Immune System Overview
advertisement

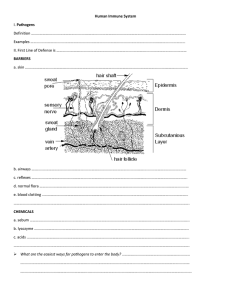
Why an immune system? We are outnumbered! Viruses and bacteria are everywhere! Humans offer limitless resources for pathogens Energy Reproductive potential Getting into the body isn’t easy! Meet the enemy Bacteria Free-living Not all are bad! Pathogenic ones produce toxins that damage human tissue Viruses Obligate parasites Hijack human cells; convert to virus-producers, killing host cell in the process (And fungi, protozoa too…) A human fortress Skin is thick – hard to penetrate Produces substances that deter invasion: Skin pH (not favorable) Mucus (sticky trap) Lysozymes (digest bacteria) Specialized traps around vulnerable areas (Eyes, noes, mouth) Cilia sweep away invaders that are trapped Stomach acid kills ingested invaders …but we do get sick! Enter through weak points: Food Nose Break in skin/scrapes Cells are damaged/destroyed Dying cells release distress chemicals (histamine) Triggers inflammation (blood vessel dilation, increased blood flow) Draws defensive cells to area (generalized white blood cells) How do we tell “friend” from “foe”? All cells present antigens – surface molecules that identify identity (antigen = antibody generator) Immune system reacts to foreign antigens A complex system! Several “lines” of defense: 1. Barriers (First line of defense) 2. Generalized defenders (Second line of defense) 3. Specific defenders AND memory (Third line of defense) Consist of: Several types of cells Proteins The Complement System Part of second line of defense Free-flowing proteins found in blood Quickly reach site of invasion React to antigens When activated, can Trigger inflammation Attract “eater cells” (macrophages) Coat pathogen (make macrophages’ job easier) Kill intruder directly Phagocytes Find and “eat” bacteria, viruses, dead/injured body cells by phagocytosis 3 types: Granulocytes (some) Macrophages Dendritic cells Granulocytes Often first to site of infection Numerous Short lifespan “Pus” in infected wounds chiefly composed of granulocytes Macrophage “Big eaters” Slower to respond to invader than granulocyte Larger, longer-lived, more capable Help alert rest of immune system to invader Start as monocytes; become macrophages when entering bloodstream Dendritic cells “Eater” cells Help with immune system activation – act as antigen- presenting cells Filter bodily fluids to clear foreign organisms and particles rd 3 Line of Defense: Humoral/Fluids Cell-Mediated Focus: catch invader before Deals with infection that has infection of cells Includes Antibodies to deactivate/eliminate threat in bodily fluids already entered cells Focus: destruction of infected cells so it doesn’t spread! Lymphocytes – Part of both humoral and cell-mediated T and B cells Originate in bone marrow Migrate to lymph nodes, spleen, thymus to mature Lymph vessels transport, store lymphocytes Feeds cells into body Filter out dead cells/invading organisms Receptors Each lymphatic cell contains surface receptors Recognize foreign antigens as cells pass by… Specialized for a particular antigen T cells – Cell-mediated immunity Primary focus = infected cells Two types: helper and killer T = thymus (site of maturation) Helper T cell Main regulator of third line of defense Primary task: activate other cells (B and killer T cells) Usually activated by macrophages/dendritic cells (during antigen presentation) Killer T cell Directly attacks body cells infected by pathogen, cancer cells Receptors used to determine if each cell encountered is self/non-self (compare to accepted receptors, MHC) B lymphocyte cell – Humoral immunity Searches for intact antigens matching receptor If a match is found… Connects to antigen Triggering signal set off… T helper proteins help fully activate B cell Produces 1000’s of clones: differentiate into plasma cells or B memory cells Plasma Cell Produces antibodies Responds to same antigen matched by B cell receptor Seek out intruders, help destroy them Release tens of thousands/second Antibodies Y-shaped Attach to matching antigens Enhance phagocytosis of macrophages (label for capture) Neutralize toxins Incapacitate viruses (coat surface proteins) Group pathogens by linking (agglutination) 5 types of antibodies (Ig’s): Most common; fight bacterial infections; pass from mom to IgG child in placenta (G = mom’s gift) In mucous membranes of digestive system, milk, tears, saliva IgA (A = a lot of mucus) Natural defenses against general bacterial infections (M=most IgM bacteria) Stimulate basophils and mast cells to defend against parasites IgE fungi and worms (E=eeeww!) On membranes of B-lymphocytes; form plasma and memory IgD cells (D=defend blood) Memory cells Prolonged lifespan “Remember” specific intruders Both B and T cells have memory cells Helps trigger immune system to respond more quickly if invader reappears Inflammation Outcome of secondary immune response Increases blood flow to affected area Blood vessels dilate to increase blood flow Immune cells go to affected area Immune response takes place at the site it’s needed Tissues = red and swollen because of the blood that enters the area; increasing temperature = antimicrobial Pain from pressure of swollen tissues on nerve endings Normal functions return when the tissue is fully recovered Immunization and Vaccination Natural Immunity Natural: exposed to foreign antigens as part of everyday life Acquired immunity – body responds to foreign antigens and develops immunity using B and T lymphocytes Passive immunity Embryological development when antibodies (Ig’s) from the mother’s blood stream are passed to the fetus Post-natal – baby receives antibodies via milk Artificial Immunity Active: Vaccinations Therapeutic exposure to antigens Stimulates the secondary response by introducing pathogenic material (inactivated, attenuated, or partial) into the body Vaccines are typically used for viruses! Antibiotics are only for bacteria Passive: Antibody transfer Patient receives (via injection) large amounts of antibodies to fight disease Globulin injections can remove certain microorganisms from the body