antagonist like reserpine, left dopamine levels unchanged; • Rather it acts as a false transmitter chlorpromazine acts like dopamine and is received by dopaminergic membrane receptors (antagonistic) Dopamine Theory of Schizophrenia • More than one type of dopaminergic receptor; total of five types • Found that antischizophrenic drug haloperidol binds to D2 only; while chlorpromazine binds to both D1 and D2 Dopamine Theory of Schizophrenia • Dopamine theory of schizophrenia is revised; schizophrenia can now be viewed as caused by excess activity at D2 receptors and thus alleviated by drugs that block activity at D2 receptors Dopamine Theory of Schizophrenia • Four questions about this theory that have yet to be resolved: Four questions about DTS • Are D2 receptors the only ones involved in schizophrenia? – The effectiveness of clozapine, which binds poorly to D2 receptors yet binds to serotonin receptors suggest that serotonin receptors may be involved in schizophrenia Four questions about DTS • Why does it take several weeks for neuroleptics to work? – The therapeutic effect of blockade is mediated by neural adaptation (slow compensatory changes) to the blockade of dopamine receptors, rather than by the blockade itself Four questions about DTS – One hypothesis is that prolonged neuroleptic treatment eventually produces depolarization blockade in dopamine neurons, and it is this decrease in activity that is related to the drug’s therapeutic effect Four questions about DTS • What parts of the brain are involved in schizophrenia? – Imaging studies have revealed many changes, including small cerebral cortices and large ventricles Four questions about DTS – The cortical abnormalities are most prevalent in the prefrontal (organization of thoughts), cingulate (emotion), and temporal (auditory stimui) cortices Four questions about DTS – Some evidence that schizophrenia is a neurodevelopmental disorder; there is no obvious ongoing degeneration in the brain of schizophrenic patients, and the pathology is observed in largely developed by the time diagnosis is first made Four questions about DTS • Why are neuroleptics effective against only some of the symptoms of schizophrenia? – current hypothesis is that: • Cases with positive symptoms (hallucinations, delusions, incoherence) are caused by excess D2 activity and are helped • Negative symptoms (catatonia, blunt affect, poverty of speech) are due to permanent brain damage and cannot be helped Schizophrenia • Video shown in class – Individuals affected with Schizophrenia – Cell migration and aggregation hypothesis Affective Disorders • Individuals in whom sadness and apathy is so severe and frequent that it interferes with functioning are said to be suffering from the psychiatric disorder of depression • The opposite of this is mania Symptoms of Depression • Intense feelings of despair, hypoactivity, sleep problems, withdrawal, lack of appetite, and lack of hygiene Symptoms of Mania • Individuals are overconfident, impulsive, distractible, and highly energetic Symptoms of Affective Disorders • Bipolar affective illness - suffer from mania and depression • Unipolar affective illness - suffer from depression Etiology of Affective Disorders • Genetic basis - concordance rate for bipolar for identical twins is 60%; 15% for fraternal twins • Depression can be reactive (stress from negative experience) or endogenous (no apparent external triggers) Etiology of Affective Disorders • Some indication that early exposure to stress increases the likelihood of developing depression in adulthood Antidepressant Drugs • Monamine Oxidase Inhibitors (MAO inhibitors) increase level of monoamines (norepinephrine and serontonin) by stopping activity of enzymes that break down monoamine neurotransmitters in the presynaptic cell (before they are released) (agonistic) • For unipolar affective disorder Antidepressant Drugs • Tricyclic Antidepressants block the reuptake of both serontonin and norepinephrine (agonistic) • For unipolar affective disorder Antidepressant Drugs • Lithium is a metalic ion • Used to treat bipolar affective disorder Antidepressant Drugs • Selective Monoamine-Reuptake Inhibitors block reuptake of a specific monoamine NTs (agonist; unipolar affective disorder) – Selective serotonin-reuptake inhibitors (SSRIs) such as Prozac, Paxil, Xoloft, Luvox, Remeron – Selective norepinephrine-reuptake inhibitors (SNRIs) such as Reboxetine – Drugs that block more than one type are Wellbutrin and Effexor Theories of Depression • Monoamine Theory of Depression • Diathesis - Stress Theory of Depression Monoamine Theory of Depression • Most widely accepted theory • Based on fact that all clinically effective drugs are serotonin and/or norepinephrine agonists; • Thus depression may be due to underactivity at serontonin and norepinephrine synapses Monoamine Theory of Depression • In support of this theory, there is evidence that certain norepinephrine and serotonin receptors are elevated in untreated depressed patients; this may be due to low levels of transmitters eliciting a compensatory increase in receptors called receptor up-regulation Monoamine Theory of Depression • However, this theory cannot explain why monoamine antidepressants take 3 or more weeks to take effect although they immediately increase extracellular monoamine leels or why serotonin and norepinephrine agonists are equally effective Diathesis-Stress Theory of Depression • Based on idea that an individual inherits a diathesis (genetic predisposition) for depression; if the individual is stressed early in life their systems become altered so that they are hypersensitive to stress the rest of their lives • This leads to development of depression